Abstract
Background
Japanese encephalitis virus (JEV) is a major mosquito-borne pathogen that causes viral encephalitis throughout Asia. Vaccination with an inactive JEV particle or attenuated virus is an efficient preventative measure for controlling infection. Flavivirus NS1 protein is a glycoprotein secreted during viral replication that plays multiple roles in the viral life cycle and pathogenesis. Utilizing JEV NS1 as an antigen in viral vectors induces a limited protective immune response against infection. Previous studies using E. coli-expressed JEV NS1 to immunize mice induced protection against lethal challenge; however, the protection mechanism through cellular and humoral immune responses was not described.
Results
JEV NS1 was expressed in and purified from Drosophila S2 cells in a native glycosylated multimeric form, which induced T-cell and antibody responses in immunized C3H/HeN mice. Mice vaccinated with 1 μg NS1 with or without water-in-oil adjuvant were partially protected against viral challenge and higher protection was observed in mice with higher antibody titers. IgG1 was preferentially elicited by an adjuvanted NS1 protein, whereas a larger load of IFN-γ was produced in splenocytes from mice immunized with aqueous NS1. Mice that passively received anti-NS1 mouse polyclonal immune sera were protected, and this phenomenon was dose-dependent, whereas protection was low or delayed after the passive transfer of anti-NS1 MAbs.
Conclusion
The purified NS1 subunit induced protective immunity in relation with anti-NS1 IgG1 antibodies. NS1 protein efficiently stimulated Th1-cell proliferation and IFN-γ production. Protection against lethal challenge was elicited by passive transfer of anti-NS1 antisera, suggesting that anti-NS1 antibodies play a substantial role in anti-viral immunity
Keywords: Japanese encephalitis virus; T-cell response, Antibodies; Monoclonal antibodies; NS1 protein; Mouse model
Introduction
Japanese encephalitis virus (JEV) is one of the most important mosquito-borne viruses in East and Southeast Asia, where seasonal outbreaks cause more than 50,000 infections and 10,000 deaths annually [1]. JEV is a mosquito-borne flavivirus in the family Flaviviridae. The Flavivirus genus contains more than 70 viruses with positive-sense, single-stranded RNA genomes (~11 kb) that encode a polypeptide (~ 3400 amino acids) consisting of the capsid protein C (core protein), the matrix protein (envelope protein M), the major envelope protein E, a number of small non-structural proteins (NS1, NS2A, NS2B, NS4A and NS4B), a helicase (NS3) and a RNA-directed polymerase (NS5) that are cleaved and co- or post-translationally processed by host- or virus-specific proteases [2]. The first non-structural protein (NS1) is translocated to the endoplasmic reticulum (ER) via signal sequences in a trans-membrane C-terminal stretch of protein E, where it is involved in ER-associated RNA replication [3]. NS1 is N-glycosylated then secreted to the extracellular milieu [4]. The pathogenic role of NS1 remains largely unknown, but has been shown to be associated with Factor H in West Nile virus (WNV) infection [5] and with C4b in WNV, yellow fever virus (YFV), and dengue virus (DENV) infections, where it may modulate complement activation [6,7]. NS1 may use structural mimicry similar to those found in the endothelial membrane or coagulation factors, which may elicit the autoimmunity that is deleterious in DENV hemorrhagic fever [8,9]. However, no such auto-antibody has yet been found in JEV infection [10]. Its association with phospholipids may induce vascular homeostasis in DENV hemorrhagic fever, which is similar to that induced by plasma lipoproteins [4].
Prevention of Japanese encephalitis through vaccination was shown to be efficient when using either a formalin-inactivated virus produced in mouse brain or cell culture, or a live attenuated vaccine, SA14-14-2 [11], which was developed in China and is broadly used for childhood vaccination in mainland China, India, and several other Southeast Asian countries [12]. The SA14-14-2 virus is produced in hamster primary kidney cells and is widely used in vaccination programs because of its innocuity, efficiency, and low cost to developing countries. A JEV vaccine approved by the Food and Drug Administration was recently produced in Vero cells, which was purified from SA14-14-2-infected cell supernatants and inactivated formalin [11].
The immunogenicity and protective immunity of flavivirus NS1 has been studied using various vaccine types. Animals were either immunized with YFV NS1 [13], or infected with vaccinia viruses or adenoviruses expressing recombinant NS1 from DENV [14], YFV [15], tick-borne encephalitis virus (TBEV) [16,17], or WNV [18]. However, they showed variable protective immune responses. Vaccinations with flavivirus NS1 DNA were also tested in NS1-induced immune protection studies against DENV [19] and TBEV [20]. These studies showed that the NS1 contributes to the induction of protective immunity against flaviviral infections. The anti-NS1 protection mechanism was partially determined, showing that passive transfer of anti-YFV NS1 monoclonal antibodies (MAbs) protected mice or reduced their neuropathology after YFV challenge [21,22] and that WNV anti-NS1 MAbs protected mice from lethal challenge [23,24].
Mice immunized with JEV NS1 expressed in insect cells induced low protection [25]. Recombinant viruses or DNA vaccines expressing JEV E or NS1 genes were used to vaccinate mice, which resulted in differing levels of protection [26]. The value of using a vaccine containing the native hexameric form of a purified flavivirus NS1 glycoprotein to protect against lethal viral challenges has yet to be tested in mice. One obstacle in protection studies is that mice are less susceptible to a viral challenge by the time a vaccination schedule in immunocompetent mice is achieved. A possible surrogate for testing protective efficacy is the use of adoptive immunity by injecting flavivirus anti-NS1 antibodies into young mice [14,17,22].
A JEV NS1 protein purified from a Drosophila S2 established cell line supernatant [27] was used to immunize C3H/HeN (C3H) mice and to test the induction of cellular and humoral immunity. Protection of mice by antibodies elicited against NS1 was tested by JEV infection of mice that were actively or passively immunized. Our results support the role of anti-NS1 antibodies in protection against flaviviral infection.
Results
Characterization of the NS1 immunogen
In a previous study, we successfully produced and purified large amounts of extracellular hexameric forms of JEV NS1 protein [27]. We studied the processing and composition of carbohydrates of NS1 protein produced in the supernatant of Drosophila S2 cells. Heat-denatured NS1 was mock-treated or treated with Endo H (Endoglycosidase H) or PNGase F (Peptide: N-Glycosidase F). Endo H and PNGase F treatment reduced the molecular weight of extracellular NS1, by 2 kD (Additional file 1: Figure S1A), indicating that the protein acquired glycans in the secretory pathway of Drosophila cells. The type of glycans was identified by lectin affinity. The NS1 protein was recognized by GNA (Galanthus nivalis agglutinin) which recognizes terminal mannose, and DSA (Datura stramonium agglutinin) which recognizes Gal-(1–4)N-Acetylglucosamine (GlcNAc) in complex and hybrid N-glycans, respectively (Additional file 1: Figure S1B), but not by SNA (Sambucus nigra agglutinin) which recognizes sialic acid linked (2–6) to galactose and MAA (Maackia amurensis agglutinin) which recognizes sialic acid linked (2–3) to galactose (data not shown). These results indicated that the glycoprotein NS1 contained N-glycans with Gal-(1–4)GlcNAc and a terminal mannose, but apparently not sialic acid.
