Abstract
Revascularization of coronary artery stenosis should be based on the objective evidence of ischemia. It is common practice for physicians to make decisions on revascularization in the cardiac catheterization laboratory based on the results of angiography, despite the fact that angiographic information does not correlate well with the functional significance of a coronary lesion. Fractional flow reserve (FFR) is a physiologic parameter which can be measured easily during the invasive procedure and can assess the functional significance of coronary stenosis. FFR-guided revascularization strategy is reported to be more effective than angiography-guided strategy in patients with coronary artery disease. Moreover, novel technologies based on FFR have been developed and will soon be incorporated into clinical practice.
Keywords: Coronary artery disease; Fractional flow reserve, myocardiol; Ischemia
Introduction
The presence of myocardial ischemia causes various symptoms in patients and is predictive of future events1),2) and revascularization of those lesions is important since it has the potential to improve patient outcomes.2-4) However, revascularization of stenotic lesions that do not lead to myocardial ischemia is not beneficial and can rather be harmful. Therefore, the decision to revascularize a coronary artery stenosis should be guided by the evidence of myocardial ischemia.
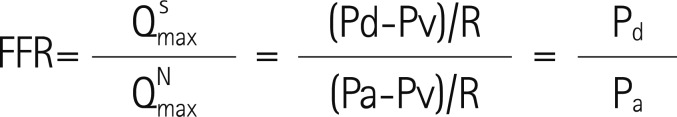
Coronary angiography is limited in its ability to determine the physiologic significance of coronary stenosis.5),6) Especially in patients with intermediate stenosis, angiographic information does not correlate well with the functional significance of a lesion.7-9) This uncertainty may result in unnecessary revascularization of insignificant lesions or failure to revascularize the clinically significant ones. As a result, fractional flow reserve (FFR) was introduced and has proven to be a reliable method for determining the functional significance of coronary stenosis. FFR expresses the maximal achievable blood flow in a coronary vessel as a fraction of normal maximal blood flow to the same myocardial territory.10) In other words, FFR represents the extent to which maximal myocardial blood flow is limited by the presence of epicardial stenosis and can be easily measured by the ratio of distal coronary pressure to aortic pressure during maximum hyperemia (Fig. 1). This index is independent of changes in hemodynamic conditions such as systemic blood pressure, heart rate, or myocardial contractility.11) As the clinical benefit of an FFR-guided revascularization strategy has been proven in several studies with different lesion subsets, this strategy has become more popular in recent years (Fig. 2).
Fig. 1.
The concept of fractional flow reserve (FFR).  : hyperemic myocardial blood flow in the presence of a stenosis,
: hyperemic myocardial blood flow in the presence of a stenosis,  : normal hyperemic myocardial blood flow, Pd: distal coronary pressure, Pa: aortic pressure, Pv: venous pressure, R: hyperemic myocardial resistance.
: normal hyperemic myocardial blood flow, Pd: distal coronary pressure, Pa: aortic pressure, Pv: venous pressure, R: hyperemic myocardial resistance.
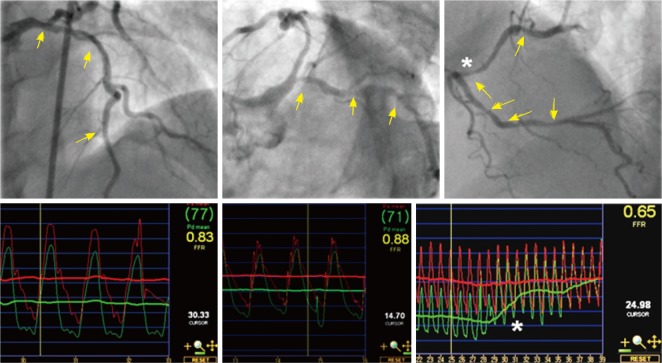
Fig. 2.
Clinical application of FFR to a patient with multiple lesions and multi-vessel disease. By coronary angiography, 11 stenoses (arrow) were found, yet none of those in the left anterior descending and left circumflex arteries were functionally significant by FFR. FFR values measured in the right coronary artery was FFR 0.65 and pullback pressure tracing revealed the lesion at the mid right coronary artery (*) was hemodynamically the most significant stenosis. After one stent implantation at the mid right coronary artery, the FFR was 0.81. FFR: fractional flow reserve.
