Abstract
We evaluated the feasibility of using the modified Brazilian disk test to measure the post-dentin interfacial bond strength. Advanced nondestructive examination and imaging techniques in the form of acoustic emission (AE) and digital image correlation (DIC) were used innovatively to capture the fracture process in real time. DIC showed strain concentration first appearing at one of the lateral sides of the post-dentin interface. The appearance of the interfacial strain concentration also coincided with the first AE signal detected. The new method has the advantages of simpler specimen preparation, no premature failure, more consistent failure mode and smaller variations in the calculated bond strength.
1. Introduction
Many factors affect the prognosis of endodontically treated teeth. Among them, post loosening and root fracture were the most common reasons that cause failure [1]. Both events are caused by excessive forces, either at the tooth-restoration interface or in the tooth tissue itself. Actually, the two are related, with loosening of the restoration being one of the main factors that cause root fracture. This is confirmed by finite element analysis, which shows that interfacial failure between the post and tooth will significantly increase the stress in the tooth and, hence, the risk of root fracture [2]. Following post loosening, the post-core-crown-tooth structure will no longer be able to function as a single unit in sustaining the occlusal load [3]. Therefore, ensuring adequate bond strength between the post and dentin is paramount for endodontic treatments to be successful. Interfacial debonding is also responsible for the failure of other forms of restoration, e.g. secondary caries in composite restorations due to colonization of acid-producing bacteria within the compromised interface.
There are many different mechanical test methods available for measuring the bond strength between intracanal filling materials and dentin, for example, the microtensile bond test, pull-out test, and push-out test [4]. The main disadvantages of the microtensile bond test, which uses extensively machined specimens with a complex shape, include a high percentage of premature specimen failure and non-uniform stress patterns. These lead to a large variability in the test results [5]. In contrast, the push-out test is reported to have a more homogenous stress distribution and less variability in the measured data. With this method, the bond strength can be calculated by simply dividing the maximum recorded force by the area of the bonded interface [6]. Consequently, the push-out test has become a popular method to measure the bond strength of intracanal filling materials. However, there are factors other than the bond strength that can greatly affect the force needed to push out the filling, one of them being friction between the post and dentin [7, 8]. Therefore, the bond strength measured using the push-out test may be overestimated [9]. In order to more precisely measure the bond strength of intracanal filling, an alternative test method seems necessary. In an ideal test, the final failure should follow immediately the initiation of debonding at the post-dentin interface. This will allow the bond strength to be determined accurately from the well-defined final failure load.
The diametral compression or Brazilian disc test has been a popular experimental method for measuring the tensile strength of brittle materials. The stress distribution and failure mechanism have been thoroughly discussed by others [10]. There have been several modifications and extensions of this test method. For example, [11] used sandwiched discs to measure the interfacial fracture toughness of bone-cement interface, while the elastic stress field of a layered cylinder under diametral compression has been analyzed by [12].
Here, we propose a novel method based on a modified specimen for the diametral compression test: a disk containing an intracanal post in the center surrounded by dentin and then composite resin (Fig 1). The purpose of this study was to evaluate the feasibility of using such a specimen under diametral compression to measure the post-dentin interfacial bond strength. The hypothesis was that we could use this test to calculate the interfacial bond strength between the post and dentin easily from the final failure force. To test this hypothesis, we used acoustic emission (AE) and digital image correlation (DIC) to detect and monitor the initiation and propagation of interfacial failure, and to establish its relationship with the final fracture of the disc.