Mouse immune responses to NS1 and SA14-14-2 immunization
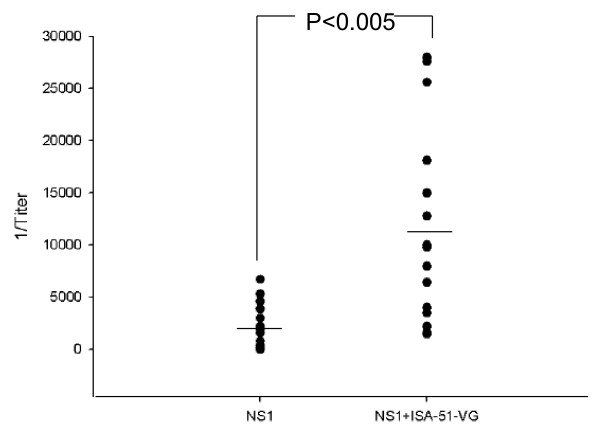
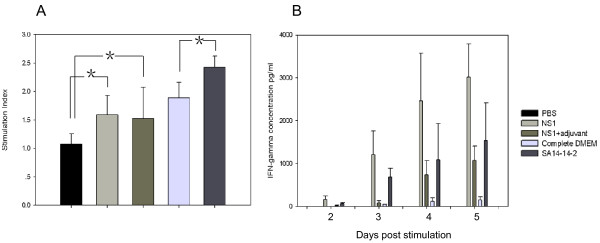
Four-week-old C3H mice were immunized twice four weeks apart using a purified NS1 hexamer obtained from Drosophila S2 cell line supernatants [27], either alone (aqueous) or adjuvanted with water-in-oil ISA-51-VG. Serum samples from each group were tested individually by anti-NS1 antibody titration. NS1 immunization induced anti-NS1 antibody responses in both groups of mice and the use of an adjuvant significantly increased the antibody titer (p < 0.005) (Figure 1). Six mouse sera samples from each group were pooled to test IgG1 and IgG2a antibodies against NS1. Immunization with aqueous or adjuvanted NS1 protein induced both IgG1 and IgG2a antibody responses, with an IgG1 titer four to nine times higher than that of IgG2a, but a similar titer to IgG2a (Table 1). SA14-14-2 vaccination mainly induced anti-NS1 IgG2a antibodies. The proliferation of T-cells and IFN-γ secretion by splenic cells of immunized C3H mice in response to stimulation with purified JEV NS1 protein were tested. The T-cell proliferation stimulation index (SI) of the PBS group was 1, while those of the aqueous NS1 and adjuvanted NS1 groups were 1.59 and 1.51, respectively, and these were both significantly higher (p < 0.05) than the SI of the phosphate buffered saline (PBS) group (Figure 2A). After vaccination with SA14-14-2 or Dulbecco's modified Eagle's medium (DMEM), purified NS1 was used for splenic cell stimulation in vitro. The T-cell proliferation SI of SA14-14-2 was 2.42, significantly higher than the control group (SI = 1.88; p < 0.05) (Figure 2A). IFN-γ production by splenic cells was quantified over a period of five days. IFN-γ was detected on day 2 or 3 post-stimulation in the splenocyte culture supernatants of mice immunized with aqueous or adjuvanted NS1, SA14-14-2 and complete DMEM. The highest IFN-γ load was 3 ng ml–1 in the aqueous NS1 group, 1 ng ml–1 in the adjuvanted NS1 group, 1.5 ng ml–1 in the SA14-14-2 group and 150 pg ml–1 in the complete DMEM group on day 5 post-stimulation (Figure 2B).
Figure 1.
IgG antibody response of mice immunized with aqueous and adjuvanted NS1. Four-week-old C3H mice were immunized with 1 μg of purified NS1. Two weeks after a second immunization was given at two months of age, mouse sera were sampled and the IgG titers were tested by indirect ELISA. The data for immunization with recombinant NS1 are derived from two independent experiments. Antibodies of 18 mice sera were titrated for each group and analyzed by Student’s t-test.
Table 1.
Determination of antibodies titers and sero-neutralization of pooled sera from immunized mice
|
Immunogen |
Antibodies Titration |
Sero- IgG IgG1 IgG2a neutralization |
||||||
|---|---|---|---|---|---|---|---|---|
| IgG | IgG1 | IgG2a | ||||||
| |
Beforea |
Afterb |
Before |
After |
Before |
After |
Before |
After |
| NS1 |
5000 |
6400 |
5000 |
5000 |
1200 |
3000 |
0 |
40 |
| NS1 + adjuvant |
15000 |
18000 |
15000 |
15000 |
1600 |
3200 |
0 |
40 |
| SA14-14-2 |
1200 |
1000 |
300 |
0 |
2400 |
2400 |
80 |
80 |
| PBS | 0 | 600 | 0 | 0 | 0 | 2400 | 0 | 40 |
a Sera collected two weeks after 2nd boost and two weeks before challenge.
b Sera collected four weeks after challenge.
Figure 2.
Proliferation and IFN-γ secretion of splenic cells from immunized C3H mice in response to inoculation with recombinant JEV NS1 protein and SA14-14-2. Splenocytes isolated from mice immunized with PBS, aqueous NS1, adjuvanted NS1, DMEM with 3% FBS (complemented DMEM) and attenuated virus SA14-14-2, were stimulated with purified NS1. A: Splenocyte proliferation. The proliferation stimulation index (SI) was defined as the ratio of stimulated cells to unstimulated cells. B: IFN-γ secretion. The IFN-γ production of splenic cells was quantified over a period of five days. Three mice were used for each group. The SI and IFN-γ concentration were analyzed by Student’s t-test. P < 0.05 was considered to be significant. *, significant difference.
NS1 immunization induced immune responses that partially protected mice from viral challenge
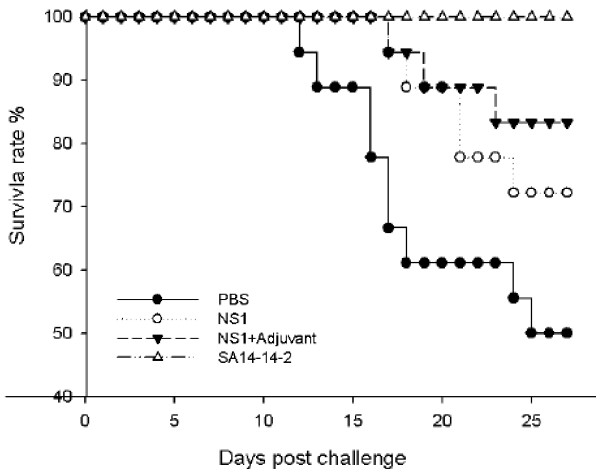
To determine whether the anti-NS1 immunity observed in immunized mice was protective, mice were challenged by an intranasal (i.n.) injection of 104 pfu of JEV SA14 and mortality was recorded over four weeks . This virus dose corresponded to 100 times the lowest dose killing the largest number of mice (Additional file 2: Figure S2B). Mouse challenge by i.n. was chosen rather than i.p. because the number of deaths and the time before death were more consistent (Additional file 2: Figure S2A). The survival rate of the adjuvanted NS1 group was significantly higher (83%) when compared with a negative control group (injection with PBS) that had a 50% survival rate (p < 0.05) (Figure 3, Table 2). The survival rate of the aqueous NS1 group was 72%, but the difference from the survival rate of the negative control group was not significant (p > 0.05) (Table 2), although a delay in the time of death was observed in the aqueous NS1-immunized mice when compared with the PBS mock-immunized mice (Figure 3).
Figure 3.
Survival curves of SA14-14-2-vaccinated and NS1-immunized mice after JEV challenge. Groups of three-month-old SA14-14-2-vaccinated or NS1-immunized C3H mice (see Figure 1) were i.n. challenged with 1 × 104 pfu of JEV SA14. The JEV-infected mice were monitored daily for 28 days. Survival curves of mice immunized with recombinant NS1 protein or injected with PBS were constructed using data from two experiments, with groups of 6–12 mice. JEV-vaccinated mice were tested once using eight mice. Control mice received PBS and were challenged with JEV.
Table 2.
Survival rate of C3H mice immunized with NS1 and SA14-14-2
| Immunogen | No. of Survival mice/ No. of Immunized mice (survival rate) | pa |
|---|---|---|
| NS1 |
13/18 (72%) |
0.195 |
| NS1 + adjuvant |
15/18 (83%) |
0.024 |
| SA14-14-2 |
8/8 (100%) |
0.021 |
| PBS | 9/18 (50%) |
aP value was obtained by log rank test when comparing the survival curve of each group of vaccinated mice with PBS group.
Sera of mice that had survived the SA14 virus challenge were titrated by ELISA. SA14 infection did not increase the anti-NS1 IgG2a titers in the SA14-14-2-vaccinated group, and anti-NS1 IgG1 was not detected after the challenge. In contrast, SA14 challenge induced an IgG2a antibody titer increase, but not IgG1, in the aqueous or adjuvanted NS1 groups (Table 1). Mouse sera collected before and after challenge were also tested for seroneutralization to follow seroconversion. Sera from mice immunized with NS1 reached a TCID50 titer of 40 after the challenge. Sera from the SA14-14-2 group exhibited the same neutralization titer (TCID50 titer = 80) before and after the challenge (Table 1). These data suggest that the attenuated virus vaccine, but not NS1, induced a sterilizing immunity against JEV.
In a previous experiment, sera from mice were pooled for antibody subtyping and neutralization testing. In order to verify whether there was any correlation between anti-NS1 antibody titer elicited by vaccination with NS1 and challenge protection, ELISA titers of 18 mice were calculated individually before challenge. Table 3 shows that the total number of surviving aqueous NS1-vaccinated mice (66.7%) was not significantly higher than those receiving PBS (44.4%) (p = 0.41); whereas all mice that had anti-NS1 antibody titers ≥ 2400 were all protected (p = 0.008) compared to mice that had titers < 2400 were not protected (33.3%) compared to the control (44.4%) (p = 1). This result suggests a relationship between anti-NS1 antibody titer and protective immunity against i.n. JEV challenge.
Table 3.