Fractional Flow Reserve: The Past
In the very early period of percutaneous coronary intervention (PCI), clinical application of intracoronary pressure was tried in patients with coronary artery stenosis but failed. However, the cause of failure at that time was due to the fact that intracoronary pressure was measured with a large over-the-wire balloon catheter without hyperemia (minimal microvascular resistance). Since then, clinical application of intracoronary pressure had been almost forgotten until the concept of myocardial FFR was developed and introduced by N. Pijls and B. De Bruyne in the early 1990s.
The concept was first validated in an animal study12) and later in humans using a positron emission tomography scan.13) Given that FFR is a continuous variable, a certain cutoff value was necessary to determine the presence of myocardial ischemia (dichotomous variable). In 1996, Pijls et al.10) performed a clinical study to define the cutoff value of FFR to determine the presence of ischemia using non-invasive tests and sequential Bayesian considerations. In this study, an FFR cutoff value of 0.75 had a positive predictive value of 100% and a negative predictive value of 88% to determine the presence of ischemia. Due to a small zone of uncertainty between 0.75 and 0.80 (grey zone) and the results of the FFR versus Angiography for Multivessel Evaluation (FAME) study,3) many clinicians now use the FFR cutoff value of 0.80 as a guide to perform revascularization.
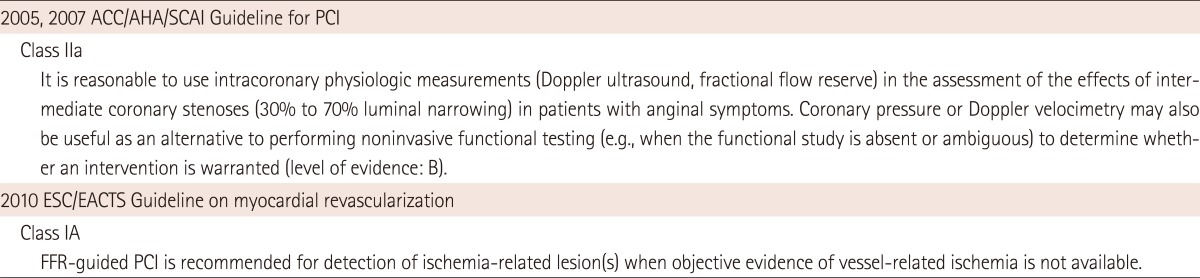
After validation of a cutoff value, the clinical benefit of FFR-guided revascularization was tested in the DEFER study (FFR to Determine the Appropriateness of Angioplasty in Moderate Coronary Stenoses).4) This study included 325 patients referred for PCI of a single, de novo stenosis of intermediate severity. PCI was performed in all patients with an FFR <0.75 (reference group, n=144). If the FFR was ≥0.75, patients were randomized to either medical treatment (defer group, n=91) or PCI (perform group, n=90). After 5 years of follow-up, event free survival did not differ between the defer and PCI groups (80% and 73%, respectively) and the percentage of patients free from chest pain at follow-up was not different between the 2 groups. The composite rate of death and acute myocardial infarction (MI) in the defer group was only 3.3% during the period of 5 years. This study showed that patient outcomes with deferral of PCI according to FFR was excellent and the risk of death or acute MI was <1% per year which could not be further decreased by stenting. Since then, the benefit of FFR-guided revascularization strategy was tested and confirmed in more complex scenarios involving multiple lesions, multivessel disease, in-stent restenosis, post-stenting, left main disease, bifurcation lesions and patients with MI.14-19) These results culminated in a Class IIA recommendation of FFR in 2007 American College of Cardiology/American Heart Association Society for Cardiac Angiography and Interventions PCI Guidelines on myocardial revascularization: "It is reasonable to use intracoronary physiologic measurements (Doppler ultrasound, fractional flow reserve) in the assessment of the effects of intermediate coronary stenoses in patients with angina symptoms" (Table 1).20)
Table 1.