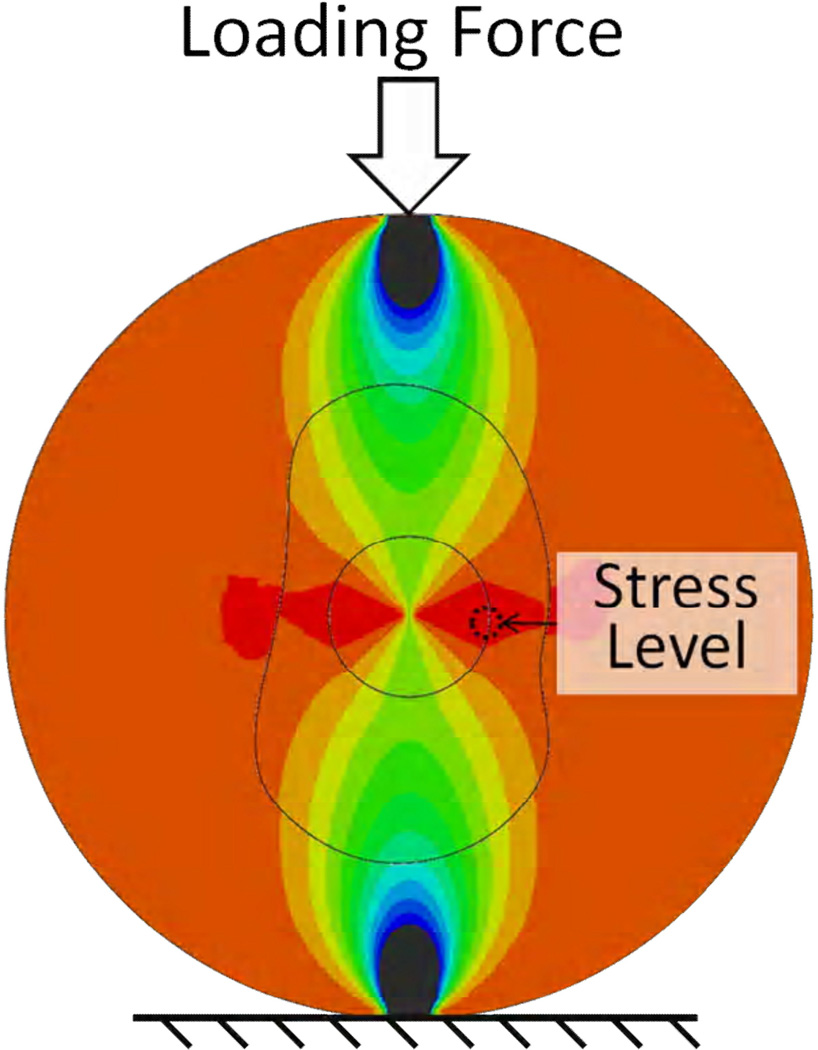
Figure 1.
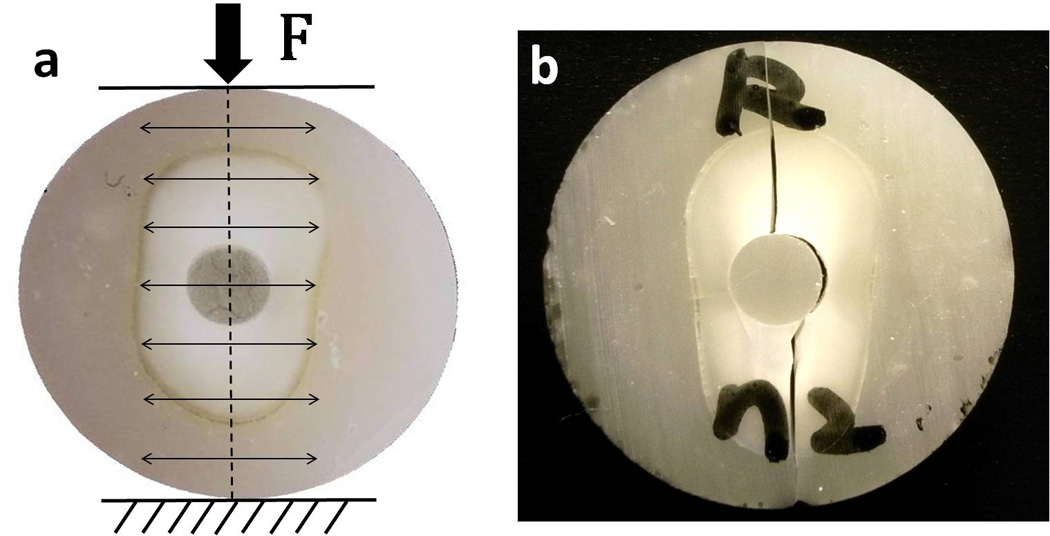
(a) Schematic view of the modified diametral compression test. (b) A typical fracture pattern of the disk specimen after test.