Survival rate of three month-old C3H mice immunized with NS1 or PBS
| Immunogen | Anti-NS1 IgG antibody titer rangea | No. of Survival mice/No. of Immunized mice (Survival rate) | Pb |
|---|---|---|---|
| NS1 |
0-12800 |
12/18 (66.7%) |
0.41 |
| NS1 |
0-2400 |
3/9 (33.3%) |
1 |
| NS1 |
2400-12800 |
9/9 (100%) |
0.008 |
| PBS | 0 | 4/9 (44.4%) |
a Two weeks before challenge, mouse sera were collected for anti-NS1 IgG antibody titration. The NS1-immunized group of mice (18 mice in total) was divided into two groups according to anti-NS1 IgG titers: one group with anti-NS1 IgG <2400 (9 mice) and one group with anti-NS1 IgG >2400 (9 mice).
bP value was obtained by log rank test when comparing the survival curve of each group with PBS group.
Passive protection of mice by anti-NS1 antibodies
We previously calculated that 20 pfu of JEV SA14 virus could kill 100% of four-week-old i.p.-infected C3H mice [28] as shown in Additional file 2: figure S2C.
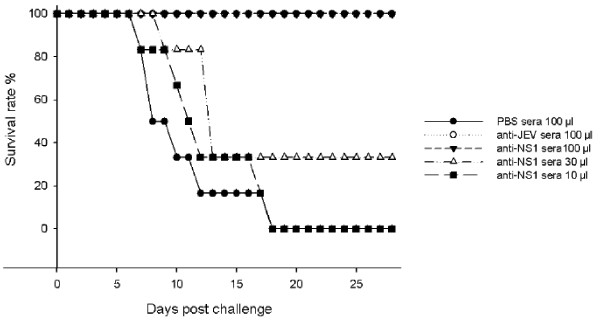
To determine whether the protection of immunized mice was associated with an anti-NS1 antibody response, the sera from NS1-immunized mice with high titers of anti-NS1 antibodies (>1:3000) were collected and pooled to perform passive transfer tests. One hundred μl of NS1 mouse anti-sera injected 1 h prior to challenge provided 100% protection in challenged mice, but decreasing the dose to 30 μl and 10 μl provided 33% and no protection, respectively (Figure 4). While sera from SA14-14-2-vaccinated mice conferred 100% protection, all mice died that were injected with sera from PBS mock-immunized mice (Figure 4).
Figure 4.
Survival of mice passively injected with anti-NS1 antisera and challenged with JEV. Groups of four-week-old C3H mice were administered with 100 μl, 30 μl and 10 μl of anti-NS1 mouse antisera, or 100 μl sera from PBS-injected mice (negative control) or 100 μl of anti-SA14-14-2 antisera (anti-JEV), and infected 1 hr later with 20 pfu of JEV SA14. The JEV infected mice were monitored daily for 28 days. The survival curve was constructed using data from one (100 μl anti-JEV, 30 and 10 μl of anti-NS1 antisera), two (sera from PBS-injected mice) or three (100 μl of anti-NS1 antisera) experiments. For 100 μl anti-JEV antisera group, 30 and 10 μl of anti-NS1 antisera groups, sera from PBS-injected mice group, 6 mice were used for each experiments. Six to 12 mice were used for 100 μl anti-NS1 antisera groups of each experiment.
Characterization of a panel of MAbs against NS1, for passive protection
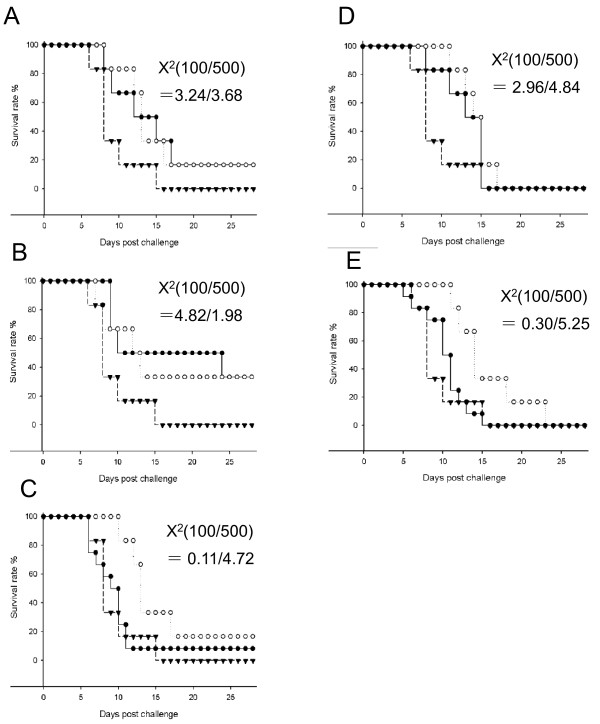
Eighteen MAbs against NS1 were generated in a previous study [27] and five had high affinity for NS1 (3E10, 4C4, 7C2, 7H5 and 8F1), where they recognized cell surface-associated and intracellular NS1 (Table 4). MAb 4C4 recognized the N-terminus of NS1; MAb 3E10 detected NS1 in an ELISA and IFA, but not in a Western blot, indicating a probable recognition of a conformational epitope. Three MAbs recognized the C-terminus of the protein and cross-reacted with the DENV NS1 protein (Table 4). These five MAbs were purified and quantified before being passively transferred at doses of 100 μg or 500 μg to four-week-old mice. Mice were challenged with 20 pfu of SA14 virus 1 h after MAb injection and mortality was recorded for four weeks. Mouse survival rates after passive transfer of 100 μg of MAb 3E10, 4C4, and 7C2 were 16%, 33%, and 8%, respectively, whereas no mice survived after injection with MAbs 7H5 or 8F1, or with the anti-HIV antibody used as a control (Figure 5, Table 5). However, increasing 7C2, 7H5, and 8F1 MAbs dosages to 500 μg per mouse enhanced the survival period (Figure 5, Table 5). Calculation of the χ2 for the survival rate, the delay until mortality, and the dose of antibody indicated a significant anti-viral activity with these MAbs (p < 0.05) (Table 5).
Table 4.
Monoclonal antibodies characterization and testing of passive protection
|
MAbs |
Intracellulara |
Surface associatedb |
IFAc |
Affinity KD (nM)d |
MAb binding domaine |
% Mice survival ratef |
|
|---|---|---|---|---|---|---|---|
| JEV Dengue 2 V | |||||||
| 3E10 |
+ |
+ |
+ |
- |
1.1 |
unknown |
16 |
| 4 C4 |
+ |
+ |
+ |
+ |
56 |
NS11–143 |
33 |
| 7 C2 |
+ |
+ |
+ |
+ |
17 |
NS1224–352 |
8 |
| 7 H5 |
+ |
+ |
+ |
+ |
6.4 |
NS1224–352 |
0 |
| 8 F1 | + | + | + | + | 5 | NS1224–352 | 0 |
a/bMAbs were incubated with S2-NS11–352 cells permeabilized or untreated (intracellular/surface associate) for fluorescence testing by flow cytometry (FACScan).
c Immunofluorescence assay (IFA) for testing monoclonal antibodies reactivity against BHK cells infected with JEV, and C6/36 cells infected with Dengue 2 virus.
d The affinity of MAbs to NS1 tested by surface plasmon resonance (SPR).
e Reactivity of MAbs for S2- NS11–143 or NS1224–352 fragments. Cells lysates were tested by Western blotting (WB). “Unknown” means did not react with both of the NS1 fragments or reduced and boiled NS1.
f Six to twelve mice were administered with 100μg of 3E10, 4 C4, 7 C2 and 8 F1, respectively, and challenged by JEV SA14.
Figure 5.
Survival of mice passively immunized with anti-NS1 monoclonal antibodies. Groups of four-week-old C3H mice were administered with 100 μg (black dot) or 500 μg (white dot) of purified MAbs 3E10 (A), 4C4 (B), 7C2 (C), 7H5 (D), 8F1 (E) before being challenged with 20 pfu of SA14. Another group of mice received 100 μg of HIV anti-envelope MAb (black triangle) as a negative control. JEV-infected mice were monitored daily for 28 days post-challenge. Survival curves were constructed using data from one or two experiments with 6–12 mice in each group. χ2 values were obtained using a log-rank test by comparing the survival curve of each group with the anti-HIV group.
Table 5.