Guidelines on FFR-guided revascularization strategy
FFR: fractional flow reserve, ACC/AHA/SCAI: American College of Cardiology/American Heart Association Society for Cardiac Angiography and Interventions, PCI: percutaneous coronary intervention, ESC/EACTS: European Society of Cardiology/European Association of Cardio-Thoracic Surgery
Fractional Flow Reserve: The Present
A nuclear substudy of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation trial showed that PCI could improve the outcome of patients with coronary artery disease (CAD) which resulted in the relief of myocardial ischemia.2) Investigators of the FAME study addressed the hypothesis that an FFR-guided PCI approach with drug-eluting stents would be superior to the current practice of conventional angiography-guided PCI in patients with multivessel CAD. The FAME protocol directed the investigators to stent a lesion with at least 50% stenosis and if the investigators thought that stenting was warranted on the basis of available clinical information. The patients were then randomized 1 : 1 to either standard PCI as planned (n=496) or to FFR-guided PCI (n=509). Although the number of angiographically significant stenoses was identical between the 2 groups (2.7±0.9 vs. 2.8±1.0), the FFR group used fewer stents per patient (1.9±1.3 vs. 2.7±1.2, p<0.001) and less contrast medium (272 mL vs. 302 mL, p<0.001). More importantly, at 1-year follow-up, the FFR group had fewer total cli-nical events (13.2% vs. 18.4%, p=0.02) and fewer combined death or MI (7.3% vs. 11%, p=0.04) compared to the angiography-guided PCI group. At 2 years, the rate of combined mortality or MI was still in favor of the FFR group (8.4% vs. 12.9%, p=0.02).21) Further analysis showed that an FFR-guided strategy is not only cost-effective but also cost-saving compared to an angiography-guided strategy.22) Another important finding of the FAME study is that assessment by FFR in patients with multivessel disease can lead to a reduction in the number of diseased coronary arteries and change in the treatment strategy. Of all patients with angiographic triple vessel disease (VD) in the FFR group, only 14% of the patients had functionally significant triple VD and 86% had ≤2 functionally significant diseased coronary arteries (2-VD=43%, 1-VD=34%, 0-VD=9%).8) Furthermore, the functional SYNTAX score (SYNTAX score only by ischemia-inducing lesions as determined by FFR) was shown to decrease the number of high-risk patients and better discriminate the risk for future adverse events in patients with multivessel CAD.23)
With the results of FAME study and its substudies, the FFR-guided revascularization strategy has become more popular and was classified as a Class IA recommendation in the 2010 European Guidelines on myocardial revascularization (Table 1).24)
Fractional Flow Reserve: The Future
Although FFR has become the gold standard invasive assessment to detect the ischemia-related lesion, it requires an invasive procedure, expensive devices and pharmacologic intervention to induce maximal hyperemia. Therefore, further development is still necessary to expand the clinical applications of FFR.
Novel hyperemic stimuli
Continuous infusion of adenosine via the central vein has been considered as the gold-standard method of hyperemia for FFR measurement.25) However, this method requires relatively large doses of adenosine resulting in high cost, an additional procedure for femoral vein access and is practically not feasible during transradial coronary catheterization procedures. Furthermore, the adenosine administration itself is associated with adverse systemic effects such as AV block, dyspnea and chest pain.26),27)
To overcome the complexity of central vein infusion of adenosine, the feasibility and efficacy of peripheral infusion of adenosine were tested in recent studies.28),29) Seo et al.29) compared the hyperemic efficacy between continuous IV infusion (140 µg/min/kg) via the femoral vein and the forearm vein and found that the hyperemic efficacy of the forearm vein infusion (FFR: 0.80±0.11) was not inferior (p for non-inferiority=0.01) to the femoral vein infusion (FFR: 0.80±0.10) of adenosine. The number of functionally significant stenoses was not different between the 2 methods {femoral vein vs. forearm vein; 17 (25.0%) vs. 17 (25.0%), p=1.0}. Therefore, this method can be used for FFR measurement, especially during transradial coronary catheterization procedures.