2. Materials and Methods
2.1 Samples preparation
Thirty-two extracted human single-canal teeth, previously stored in 4°C chloramines (0.5%), were used to prepare the specimens. Any soft tissue on the root surface was removed with scaling and curettage. Teeth with caries or cracks were excluded. The crown portion above the cementum-enamel junction and 5mm apical were cut off with a low-speed diamond saw (Isomet, Buehler, Lake Bluff, IL, USA). Root canals were prepared with the standard endodontical protocol. A 2mm parallel post space was created with a lower speed drill.
The teeth were divided into 4 groups of 8, which contained glass-fiber posts (RelyXTM Fiber Posts, 3M, St. Paul, MN, USA), stainless-steel posts, direct resin fillings (Z250, 3M ESPE) and no restorations, respectively. The posts were cemented with resin cement (AdperTM Single Bond Plus, 3M; RelyXTM ARC Adhesive Resin Cement, 3M), following the manufacturer’s protocol. The teeth were potted with resin (Z250, 3M ESPE) in a customized device to fabricate 10mm-diameter rods with the posts centrally located (Fig. 2). One tooth from each group was scanned using micro-CT (XT H 255, X-Tek, UK) to evaluate the quality of post restoration. An additional group of composite resin rods with no teeth were used to determine the tensile strength of the composite. All the rods were sliced into 2-mm thick disks, and then stored in de-ionized water for 7 days before testing.
Figure 2.

Customized PTFE device for sample preparation. The post was inserted into the central hole to make sure it is concentric with the outer ring.
2.2 Experimental setup for determination of failure procedure
The diametral compression test was conducted on a universal test machine (858 Mini Bionix II, MTS, USA) with two parallel horizontal planes. The load was applied under stroke-control at a rate of 0.5 mm/min until the specimen fractured. Test data, including the time histories of displacement and load, were recorded. In addition, nondestructive techniques in the form of acoustic emission (AE) and digital image correlation (DIC) were used to monitor the fracture process. The acoustic emission system (Physical Acoustics Corporation, NJ, USA) was used to detect signals produced from micro-cracking while the specimens were being loaded. AE sensors were attached to the lower stationary plate on which the specimen was placed. Signals detected by the sensors were passed through a preamplifier of 40 dB gain with a band pass of 100 kHz to 2MHz and a threshold set at 35 dB. Previous studies showed that setting the threshold at 35dB could successfully eliminate the background noise from the AE signals [13, 14]. The data obtained from the AE and universal test machine were used in combination to determine when cracking at the tooth-restoration interface and final failure occurred. The DIC technique was used to measure the change in strain on the surface of the specimen during the whole loading history. The system included a high-speed CCD camera and proprietary software for displacement and strain calculations (DaVis 7.0, LaVision, Germany). The surface of the specimen facing the CCD camera was sprayed with a fine layer of black paint to produce irregular-shaped speckles for ease of displacement tracking. Photographs were taken continuously at a rate of 10–20 fps throughout the test and subsequently analyzed by the DIC software. The whole test setup is illustrated in Fig 2b.
2.3 Bond strength and tensile strength calculation
Using finite element (FE) analysis, the relationship between the post-dentin interfacial tensile stress and the applied force to the disk was established. The post-dentin bond strength could then be calculated using the final failure force. In the same way, the tensile strength of dentin and resin could be determined from specimens with no fillings and those of composite resin only, respectively. 3D finite element models were used to simulate the disks (Fig. 3a). Example geometries of the models were obtained from micro-CT images of actual specimens, which were converted to FE meshes using the commercial software Amira (version 4.1, Mercury Computer Systems, Berlin, Germany). The materials were assumed to be homogeneous, linear elastic and isotropic (or transversely isotropic for the fiber post), with properties as shown in Table 1. Coulomb friction was assumed between the loading plate and the specimen, and the frictional coefficient was taken to be 0.3. The models were analyzed using the commercial software ABAQUS (version 6.10, Rising Sun Mills, Providence, RI, USA). Fig. 3 shows the FE model and radial stress distribution for a disk specimen with a direct resin filling. It contained 207,774 nodes and 4,800 6-noded prismatic and 186,820 8-noded brick elements. The bond strength was calculated from the maximum tensile stress at the post-dentin interface, as indicated in Fig. 3b, using the load at failure. In order to compare the difference in bond strength between the different groups with posts, the data were analyzed by the two-tailed T-test. All statistical tests were carried out at a 0.05 significance level.