Survival rate of C3H mice passively immunized with anti-NS1 monoclonal antibodies
| MAbs | MAb dose (μg) | No. of survival mice/ No. of passive transfer mice (survival rate) | pa |
|---|---|---|---|
| 3E10 |
100 |
1/6 (16.7%) |
0.07 |
| |
500 |
1/6 (16.7%) |
0.05 |
| 4 C4 |
100 |
2/6 (33.3%) |
0.02 |
| |
500 |
2/6 (33.3%) |
0.15 |
| 7 C2 |
100 |
1/12 (8.3%) |
0.74 |
| |
500 |
1/6 (16.7%) |
0.02 |
| 7 H5 |
100 |
0/6 (0%) |
0.08 |
| |
500 |
0/6 (0%) |
0.02 |
| 8 F1 |
100 |
0/12 (0%) |
0.58 |
| |
500 |
0/6 (0%) |
0.02 |
| Anti-HIV | 100 | 0/6 (0%) |
aP value was obtained by log rank test when comparing the survival curve of each group of mice which received anti-NS1 MAb with anti-HIV group.
Discussion
Japanese encephalitis remains a serious public health threat in Asia, where more than two billion people are at risk. The complex JEV zoonotic cycle prevents any direct action to reduce viral transmission; therefore, human infection can only be prevented by vaccination campaigns with children [12]. Apart from the live-attenuated JEV vaccine SA14-14-2 developed for childhood application [11], no affordable JEV vaccine is recognized for mass vaccination. Several vaccine candidates inducing neutralizing antibodies are under clinical trial and they may meet the immunogenicity and protective capacity requirements after a single dose regimen [11]. However, the use of NS1 protein as an immunogen to reinforce the immune response to JEV structural proteins has been discussed, although the induction mechanisms of protective JEV immunity using a NS1 hexameric antigen form have not been investigated. Drosophila S2 cells have been used for JEV NS1 protein expression and purification from the cell supernatant harvested after serum-free cell culture [27]. Previous recovery of DENV E protein crystals in S2 cells indicated that this system expressed native-like and well-folded glycoproteins [29]. More than 50 mg L–1 of the hexameric form of NS1 glycosylated protein were expressed in the cell culture supernatant [27], which was shown in this study to contain carbohydrates similar to the native protein produced in infected cells [30] and was suitable for recombinant vaccine subunit preparation. In this study, two doses of 1 μg of glycosylated hexameric JEV NS1 were used to immunize mice. High antibody titers were detected in the sera of two groups of mice immunized with aqueous or emulsified NS1 with ISA-51-VG formulations. The adjuvant ISA-51-VG was a mix of mineral oil and a surfactant, which has been previously tested for human vaccination [31]. This adjuvant was tested for its capacity to boost the T-cell response against NS1 in immunized mice. The titers of IgG1 subclass were 4–9 times higher than those of IgG2a in both groups of mice, while titers of IgG1 in mice immunized with adjuvanted NS1 were 2–4 times higher when compared with those of mice immunized with aqueous NS1, whereas IgG2a titers remained low. Similarly, 100 times higher IgG1 titers compared with IgG2a were observed in mice that were immunized with E. coli-expressed JEV NS1 protein mixed with Freund’s adjuvant [32]. This difference was presumably due to the use of Freund’s adjuvant, the high antigen dose and the number of antigen injections (three instead of two). In vitro splenocyte stimulation by NS1 elicited T-cell proliferation and IFN-γ secretion, although higher IFN-γ secretion was observed in mice immunized with aqueous NS1. These results suggested that the NS1 proteins are engulfed by antigen presenting cells (APCs) in vivo. The peptides derived from NS1 digestion are subsequently presented by MHC class II molecules to T helper cells. The IgG1 subclass antibody response corresponds to Th2 cell activation, whereas the IgG2a response reflects Th1 cell activation. The IFN-γ produced by Th1 cells inhibits Th2 cell proliferation and IgG1 production [30]. These results indicate that NS1 immunization elicited both Th1 and Th2 cell responses and that ISA-51-VG improved IgG1 production, and reduced Th1 activation and INF-γ expression. Mice inoculated with TBE NS1, which was expressed by a recombinant adenovirus, stimulated in vivo IFN-γ production [17]. A previous study showed that soluble DENV-1 NS1 is a lipoprotein [4] and was internalized by mouse hepatocytes in vivo and by cultured cell lines in vitro [33]. We observed that purified soluble JEV NS1 attached to many types of cell membranes in vitro and was subsequently internalized (Li and Deubel, unpublished data). This feature may at least partially explain why aqueous NS1 rapidly stimulated the Th1 cell response via APCs, whereas NS1 mixed with ISA-51-VG was slowly released from the emulsion and preferentially activated a Th2 response [31,34]. The cell-mediated immune response induced by SA14-14-2 immunization and NS1 stimulation was also studied. Compared with the NS1 group, the SA14-14-2 group showed higher cell proliferation SI but lower IFN-γ production. These differences may be due to different epitope presentation from native protein or replicative virus cytokine profiles in response to NS1 and SA14-14-2 immunization, respectively. IL-2 was detected in SA14-14-2, but not in NS1-immunized mice (data not shown), confirming a Th1 stimulation pathway induced by replicative viruses. Production of cytotoxic T lymphocytes (CTLs) is another protective immune response induced by NS1 immunogens issued from replicative viruses [35]. Mice primed with JEV-infected cells [36] or JEV NS1 expression recombinant viruses [37] stimulated mice to generate CTLs against JEV. Further study showed that CTLs recognize peptides derived from NS1 and NS3 [35]. One study showed that NS1-expressing DNA immunogen could stimulate CTLs against JEV in mice, but induced low protection [38]. However, we did not expect any CTL response since NS1 was not presented in a replicative system that could stimulate class I antigen presentation.
The protective immune responses elicited against the purified JEV NS1 hexameric protein was investigated by challenging mice with JEV SA14 injected i.n. Immunization with recombinant subunits required several injections, but the mice were not highly susceptible to JEV at the end of the immunization schedule. However, the i.n. method adopted in this study killed more consistently mice aged over three months than i.p. inoculation (Additional file 2: Figure S2A and B). Another approach would have been to infect mice by an intracerebral or an i.p. route [39], but we felt these techniques did not simulate a natural transmission, as they mechanically break the blood brain barrier. In our study, two doses of 1 μg of hexameric NS1 emulsified in adjuvant provided significant protection (83%) against viral challenge when compared with soluble NS1 (72%), as it reduced morbidity and mortality and increased the survival period after infection. Anti-NS1 immune responses were induced by YFV, DENV, TBEV and WNV immunization with NS1 protein, an NS1-encoding DNA gene, or viral vectors expressing NS1 [13,14,18]. Mouse immunization with JEV NS1 produced in Spodoptera frugiperda Sf9 insect cells induced little or no protection [25], whereas NS1 carried by viral vectors induced an antibody response [26,37], but low protection [26,37]. DNA vaccination of mice with the NS1 gene [40] induced more than 80% protection, whereas DNA vaccination with the NS1-NS2A gene protected only 20% of mice against a JEV challenge [39]. Interestingly, 100 μg of non-folded and non-glycosylated JEV NS1 was produced in E. coli and injected three times to induce protective immunity in 87.5% of vaccinated mice [32]. Recently, a study using protein E fragments or NS1 produced in E. coli and injected at 50 μg seven (i.n.) or five (i.p.) times showed better protection when the proteins were injected i.n. rather than i.p. [41]. Only two much lower doses of the hexameric NS1 form provided protective effects, which may be due to the elicitation of antibodies that bind to conformational epitopes.
Higher antibody titers in the mouse group with a higher survival rate suggested that NS1 had induced an antibody response that might play an important role in preventing JEV infection. In order to verify this hypothesis, different antibody doses induced during mouse immunization were injected into naïve mice. One-month-old mice were used for the adoptive immunity test, so it was possible to apply an i.p. challenge in C3H mice, which caused 100% mortality with a low dose of virus [28]. Passive transfer of 100 μl of anti-NS1 antisera (titrated 1:3000) to one-month-old mice protected 100% from morbidity and death, whereas 30 μl was less protective and 10 μl was not protective, suggesting that an important NS1 function in JEV pathogenesis could be inhibited by IgG-NS1 immunocomplexes. However, anti-NS1 has no neutralizing activity on virus infection in vitro. The antibody-dependent complement-mediated cytolysis of JEV-infected cells associated with anti-NS1 antibodies was demonstrated by in vitro experiments [42]. Another study showed that the depletion of C3 complement components in mice did not affect the anti-NS1 passive protection capacity against YFV [22]. In addition, immunization with a genetic deletion in C5 using an adenovirus expressing NS1 protected mice from a TBEV lethal challenge [16]. These experiments suggested that antibody-dependent complement-mediated cytolysis may play a minor role in antibody-associated immune protection in vivo. However, WNV anti-NS1 MAb through Fc-γ receptor-dependent and C1q-independent pathways could be an alternative protection route involving the scavenging of infected cells by macrophages [23,24]. In our study, five JEV anti-NS1 MAbs generated in a previous study [27] that exhibited a high binding affinity against different NS1 epitopes were used in a passive protection test. Two MAbs exhibited no capacity to prevent death, although they significantly extended survival by 2–6 days. MAb 3E10 was directed against a conformational epitope, while MAb 4C4 recognized the NS1 N-terminus and 7C2 recognized the NS1 C-terminus and provided significant delay and prevention against JEV mortality. However, 500 μg of MAbs 7H5 and 8F1 significantly delayed death after JEV infection in a dose-dependent manner and were probably directed against a linear epitope of the C-terminus fraction of NS1 that cross-reacted with DENV NS1 (Tables 4 and 5). Whether those MAbs recognize the same epitope is not known, but they presented different NS1 binding affinities. Interestingly, anti-WNV MAbs that bound to a similar NS1 fragment also provided mice with up to 90% protective immunity from a lethal challenge [23]. Identification of the epitope(s) targeted by the three JEV anti-NS1 MAbs would facilitate further study of the NS1 antibody interaction and its function in anti-flaviviral immunity. Further study using a mixture of those MAbs and their possible role in scavenging NS1-IgG complexes would bring a better understanding of the function of anti-NS1 antibodies in protective immunity.
