Figure 6.
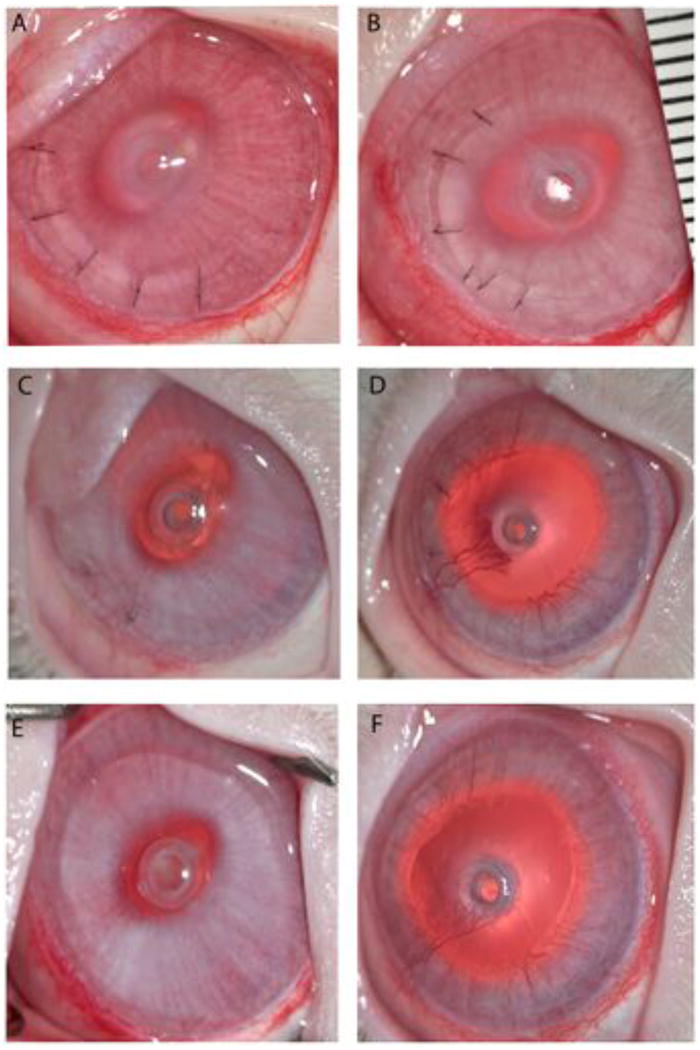
Clinical photographs of comparative KPro-FP placed intrastromally with the extension into the anterior chamber of the eye of a New Zealand white rabbit shown at three representative time points. (A, B) At post-operative day 2, HMPEI-PMMA KPro-FP (A) rabbit eye shows a lamellar flap with 6 sutures and mild post-operative corneal swelling similar to control PMMA KPro-FP (B) showing the same clinical features. (C, D) At one month post-operatively, HMPEI-PMMA KPro-FP (C) shows minimal corneal swelling, only a mild neovascularization at the surgical wound site, and no corneal ectasia, while PMMA KPro-FP (D) shows moderate corneal edema, corneal neovascularization has advanced to the front plate, and there is mild corneal ectasia. (E, F) By three months post-operatively, HMPEI-PMMA KPro-FP (E) remains quiescent with minimal corneal reactivity, neovascularization, and conical ectasia compared to the uncoated control PMMA KPro-FP (F) that shows moderate corneal swelling, extension of the corneal neovascularization over the front piece, and progressive conical ectasia.