Figure 3.
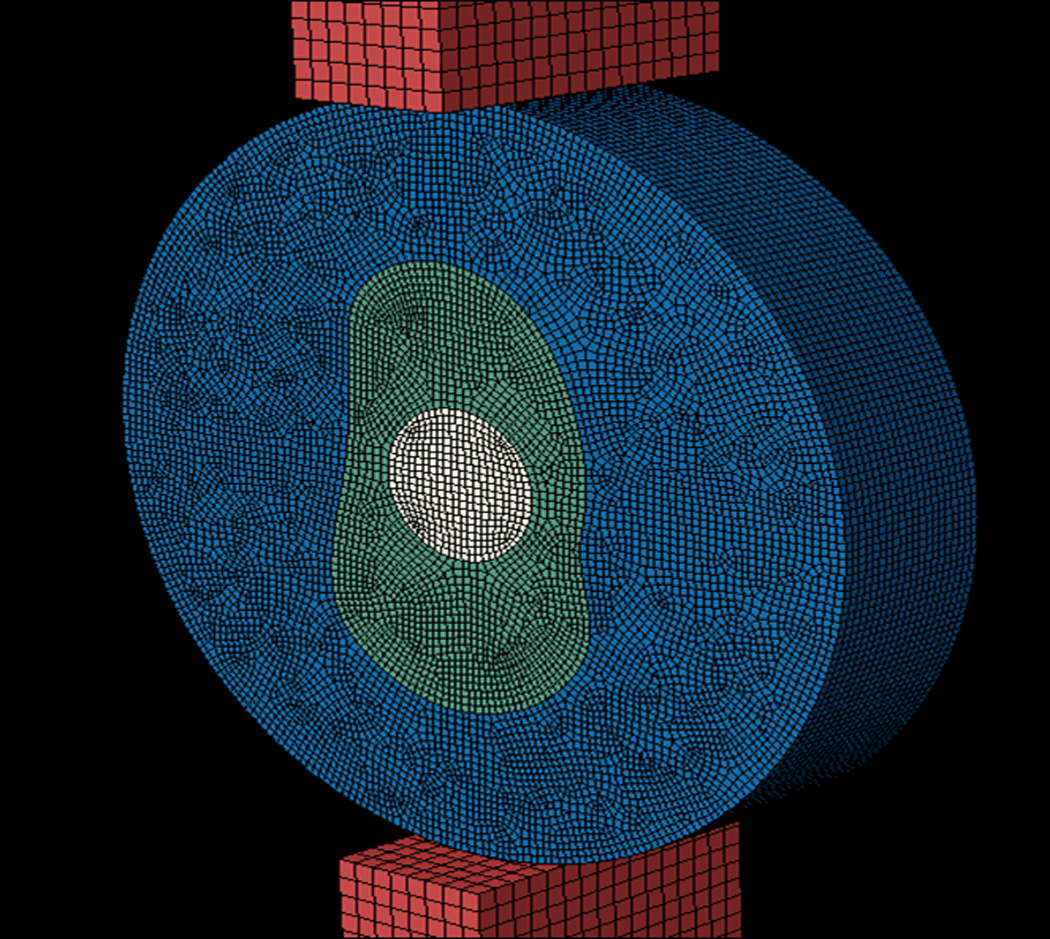
FE model (a) and radial stress distribution (b) for disk with direct resin filling.
Table 1.