The mechanism by which NS1 contributes to in vivo flaviviral pathogenesis is largely unknown, which hinders the elucidation of the mechanism whereby anti-NS1 provides protective activity. Anti-NS1 antibodies interact with protein NS1′, an elongated form of NS1 found in flaviviruses of the JEV serogroup [43], which is involved in neuroinvasion by WNV subtype Kunjin [44]. However, the mechanism involved remains unknown. It is likely that, in addition to interacting with NS1, anti-NS1 antibodies may block the in vivo deleterious activity of NS1′ in WNV and JEV infections. Understanding this interaction would open up new research avenues.
NS1 alone cannot induce a sterilizing immunity, but it contributes to the consolidation of flavivirus neutralizing immunity that is primarily elicited by protein E. Several vaccine candidates are known to provide better protection when NS1 is included in the vaccine preparation [38,45-50]. A recent study demonstrated the enhancement of anti-E antibody neutralization titer by mouse co-immunization of protein E with NS1, suggesting that NS1 might be usefully added to the viral structural components in a JEV vaccine [51].
A previous study showed that autoantibodies induced by DENV NS1 recognized coagulation factors including fibrinogen and platelets, as well as integrin/adhesion proteins [8]. Binding of anti-DENV NS1 antibodies to endothelial cells induced inflammation and apoptosis [10]. The possibility that other flaviviral NS1 proteins may elicit autoantibodies when used as components of a vaccine should not be underestimated. Whether JEV NS1 induced autoantibodies needs further study. However, JEV anti-NS1 antibodies did not bind to endothelial cells like DENV anti-NS1 antibodies did [10] and JEV infection does not cause hemorrhagic manifestations, minimizing the role of NS1-elicited autoantibodies.
In summary, immunization with a hexameric NS1 elicited Th2 and low Th1 cell responses, and induced a partial protective immune response in a mouse model. The ISA-51-VG adjuvant improved the performance of NS1 immunization by contributing to the production of higher antibody titers and increased the mouse survival rate. Passive transfer of sufficient anti-NS1 antibodies provided full protection to mice from lethal JEV challenge. However, anti-NS1 MAbs provided poor protection, although they significantly extended the survival period before death. These results support the hypothesis that anti-NS1 antibodies participate in immune protection against JEV infection.
Materials and Methods
Cells and viruses
Baby hamster kidney (BHK-21) cell lines were cultured in Dulbecco’s modified Eagle’s medium (DMEM, Invitrogen, Carlsbad, CA, USA) containing 3% fetal bovine serum (FBS), 100 U penicillin, and 100 μg streptomycin at 37 °C in 5% CO2. The JEV SA14 strain was obtained from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China). The attenuated vaccine strain JEV SA14-14-2 was obtained from the Chengdu Institute of Biological Products (Chengdu, China). BHK-21 cells were infected at a multiplicity of infection of 0.1 pfu cell–1. Drosophila S2 cells were purchased from Invitrogen (Carlsbad, CA, USA) and cultured in Schneider’s Drosophila medium (Invitrogen) with 10% FBS, 50 U penicillin, and 50 μg streptomycin, and incubated at 28 °C.
NS1 expression and purification from Drosophila S2 cells
NS1 protein expression and purification procedures were conducted according to previously published methods [27]. Briefly, the JEV Nakayama strain genes encoding the full-length 352 amino acids of NS1 and its fragments, containing N-terminus amino acids (1–143) and C-terminus amino acids (224–352), were amplified by RT-PCR and inserted into the pMT/Bip/V5-His A plasmid vector to produce pMT-NS11-352, pMT-NS11-143, and pMT-NS1224-352, respectively. Drosophila S2 cells were co-transfected with plasmids pMT-NS11-352, pMT-NS11-143, or pMT-NS1224-352, and pCoblast (Invitrogen). S2 cells were selected using blasticidin. To improve NS1 production, cell populations were cloned by limit dilution to generate an S2-NS1 cell clone expressing high levels of NS1. Cells were cultured in Express Five medium (Invitrogen) without FBS in a Wave Bioreactor™ (GE Amersham, Uppsala, Sweden). Cell supernatants were collected, filtered, and concentrated, and the buffer was exchanged. The resultant fluids containing NS1 were loaded onto a chelating sepharose column (GE Amersham). The column was washed with binding buffer and the recombinant protein was eluted. After nickel ion column chromatography, the protein was applied to a size exclusion Superdex 200 10/300 column using the AKTA Purifier System (GE Amersham).
Carbohydrate analysis of JEV NS1 secreted from Drosophila S2-NS1 cell clone
The NS1 denatured monomeric form was digested by Endoglycosidase H (Endo H) or Peptide: N-glycosidase F (PNGase F) (New England BioLabs, Beverley, MA, USA) according to the manufacturer’s instruction. Briefly, 3 μg of native or denatured NS1 were mixed with 6,000 units of Endo H or 7,000 units of PNGase F in reaction buffer, and incubated at 37 °C for 3 hr. After digestion, the reaction mixtures were added to equal volumes of 2 times loading buffer, heated at 95 °C for 5 min, and separated by 12.5% SDS-polyacrylamide gel electrophoresis (SDS-PAGE).
Glycosylation differentiation: The DIG glycan differentiation kit (Roche, Mannheim, Germany) was used for NS1 glycan differentiation. The NS1 proteins and control glycoproteins were transferred onto nitrocellulose membranes after gel electrophoretic separation. The membranes were incubated in blocking buffer for 1 hr, washed twice in TBS (Tris buffered saline) and once in buffer 1 (TBS; 1 mM MgCl2, 1 mM MnCl2, 1 mM CaCl2, pH 7.5) and incubated each 1 hr with digoxigenin-labeled GNA, SNA, MAA, and DSA. The membranes were washed three times with TBS, then anti-digoxigenin-alkaline phosphatase was added and incubated for 1 hr. The membranes were washed three times in distilled water and 1 ml of alkaline phosphatase substrate (Promega, San Luis Obispo, CA, USA) was added to each membrane for staining.
Western blotting
The NS1 protein sample was boiled at 95 °C for 5 min in a reducing SDS loading buffer, then separated by 10% SDS-PAGE. The protein was transferred to nitrocellulose membranes that were blocked with 5% non-fat milk in TBS/Tween-20 before being incubated with a 1:1000 dilution of anti-V5 tag or anti-NS1 MAbs. After washing, the membranes were incubated with a 1:3000 dilution of alkaline-phosphatase-conjugated secondary antibodies (Promega). Signals were detected based on the coloration of an alkaline phosphatase dark blue substrate (Promega).
Antibody titration
The anti-NS1 antibody titers were tested by ELISA. One hundred ng per well of purified NS1 protein was coated onto 96-well plates (Corning Costar, Lowell, MA, USA) that were incubated overnight at 4°C. Plates were washed and blocked with PBS/3% BSA. A series of 1:2 dilutions (from 1:100 to 1:204,800 in PBS/1% BSA) of mouse serum was added to the wells and incubated for 1 h at room temperature (RT). Plates were washed before adding horseradish-peroxidase-labeled goat anti-mouse IgG (H + L), IgG1, IgG2a, (Southern Biotech, Birmingham, AL, USA) that were diluted 5,000-fold. Plates were then incubated for 1 h at RT. The plates were washed again before adding ortho-phenyl diamine substrate (Sigma–Aldrich) and incubated for 10 min at RT. Enzymatic reactions were stopped with 3 M H2SO4 and absorbance was recorded at 492 nm using an ELISA plate reader (Molecular Devices, Sunnyvale, CA, USA)
Neutralizing antibody titers were determined in BHK cells. Pooled sera from each group were subjected to two fold dilutions in DMEM 2% FBS from 1:20 to 1:320 dilution,and mixed with 150 pfu (corresponding to 10 TCID50) of JEV SA14 virus in 96-well plates before incubating for 1 h at 37 °C, after which 6,000 BHK cells were added. The plates were read after 3 d, and the serum dilution that reduced 50% of the virus (TCID50) was recorded.