Novel hyperemic agents for invasive physiologic assessment were also introduced. Nair et al.30) compared the hyperemic efficacy between a selective A2A receptor antagonist, regadenoson (400 ug, IV bolus) and adenosine in 25 patients with intermediate coronary stenosis and found that a single IV bolus of regadenoson was as effective as an IV infusion of adenosine. Jang et al.31) compared the hyperemic efficacy of a bolus administration of nicorandil (intracoronary, 2 mg) with continuous infusion of adenosine in 210 patients. In this study, hyperemic efficacy of nicorandil was not inferior to that of adenosine (0.82±0.10 vs. 0.82±0.10; p for non-inferiority<0.001) and there was a strong linear correlation between the FFR measured by IV infusion of adenosine and nicorandil (R2=0.934). Moreover, nicorandil caused less changes in mean blood pressure, heart rate, PR interval and less severe chest pain than adenosine (p<0.05). While transient AV block occurred in 16 patients with adenosine, none were detected with nicorandil.
These novel agents and methods of adenosine administration will cause less discomfort in patients and reduce the complexity of invasive physiologic assessment.
Novel physiologic index without hyperemia
A new physiologic index, instantaneous wave-free ratio (iFR) without the requirement for hyperemia was introduced and tested in Adenosine Vasodilator Independent Stenosis Evaluation (ADVISE) study.32) From the meticulous investigation on coronary flow and resistance, the investigators found that there is a certain period in the cardiac cycle during which the resistance at rest is similar in variability and magnitude to those during hyperemia. In the ADVISE study, the distal-to-proximal pressure ratio during this period, which is also known as iFR, was compared with FFR in 157 stenoses. In this study, iFR had a good correlation with FFR (r=0.9, p<0.001) with excellent diagnostic performance (Fig. 3). This novel concept, iFR, has great appeal as it may provide a faster and easier invasive physiologic assessment for CAD. However, this concept still awaits further validation.
Fig. 3.
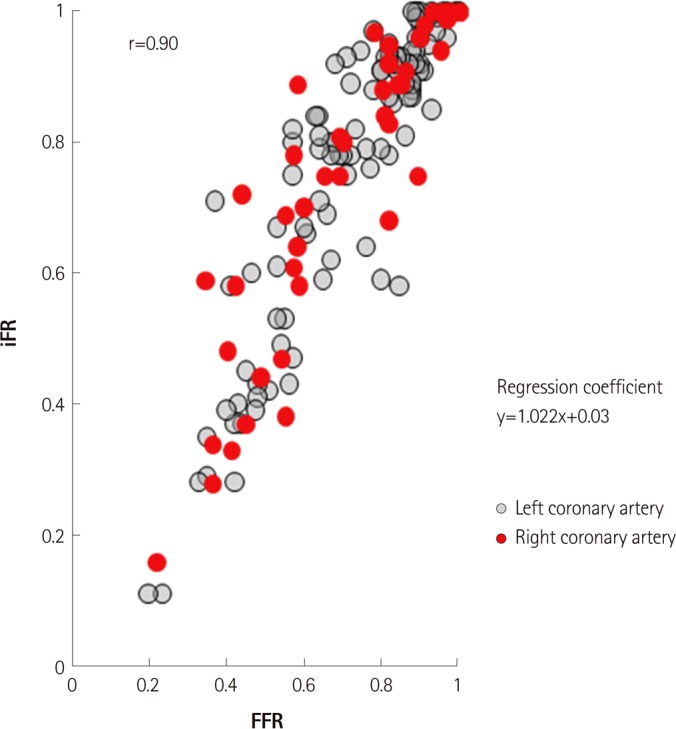
Correlation between iFR and FFR according to the coronary artery (data from ADVISE study, courtesy of Justin Davies, MD). iFR: instantaneous wave-free ratio, FFR: fractional flow reserve.