Materials properties required for FE analysis
3. Results
3.1 Results of serial image correlation
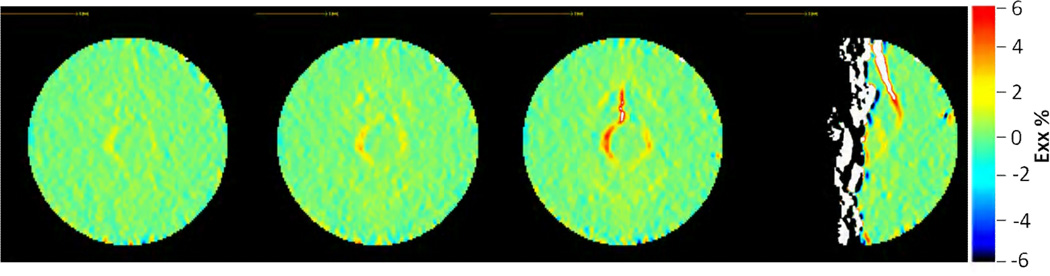
In so far as the fracture patterns are concerned, most specimens fractured along the central vertical diameter and around the interface between the post and dentin (Fig. 1); only two specimens from the fiber-post group fractured along the outer dentin-resin interface and they were excluded from the calculation. From the serial image correlation results, it could be clearly seen that a strain concentration first appeared on one of the lateral sides of the post-dentin interface, and then extended to the top and bottom of the interface before fast fracture occurred (Fig. 4). The whole process happened within 1–20 frames, i.e. less than one second. The emergence and extension of this strain concentration was the direct result of debonding along the post-dentin interface.
Figure 4.
Successive strain maps during loading obtained by DIC. Emergence and extension of strain concentration showing the development of debonding at the post-dentin interface followed by final fracture.
3.2 Relation of load-displacement curves and acoustic emission
In the plot of load and acoustic emission signals against time (Fig. 5), the first AE signal preceded or coincided with the final fracture, indicated by the first drop in load. The subsequent rise and the second drop in load corresponded to the loading and fracture of the separated half disks. Thus, the final fracture occurred almost immediately following the first AE event. When compared with the image correlation data, the first AE signal was seen to coincide with the first appearance of the strain concentration at the post-dentin interface. The first AE signal therefore indicated the initiation of interfacial debonding. It follows that, for most specimens, debonding at the post-dentin interface was followed quickly by the final fracture of the disk.