Lymphocyte proliferation and IFN-γ secretion
Two weeks after the 2nd inoculation of NS1, PBS, or six weeks after the inoculation of SA14-14-2, DMEM with 3% FBS (complete DMEM medium), three mice were killed from each group. Mouse spleens were isolated and crushed in cell strainers (Becton, Dickinson and Company, Franklin Lakes, NY, USA) to prepare splenocyte suspensions. Erythrocytes were lysed with red blood cell lysis solution (15.5 mM NH4Cl, 1 mM KHCO3, and 0.01 mM EDTA-2Na) and centrifuged at 500 × g, for five min, the cell pellet was washed three times then re-suspended in cell culture medium. The cell concentration of each mouse was counted and diluted to 4 × 106 cells ml–1 in RPMI 1640 medium with 10% heat-inactivated FBS to be used for lymphocyte proliferation and cytokine production assays [52]. Mouse splenocytes were cultured with 5 μg ml–1 of JEV NS1 protein. T-cell proliferation was quantified using the Cell Titer 96® Aqueous Non-Radioactive Cell Proliferation Assay (Promega), according to the manufacturer’s instructions. T-lymphocyte proliferation was measured using a stimulation index, which was expressed as the OD570 ratio of NS1-stimulated wells to that of wells without NS1 [53].
Splenocyte suspensions (0.5 ml) were dispensed into the wells of a 24-well cell culture plate. An equal volume of NS1 (10 μg ml–1) in medium was also added. Cells were incubated for 5 d. Cell culture supernatants were harvested and stored at −80°C before analysis. IFN-γ production was tested using a Mouse IFN-γ ELISA Kit (BD Pharmingen, San Diego, CA, USA), according to the manufacturers’ instructions [52].
Anti-NS1 MAb preparation and characterization
Anti-JEV MAb preparation followed a previously published method [27]. Briefly, MAbs were purified from hybridoma cultured supernatants or from mouse ascitic fluid using Protein A or Protein G columns (GE Amersham). Antibodies were characterized by flow cytometry to determine cell surface and intracellular NS1 recognition. Epitope mapping was performed using an ELISA or Western blotting with full-length, and N-terminus (amino acids 1–143) and C-terminus (amino acids 224–352) NS1 fragments [27].
Mouse immunization and challenge
The mouse experimental protocol was approved by the Institut Pasteur of Shanghai Ethics Committee for Animal Care (ID# 01–2006) and was conducted in the Institut Pasteur animal facility following the European directive 2010/63/EU on the protection of animals used for scientific purposes.
Four-week-old female C3H/HeN mice were purchased from Vital River, the Chinese representative of Charles River Laboratories (Vital River Lab Animal Technology Co., Ltd, Beijing, China). Mice were separated into four groups: a negative control group that received 200 μl of PBS i.p.; a positive control group that received one dose of 104 pfu JEV SA14-14-2 vaccine i.p.; an NS1 group that was injected with 1 μg of NS1 in 200 μl of PBS (aqueous NS1); and a group injected with 1 μg of NS1 emulsified with water-in-oil adjuvant by mixing NS1 in 100 μl of PBS with an equal volume of Montanide oil (ISA-51-VG, SEPPIC SA, Puteaux, France) in a latex-free syringe. All groups were immunized by the i.p. route with two doses of antigen four weeks apart. Mouse sera were collected two weeks after the second inoculation. Four weeks after the second inoculation, mice were transferred in isolators to a biosafety level 2 animal facility, where they were challenged by i.n. inoculation of 10 μl containing 104 pfu of SA14 virus in each nostril. Surviving mice sera were collected for antibody titration.
Mouse passive protection
Four-week-old mice were treated by i.p. transfer of 100 μl, 30μl, 10μl of pooled anti-NS1 mouse sera obtained from NS1-immunized mice containing an anti-NS1 antibody titer > 1:3000, or 100 μg or 500 μg of anti-NS1 MAbs. An HIV anti-envelop IgG1 MAb (a generous gift from Pr. Paul Zhou, Institut Pasteur of Shanghai) was used as an isotype control. Passive transfer of pooled anti-JEV antisera obtained from mice vaccinated with SA14-14-2 was used as a positive control. All sera were pre-incubated at 56°C for 30 min. One hour after the sera injection, mice were challenged with an injection of 20 pfu of JEV SA14. Mouse survival rates were calculated four weeks after the challenge.
Statistics
Cell proliferation, cytokine, and antibody titer data were analyzed by Excel and expressed as the mean ± SD. Survival analysis curves were analyzed using the log-rank test calculated by STATA version 11.1 (StataCorp, College Station, TX, USA). Figures were created using Sigmaplot (Systat Software, Inc., San Jose, CA, USA).
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conception of the study and design of the experiments: YL, VDe. Performance of the experiments: YL, CD, LP. Advice and assistance with the live-attenuated vaccine JEV: YY. Analysis of the data and statistics: YL, VDe, VDu. Writing of the paper: YL, VDe. All authors read and approved the final manuscript.
Supplementary Material
Figure S1. Characterization of carbohydrates of S2 cells expressing NS1. A: Purified NS1 protein was denatured and mock-treated (lane 1) or incubated with Endo H (lane 2) and PNGase F (lane 3) and the products were separated by SDS-PAGE. B: After electrophoresis, the GNA recognition control glycoprotein carboxypeptidase Y (arrow, lane 1), the DSA recognition control glycoprotein asialofetuin (lane 3), and NS1 protein (arrows, lanes 2 and 4) were transferred to a nitrocellulose membrane and incubated with digoxigenin-labeled GNA (lanes 1 and 2) or DSA (lanes 3 and 4) and further incubated with anti-digoxigenin alkaline phosphatase-labeled antibodies and with alkaline phosphatase substrate.
Figure S2. Susceptibility of C3H mice to JEV SA14 infection. Groups of six C3H mice infected with JEV SA14 were monitored daily for 28 days. Two groups of three-month-old C3H mice were infected with different doses of JEV SA14 by intraperitoneal (A) or intranasal (B) route. One group of one-month-old C3H mice was infected with different doses of JEV SA14 by intraperitoneal route (C).
Contributor Information
Yize Li, Email: yzli@sibs.ac.cn.
Dorian Counor, Email: dcounor@sibs.ac.cn.
Peng Lu, Email: lupeng0515@gmail.com.
Veasna Duong, Email: dveasna@pasteur-kh.org.
Yongxin Yu, Email: yuyongxin@nicpbp.org.cn.
Vincent Deubel, Email: vdeubel@pasteur-kh.org.
Acknowledgments
We wish to thank the Chengdu Institute of Biological Products (Chengdu, China) for sharing the JEV vaccine SA14-14-2. The JEV SA14 was obtained from the National Institute for the Control of Pharmaceutical and Biological Products, Beijing, China. We thank Mr Regis Vialle (SEPPIC SA) for providing ISA-51-VG adjuvant used in this study. We thank Pr. Paul Zhou (Institut Pasteur of Shanghai-Chinese Academy of Sciences) for providing anti-HIV MAb. We thank Prs. Ralf Altmeyer and Bing Sun for their interest and support of this study. D.C. was a recipient of an award from the Areva Foundation. This study was supported by the Shanghai Pasteur Health Research Foundation.