Non-invasive assessment of fractional flow reserve using CT scan
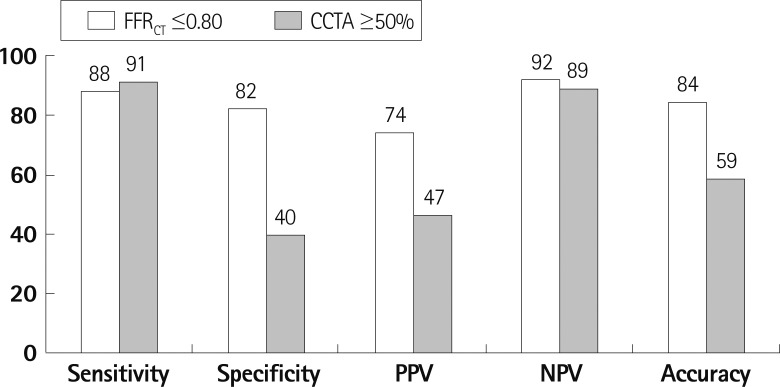
Recent advancements of CT technologies have enabled several novel methods to assess the functional significance of coronary stenosis in addition to anatomical information. One of these is the application of computational fluid dynamics to coronary CT angiography (CCTA) images.33) With this technology, FFR can be computed using images from conventional CCTA (CT-derived computed FFR; FFRCT) without any invasive procedure and without hyperemia (Fig. 4). A prospective, multicenter clinical trial, Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve (DISCOVER-FLOW) study, was performed to assess the diagnostic performance of FFRCT in the prediction of the functional significance of stenosis.34) In this study, 103 patients (159 vessels) with stenosis in a major epicardial coronary artery who had diagnostic quality CT images from 64 or more detector row CT scanners were consecutively enrolled and the diagnostic accuracy of CCTA (≥50% stenosis) and FFRCT were compared. On a per-vessel basis, accuracy, sensitivity, specificity, positive predictive value, and negative predictive value for FFRCT and CCTA were 84.3%, 87.9%, 82.2%, 73.9%, 92.2%, respectively, and 58.5%, 91.4%, 39.6%, 46.5%, 88.9%, respectively (Fig. 5). This study showed that noninvasive FFR derived from CCTA (FFRCT) had a high diagnostic performance for the detection and exclusion of coronary lesions that lead to ischemia. Clinical application of this novel technology may potentially reduce unnecessary invasive procedures. Moreover, combination of virtual intervention and this technology can help to determine the treatment strategy in complex lesions prior to the invasive procedure. Although the concept and results of the DISCOVER-FLOW study are very encouraging, further studies with a larger number of patients are needed to validate the clinical usefulness of this novel technology. A larger, prospective multicenter clinical trial, Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography study, has completed patient enrollment and the results will soon be available.35)
Fig. 4.
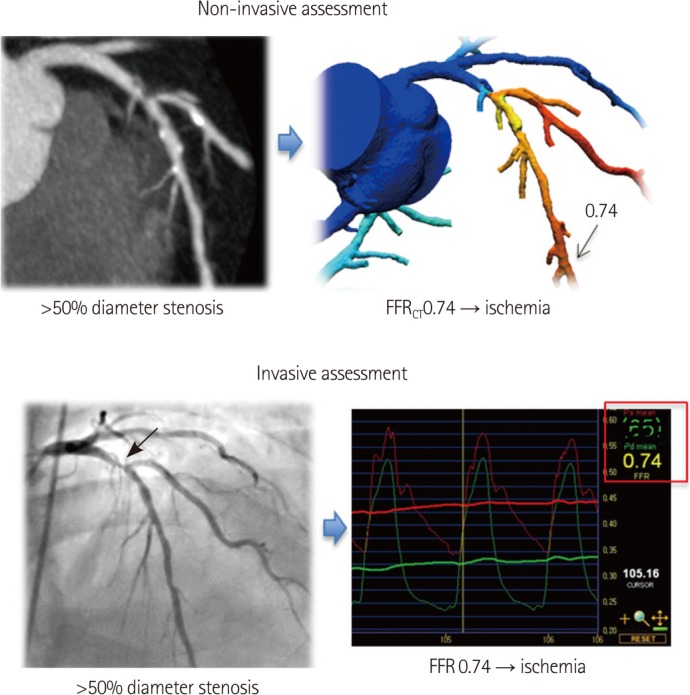
A case example of CT-derived computed FFR. By coronary CT angiography, significant stenosis was found at the proximal left anterior descending coronary artery. When this lesion was assessed by CT-derived computed FFR, FFRG was 0.74 and found to be functionally significant. This information derived from non-invasive assessment matched very well with invasive angiography and invasive FFR measurement (FFR=0.74). FFR: fractional flow reserve.
Fig. 5.
Comparison of the diagnostic performance between FFRCT and CCTA (from DISCOVER FLOW study, per-vessel analysis, n=159). PPV: positive predictive value, NPV: negative predictive value, FFRCT: CT-derived computed FFR, CCTA: coronary CT angiography, DISCOVER FLOW: Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve, FFR: fractional flow reserve.