Figure 5.
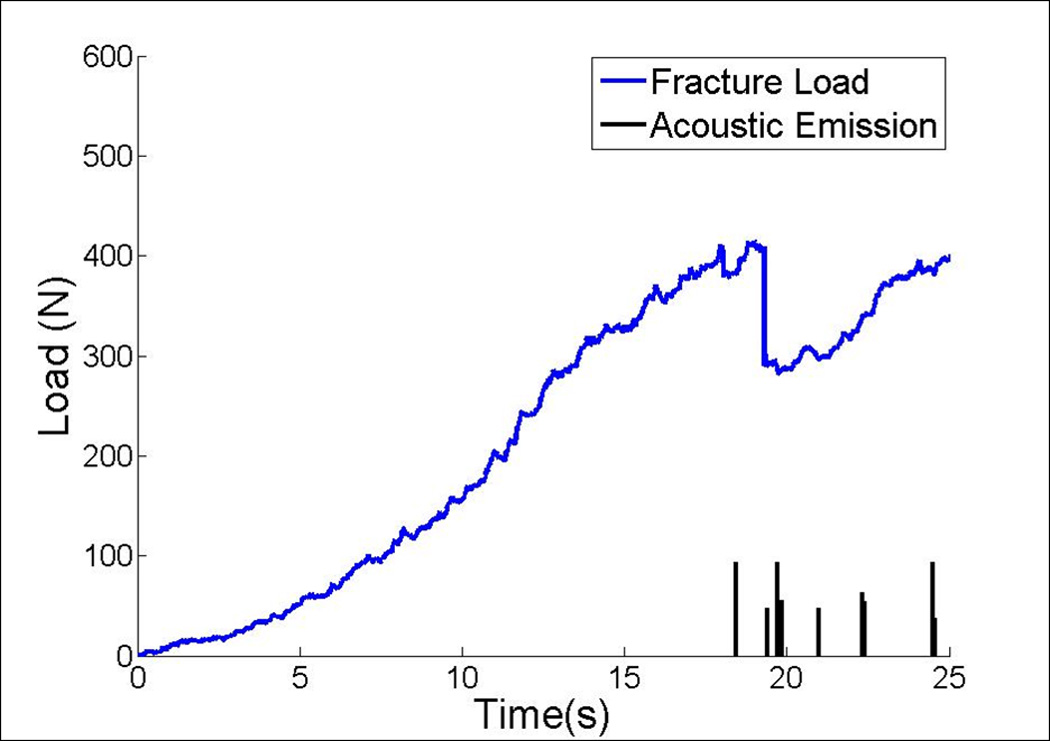
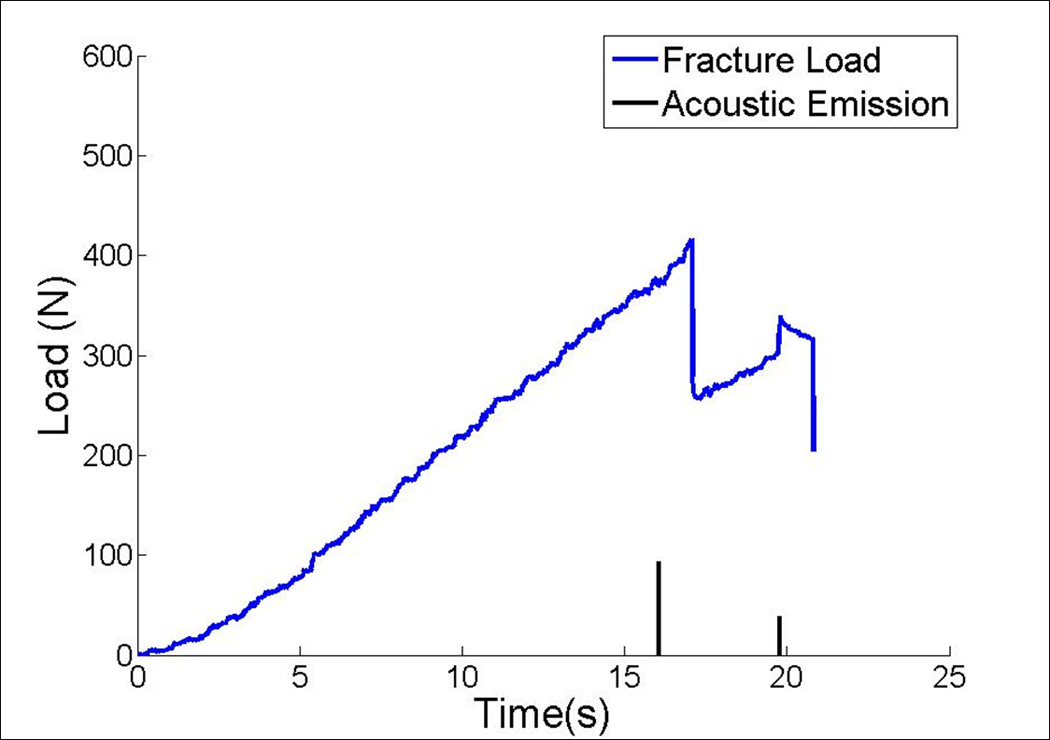
Typical load against time curves with acoustic emission (AE) events. (a) First AE signal occurred at the point of fracture. (b) First AE signal occurred just before final fracture.
3.3 Bond strength and tensile strength
The bond strengths, as calculated from the final failure data and the finite element analysis, are shown in Table 2. The results showed that the bond strength of the direct resin-filling group (8.88±1.57 MPa) was significantly lower than those of the fiber- and metal-post groups (11.16±2.40 & 12.85±3.99 MPa, respectively) (p<0.001). However, there was no statistically significant difference between the two post groups (p=0.062). The tensile strength of composite resin Z250 and dentin, as determined by testing the monolithic resin disks and dentin specimens with no fillings, respectively, under diametral compression, are also given in Table 3. The measured tensile strength of Z250 was 46.97±7.18 MPa and that of dentin was 82.56±38.22 MPa.
Table 2.
Mean and standard deviation of bond strength of the three post groups (n=sample size)
| Groups | Mean | SD | Coefficients of Variation |
|---|---|---|---|
| Fiber post (n=24) |
11.16a | 2.40 | 21.51% |
| Direct resin fillings (n=25) |
8.88b | 1.57 | 17.68% |
| Metal post (n=24) |
12.85a | 3.99 | 31.05% |
Subgroups with the same letter superscripts are not significantly different
Table 3.