References
- Mackenzie JS. Emerging zoonotic encephalitis viruses: lessons from Southeast Asia and Oceania. J Neurovirol. 2005;11:434–440. doi: 10.1080/13550280591002487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers TJ, Hahn CS, Galler R, Rice CM. Flavivirus genome organization, expression, and replication. Annu Rev Microbiol. 1990;44:649–688. doi: 10.1146/annurev.mi.44.100190.003245. [DOI] [PubMed] [Google Scholar]
- Lindenbach BD, Rice CM. Genetic interaction of flavivirus nonstructural proteins NS1 and NS4A as a determinant of replicase function. J Virol. 1999;73:4611–4621. doi: 10.1128/jvi.73.6.4611-4621.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutsche I, Coulibaly F, Voss JE, Salmon J, D'Alayer J, Ermonval M, Larquet E, Charneau P, Krey T, Megret F. et al. Secreted dengue virus nonstructural protein NS1 is an atypical barrel-shaped high-density lipoprotein. Proc Natl Acad Sci USA. 2011;108:8003–8008. doi: 10.1073/pnas.1017338108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung KM, Liszewski MK, Nybakken G, Davis AE, Townsend RR, Fremont DH, Atkinson JP, Diamond MS. West Nile virus nonstructural protein NS1 inhibits complement activation by binding the regulatory protein factor H. Proc Natl Acad Sci USA. 2006;103:19111–19116. doi: 10.1073/pnas.0605668103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avirutnan P, Fuchs A, Hauhart RE, Somnuke P, Youn S, Diamond MS, Atkinson JP. Antagonism of the complement component C4 by flavivirus nonstructural protein NS1. J Exp Med. 2010;207:793–806. doi: 10.1084/jem.20092545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avirutnan P, Hauhart RE, Somnuke P, Blom AM, Diamond MS, Atkinson JP. Binding of flavivirus nonstructural protein NS1 to C4b binding protein modulates complement activation. J Immunol. 2011;187:424–433. doi: 10.4049/jimmunol.1100750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falconar AKI. The dengue virus nonstructural-1 protein (NS1) generates antibodies to common epitopes on human blood clotting, integrin/adhesin proteins and binds to human endothelial cells: potential implications in haemorrhagic fever pathogenesis. Arch Virol. 1997;142:897–916. doi: 10.1007/s007050050127. [DOI] [PubMed] [Google Scholar]
- Chang HH, Shyu HF, Wang YM, Sun DS, Shyu RH, Tang SS, Huang YS. Facilitation of cell adhesion by immobilized dengue viral nonstructural protein 1 (NS1): arginine-glycine-aspartic acid structural mimicry within the dengue viral NS1 antigen. J Infect Dis. 2002;186:743–751. doi: 10.1086/342600. [DOI] [PubMed] [Google Scholar]
- Lin CF, Lei HY, Shiau AL, Liu HS, Yeh TM, Chen SH, Liu CC, Chiu SC, Lin YS. Endothelial cell apoptosis induced by antibodies against dengue virus nonstructural protein 1 via production of nitric oxide. J Immunol. 2002;169:657–664. doi: 10.4049/jimmunol.169.2.657. [DOI] [PubMed] [Google Scholar]
- Jelinek T. Ixiaro: a new vaccine against Japanese encephalitis. Expert Rev Vaccines. 2009;8:1501–1511. doi: 10.1586/erv.09.112. [DOI] [PubMed] [Google Scholar]
- Hills SL, Griggs AC, Fischer M. Japanese encephalitis in travelers from non-endemic countries, 1973–2008. Am J Trop Med Hyg. 2010;82:930–936. doi: 10.4269/ajtmh.2010.09-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger JJ, Brandriss MW, Cropp CB, Monath TP. Protection against yellow fever in monkeys by immunization with yellow fever virus nonstructural protein NS1. J Virol. 1986;60:1153–1155. doi: 10.1128/jvi.60.3.1153-1155.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falgout B, Bray M, Schlesinger JJ, Lai CJ. Immunization of mice with recombinant vaccinia virus expressing authentic dengue virus nonstructural protein NS1 protects against lethal Dengue virus encephalitis. J Virol. 1990;64:4356–4363. doi: 10.1128/jvi.64.9.4356-4363.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnak JR, Schlesinger JJ. Protection of mice against yellow fever virus encephalitis by immunization with a vaccinia virus recombinant encoding the yellow fever virus nonstructural proteins, NS1, NS2a and NS2b. J Gen Virol. 1990;71:1697–1702. doi: 10.1099/0022-1317-71-8-1697. [DOI] [PubMed] [Google Scholar]
- Jacobs SC, Stephenson JR, Wilkinson GWG. Protection elicited by a replication-defective adenovirus vector expressing the tick-borne encephalitis virus nonstructural glycoprotein NS1. J Gen Virol. 1994;75:2399–2402. doi: 10.1099/0022-1317-75-9-2399. [DOI] [PubMed] [Google Scholar]
- Timofeev AV, Ozherelkov SV, Pronin AV, Deeva AV, Karganova GG, Elbert LB, Stephenson JR. Immunological basis for protection in a murine model of tick-borne encephalitis by a recombinant adenovirus carrying the gene encoding the NS1 non-structural protein. J Gen Virol. 1998;79(Pt 4):689–695. doi: 10.1099/0022-1317-79-4-689. [DOI] [PubMed] [Google Scholar]
- Schepp-Berglind J, Luo M, Wang D, Wicker JA, Raja NU, Hoel BD, Holman DH, Barrett AD, Dong JY. Complex adenovirus-mediated expression of West Nile virus C, PreM, E, and NS1 proteins induces both humoral and cellular immune responses. Clin Vaccine Immunol. 2007;14:1117–1126. doi: 10.1128/CVI.00070-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu SF, Liao CL, Lin YL, Yeh CT, Chen LK, Huang YF, Chou HY, Huang JL, Shaio MF, Sytwu HK. Evaluation of protective efficacy and immune mechanisms of using a non-structural protein NS1 in DNA vaccine against dengue 2 virus in mice. Vaccine. 2003;21:3919–3929. doi: 10.1016/S0264-410X(03)00310-4. [DOI] [PubMed] [Google Scholar]
- Timofeev AV, Butenko VM, Stephenson JR. Genetic vaccination of mice with plasmids encoding the NS1 non-structural protein from tick-borne encephalitis virus and dengue 2 virus. Virus Genes. 2004;28:85–97. doi: 10.1023/B:VIRU.0000012266.04871.ce. [DOI] [PubMed] [Google Scholar]
- Henchal EA, Henchal LS, Schlesinger JJ. Synergistic interactions of anti-NS1 monoclonal-antibodies protect passively immunized mice from lethal challenge with dengue-2 virus. J Gen Virol. 1988;69:2101–2107. doi: 10.1099/0022-1317-69-8-2101. [DOI] [PubMed] [Google Scholar]
- Schlesinger JJ, Foltzer M, Chapman S. The Fc portion of antibody to yellow fever virus NS1 is a determinant of protection against YF encephalitis in mice. Virology. 1993;192:132–141. doi: 10.1006/viro.1993.1015. [DOI] [PubMed] [Google Scholar]
- Chung KM, Nybakken GE, Thompson BS, Engle MJ, Marri A, Fremont DH, Diamond MS. Antibodies against West Nile virus nonstructural protein NS1 prevent lethal infection through Fc gamma receptor-dependent and -independent mechanisms. J Virol. 2006;80:1340–1351. doi: 10.1128/JVI.80.3.1340-1351.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung KM, Thompson BS, Fremont DH, Diamond MS. Antibody recognition of cell surface-associated NS1 triggers Fc-gamma receptor-mediated phagocytosis and clearance of West Nile virus-infected cells. J Virol. 2007;81:9551–9555. doi: 10.1128/JVI.00879-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCown J, Cochran M, Putnak R, Feighny R, Burrous J, Henchal E, Hoke C. Protection of mice against lethal Japanese encephalitis with a recombinant baculovirus vaccine. Am J Trop Med Hyg. 1990;42:491–499. doi: 10.4269/ajtmh.1990.42.491. [DOI] [PubMed] [Google Scholar]
- Konishi E, Pincus S, Fonseca BAL, Shope RE, Paoletti E, Mason PW. Comparison of protective immunity elicited by recombinant vaccinia viruses that synthesize E or NS1 of Japanese encephalitis virus. Virology. 1991;185:401–410. doi: 10.1016/0042-6822(91)90788-D. [DOI] [PubMed] [Google Scholar]
- Li YZ, Counor D, Lu P, Liang GD, Huong VT, Nga PT, Loan HT, Sun G, Grandadam M, Butrapet S. et al. A specific and sensitive antigen capture assay for NS1 protein quantitation in Japanese encephalitis virus infection. J Virol Methods. 2011;179:8–16. doi: 10.1016/j.jviromet.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Wang K, Deubel V. Mice with different susceptibility to Japanese encephalitis virus infection show selective neutralizing antibody response and myeloid cell infectivity. PLoS One. 2011;6:e24744. doi: 10.1371/journal.pone.0024744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modis Y, Ogata S, Clements D, Harrison SC. Structure of the dengue virus envelope protein after membrane fusion. Nature. 2004;427:313–319. doi: 10.1038/nature02165. [DOI] [PubMed] [Google Scholar]