Conclusion
Fractional flow reserve has become the gold standard to define the functional significance of coronary stenosis. Novel hyperemic stimuli and novel physiologic indices without hyperemia will reduce the barriers and expand the clinical application of FFR. Furthermore, non-invasive assessment of the functional significance of coronary stenosis such as CT-derived computed FFR, can be helpful in optimizing the interventional treatment strategy for patients with CAD prior to the invasive procedure.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–185. doi: 10.1016/j.nuclcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) Trial Nuclear Substudy. Circulation. 2008;117:1283–1291. doi: 10.1161/CIRCULATIONAHA.107.743963. [DOI] [PubMed] [Google Scholar]
- 3.Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–224. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 4.Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105–2111. doi: 10.1016/j.jacc.2007.01.087. [DOI] [PubMed] [Google Scholar]
- 5.White CW, Wright CB, Doty DB, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med. 1984;310:819–824. doi: 10.1056/NEJM198403293101304. [DOI] [PubMed] [Google Scholar]
- 6.Vogel RA. Assessing stenosis significance by coronary arteriography: are the best variables good enough? J Am Coll Cardiol. 1988;12:692–693. doi: 10.1016/s0735-1097(88)80058-5. [DOI] [PubMed] [Google Scholar]
- 7.Koo BK, Park KW, Kang HJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29:726–732. doi: 10.1093/eurheartj/ehn045. [DOI] [PubMed] [Google Scholar]
- 8.Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME Study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–2821. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- 9.Yong AS, Ng AC, Brieger D, Lowe HC, Ng MK, Kritharides L. Three-dimensional and two-dimensional quantitative coronary angiography, and their prediction of reduced fractional flow reserve. Eur Heart J. 2011;32:345–353. doi: 10.1093/eurheartj/ehq259. [DOI] [PubMed] [Google Scholar]
- 10.Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703–1708. doi: 10.1056/NEJM199606273342604. [DOI] [PubMed] [Google Scholar]
- 11.De Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans: feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996;94:1842–1849. doi: 10.1161/01.cir.94.8.1842. [DOI] [PubMed] [Google Scholar]
- 12.Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354–1367. doi: 10.1161/01.cir.87.4.1354. [DOI] [PubMed] [Google Scholar]
- 13.De Bruyne B, Baudhuin T, Melin JA, et al. Coronary flow reserve calculated from pressure measurements in humans: validation with positron emission tomography. Circulation. 1994;89:1013–1022. doi: 10.1161/01.cir.89.3.1013. [DOI] [PubMed] [Google Scholar]
- 14.Bech GJ, Droste H, Pijls NH, et al. Value of fractional flow reserve in making decisions about bypass surgery for equivocal left main coronary artery disease. Heart. 2001;86:547–552. doi: 10.1136/heart.86.5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindstaedt M, Yazar A, Germing A, et al. Clinical outcome in patients with intermediate or equivocal left main coronary artery disease after deferral of surgical revascularization on the basis of fractional flow reserve measurements. Am Heart J. 2006;152:156.e1–156.e9. doi: 10.1016/j.ahj.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 16.Potvin JM, Rodés-Cabau J, Bertrand OF, et al. Usefulness of fractional flow reserve measurements to defer revascularization in patients with stable or unstable angina pectoris, non-ST-elevation and ST-elevation acute myocardial infarction, or atypical chest pain. Am J Cardiol. 2006;98:289–297. doi: 10.1016/j.amjcard.2006.02.032. [DOI] [PubMed] [Google Scholar]
- 17.Fischer JJ, Wang XQ, Samady H, et al. Outcome of patients with acute coronary syndromes and moderate coronary lesions undergoing deferral of revascularization based on fractional flow reserve assessment. Catheter Cardiovasc Interv. 2006;68:544–548. doi: 10.1002/ccd.20748. [DOI] [PubMed] [Google Scholar]