- Abbas AK, Murphy KM, Sher A. Functional diversity of helper T lymphocytes. Nature. 1996;383:787–793. doi: 10.1038/383787a0. [DOI] [PubMed] [Google Scholar]
- Aucouturier J, Dupuis L, Deville S, Ascarateil S, Ganne V. Montanide ISA 720 and 51: a new generation of water in oil emulsions as adjuvants for human vaccines. Expert Rev Vaccines. 2002;1:111–118. doi: 10.1586/14760584.1.1.111. [DOI] [PubMed] [Google Scholar]
- Lin CW, Liu KT, Huang HD, Chen WJ. Protective immunity of Ecoli-synthesized NS1 protein of Japanese encephalitis virus. Biotechnol Lett. 2008;30:205–214. doi: 10.1007/s10529-007-9529-9. [DOI] [PubMed] [Google Scholar]
- Alcon-LePoder S, Drouet MT, Roux P, Frenkiel MP, Arborio M, Durand-Schneider AM, Maurice M, Le Blanc I, Gruenberg J, Flamand M. The secreted form of dengue virus nonstructural protein NS1 is endocytosed by hepatocytes and accumulates in late endosomes: implications for viral infectivity. J Virol. 2005;79:11403–11411. doi: 10.1128/JVI.79.17.11403-11411.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel N, Rong Q, Zimmerman D, Rosenthal KS. A L.E.A.P.S.TM heteroconjugate vaccine containing a T cell epitope from HSV-1 glycoprotein D elicits Th1 responses and protection. Vaccine. 2003;21:4410–4420. doi: 10.1016/S0264-410X(03)00429-8. [DOI] [PubMed] [Google Scholar]
- Murali-Krishna K, Ramireddy B, Ravi V, Manjunath R. Recognition of nonstructural protein-peptides by cytotoxic T lymphocytes raised against Japanese encephalitis virus. Microbiol Immunol. 1995;39:1021–1024. doi: 10.1111/j.1348-0421.1995.tb03294.x. [DOI] [PubMed] [Google Scholar]
- Murali-Krishna K, Ravi V, Manjunath R. Japanese encephalitis virus infection of mouse cell lines: ability to prime mice for generation of virus-specific cytotoxic T lymphocytes and differences in CTL recognizable viral determinants. Arch Virol. 1995;140:127–143. doi: 10.1007/BF01309728. [DOI] [PubMed] [Google Scholar]
- Xu G, Xu X, Li Z, He Q, Wu B, Sun S, Chen H. Construction of recombinant pseudorabies virus expressing NS1 protein of Japanese encephalitis (SA14-14-2) virus and its safety and immunogenicity. Vaccine. 2004;22:1846–1853. doi: 10.1016/j.vaccine.2003.09.015. [DOI] [PubMed] [Google Scholar]
- Konishi E, Ajiro N, Nukuzuma C, Mason PW, Kurane I. Comparison of protective efficacies of plasmid DNAs encoding Japanese encephalitis virus proteins that induce neutralizing antibody or cytotoxic T lymphocytes in mice. Vaccine. 2003;21:3675–3683. doi: 10.1016/S0264-410X(03)00382-7. [DOI] [PubMed] [Google Scholar]
- Chen HW, Pan CH, Liau MY, Jou R, Tsai CJ, Wu HJ, Lin YL, Tao MH. Screening of protective antigens of Japanese encephalitis virus by DNA immunization: a comparative study with conventional viral vaccines. J Virol. 1999;73:10137–10145. doi: 10.1128/jvi.73.12.10137-10145.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YL, Chen LK, Liao CL, Yeh CT, Ma SH, Chen JL, Huang YL, Chen SS, Chiang HY. DNA immunization with Japanese encephalitis virus nonstructural protein NS1 elicits protective immunity in mice. J Virol. 1998;72:191–200. doi: 10.1128/jvi.72.1.191-200.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tafuku S, Miyata T, Tadano M, Mitsumata R, Kawakami H, Harakuni T, Sewaki T, Arakawa T. Japanese encephalitis virus structural and nonstructural proteins expressed in Escherichia coli induce protective immunity in mice. Microbes Infect. 2012;14:169–176. doi: 10.1016/j.micinf.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Krishna VD, Rangappa M, Satchidanandam V. Virus-specific cytolytic antibodies to nonstructural protein 1 of Japanese encephalitis virus effect reduction of virus output from infected cells. J Virol. 2009;83:4766–4777. doi: 10.1128/JVI.01850-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth AE, Atkins JF. A conserved predicted pseudoknot in the NS2A-encoding sequence of West Nile and Japanese encephalitis flaviviruses suggests NS1' may derive from ribosomal frameshifting. Virol J. 2009;6:I4. doi: 10.1186/1743-422X-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melian EB, Hinzman E, Nagasaki T, Firth AE, Wills NM, Nouwens AS, Blitvich BJ, Leung J, Funk A, Atkins JF. et al. NS1' of flaviviruses in the Japanese encephalitis virus serogroup is a product of ribosomal frameshifting and plays a role in viral neuroinvasiveness. J Virol. 2010;84:1641–1647. doi: 10.1128/JVI.01979-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang YM, Hayes EP, McCarty TC, Dubois DR, Summers PL, Eckels KH, Chanock RM, Lai CJ. Immunization of mice with dengue structural proteins and nonstructural protein NS1 expressed by baculovirus recombinant induces resistance to dengue virus encephalitis. J Virol. 1988;62:3027–3031. doi: 10.1128/jvi.62.8.3027-3031.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray M, Zhao BT, Markoff L, Eckels KH, Chanock RM, Lai CJ. Mice immunized with recombinant vaccinia virus expressing dengue-4 virus structural proteins with or without nonstructural protein-NS1 are protected against fatal dengue virus encephalitis. J Virol. 1989;63:2853–2856. doi: 10.1128/jvi.63.6.2853-2856.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckels KH, Dubois DR, Summers PL, Schlesinger JJ, Shelly M, Cohen S, Zhang YM, Lai CJ, Kurane I, Rothman A. et al. Immunization of monkeys with baculovirus-dengue type-4 recombinants containing envelope and nonstructural proteins: evidence of priming and partial protection. Am J Trop Med Hyg. 1994;50:472–478. doi: 10.4269/ajtmh.1994.50.472. [DOI] [PubMed] [Google Scholar]
- Hall RA, Nisbet DJ, Pham KB, Pyke AT, Smith GA, Khromykh AA. DNA vaccine coding for the full-length infectious Kunjin virus RNA protects mice against the New York strain of West Nile virus. Proc Natl Acad Sci USA. 2003;100:10460–10464. doi: 10.1073/pnas.1834270100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang DK, Kweon CH, Kim BH, Lim SI, Kwon JH, Kim SH, Song JY, Han HR. Immunogenicity of baculovirus expressed recombinant proteins of Japanese encephalitis virus in mice. J Vet Sci. 2005;6:125–133. [PubMed] [Google Scholar]
- Watts DM, Tesh RB, Siirin M, Rosa AT, Newman PC, Clements DE, Ogata S, Coller BA, Weeks-Levy C, Lieberman MM. Efficacy and durability of a recombinant subunit West Nile vaccine candidate in protecting hamsters from West Nile encephalitis. Vaccine. 2007;25:2913–2918. doi: 10.1016/j.vaccine.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa T, Wang G, Widman DG, Infante E, Winkelmann ER, Bourne N, Mason PW. Enhancing the utility of a prM/E-expressing chimeric vaccine for Japanese encephalitis by addition of the JEV NS1 gene. Vaccine. 2011;29:7444–7455. doi: 10.1016/j.vaccine.2011.07.058. [DOI] [PubMed] [Google Scholar]
- Lieberman MM, Clements DE, Ogata S, Wang G, Corpuz G, Wong T, Martyak T, Gilson L, Coller BA, Leung J. et al. Preparation and immunogenic properties of a recombinant West Nile subunit vaccine. Vaccine. 2007;25:414–423. doi: 10.1016/j.vaccine.2006.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu JH, Chiang CC, Ng ML. Immunization of flavivirus West Nile recombinant envelope domain III protein induced specific immune response and protection against West Nile virus infection. J Immunol. 2007;178:2699–2705. doi: 10.4049/jimmunol.178.5.2699. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Characterization of carbohydrates of S2 cells expressing NS1. A: Purified NS1 protein was denatured and mock-treated (lane 1) or incubated with Endo H (lane 2) and PNGase F (lane 3) and the products were separated by SDS-PAGE. B: After electrophoresis, the GNA recognition control glycoprotein carboxypeptidase Y (arrow, lane 1), the DSA recognition control glycoprotein asialofetuin (lane 3), and NS1 protein (arrows, lanes 2 and 4) were transferred to a nitrocellulose membrane and incubated with digoxigenin-labeled GNA (lanes 1 and 2) or DSA (lanes 3 and 4) and further incubated with anti-digoxigenin alkaline phosphatase-labeled antibodies and with alkaline phosphatase substrate.
Figure S2. Susceptibility of C3H mice to JEV SA14 infection. Groups of six C3H mice infected with JEV SA14 were monitored daily for 28 days. Two groups of three-month-old C3H mice were infected with different doses of JEV SA14 by intraperitoneal (A) or intranasal (B) route. One group of one-month-old C3H mice was infected with different doses of JEV SA14 by intraperitoneal route (C).