- 18.Berger A, Botman KJ, MacCarthy PA, et al. Long-term clinical outcome after fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. J Am Coll Cardiol. 2005;46:438–442. doi: 10.1016/j.jacc.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 19.Wongpraparut N, Yalamanchili V, Pasnoori V, et al. Thirty-month outcome after fractional flow reserve-guided versus conventional multivessel percutaneous coronary intervention. Am J Cardiol. 2005;96:877–884. doi: 10.1016/j.amjcard.2005.05.040. [DOI] [PubMed] [Google Scholar]
- 20.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:156–175. doi: 10.1161/CIRCULATIONAHA.105.170815. [DOI] [PubMed] [Google Scholar]
- 21.Pijls NH, Fearon WF, Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) Study. J Am Coll Cardiol. 2010;56:177–184. doi: 10.1016/j.jacc.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Fearon WF, Bornschein B, Tonino PA, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation. 2010;122:2545–2550. doi: 10.1161/CIRCULATIONAHA.109.925396. [DOI] [PubMed] [Google Scholar]
- 23.Nam CW, Mangiacapra F, Entjes R, et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol. 2011;58:1211–1218. doi: 10.1016/j.jacc.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 24.Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555. doi: 10.1093/eurheartj/ehq277. [DOI] [PubMed] [Google Scholar]
- 25.De Bruyne B, Pijls NH, Barbato E, et al. Intracoronary and intravenous adenosine 5'-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation. 2003;107:1877–1883. doi: 10.1161/01.CIR.0000061950.24940.88. [DOI] [PubMed] [Google Scholar]
- 26.Wilson RF, Wyche K, Christensen BV, Zimmer S, Laxson DD. Effects of adenosine on human coronary arterial circulation. Circulation. 1990;82:1595–1606. doi: 10.1161/01.cir.82.5.1595. [DOI] [PubMed] [Google Scholar]
- 27.Kern MJ, Deligonul U, Tatineni S, Serota H, Aguirre F, Hilton TC. Intravenous adenosine: continuous infusion and low dose bolus administration for determination of coronary vasodilator reserve in patients with and without coronary artery disease. J Am Coll Cardiol. 1991;18:718–729. doi: 10.1016/0735-1097(91)90795-b. [DOI] [PubMed] [Google Scholar]
- 28.Lindstaedt M, Bojara W, Holland-Letz T, et al. Adenosine-induced maximal coronary hyperemia for myocardial fractional flow reserve measurements: comparison of administration by femoral venous versus antecubital venous access. Clin Res Cardiol. 2009;98:717–723. doi: 10.1007/s00392-009-0056-7. [DOI] [PubMed] [Google Scholar]
- 29.Seo MK, Shin DH, Yang HM, et al. Comparison of hyperemic efficacy between central and peripheral veous adenosine infusion for fractional flow reserve measurement. Circulation. 2010;122:A18620. doi: 10.1161/CIRCINTERVENTIONS.111.965392. Abstract. [DOI] [PubMed] [Google Scholar]
- 30.Nair PK, Marroquin OC, Mulukutla SR, et al. Clinical utility of regadenoson for assessing fractional flow reserve. JACC Cardiovasc Interv. 2011;4:1085–1092. doi: 10.1016/j.jcin.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 31.Jang HJ, Koo BK, Kim JH, et al. Safety and efficacy of a novel hyperemic agent, nicorandil, for invasive physiologic assessment in a catheterization laboratory: a prospective multicenter study. Korean Circ J. 2011:550608A. Abstract. [Google Scholar]
- 32.Sen S, Escaned J, Malik IS, et al. Development and Validation of a New Adenosine-Independent Index of Stenosis Severity From Coronary Wave-Intensity Analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) Study. J Am Coll Cardiol. 2012;59:1392–1402. doi: 10.1016/j.jacc.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Kim HJ, Vignon-Clementel IE, Coogan JS, Figueroa CA, Jansen KE, Taylor CA. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann Biomed Eng. 2010;38:3195–3209. doi: 10.1007/s10439-010-0083-6. [DOI] [PubMed] [Google Scholar]
- 34.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989–1997. doi: 10.1016/j.jacc.2011.06.066. [DOI] [PubMed] [Google Scholar]
- 35.Min JK, Berman DS, Budoff MJ, et al. Rationale and design of the DeFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic AngiOgraphy) Study. J Cardiovasc Comput Tomogr. 2011;5:301–309. doi: 10.1016/j.jcct.2011.08.003. [DOI] [PubMed] [Google Scholar]