Mean and standard deviation of tensile strength of dentin and composite resin (n=sample size)
| materials | Mean | SD | Coefficients of Variation |
|---|---|---|---|
| Z250 composite resin (n=14) |
46.97 | 7.18 | 15.29% |
| Human Dentin (n=21) |
82.56 | 38.22 | 46.29% |
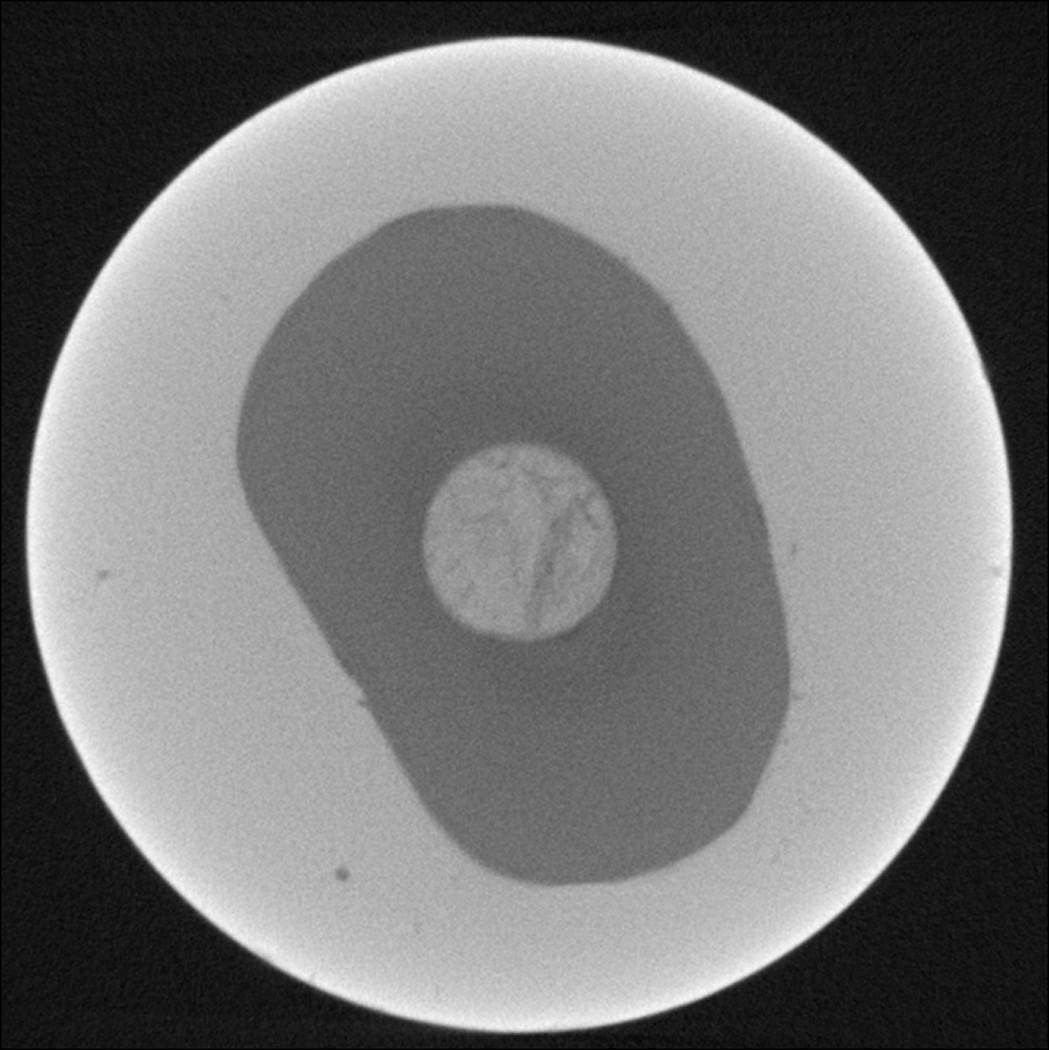
3.4 Micro-CT images
The micro-CT images showed that there were many voids or gaps at the post-dentin interface of specimens in the direct resin-filling group (Fig 6a). In the metal- or fiber-post groups, on the other hand, the post, resin cement and dentin had very good integration (Fig 6b).
Figure 6.
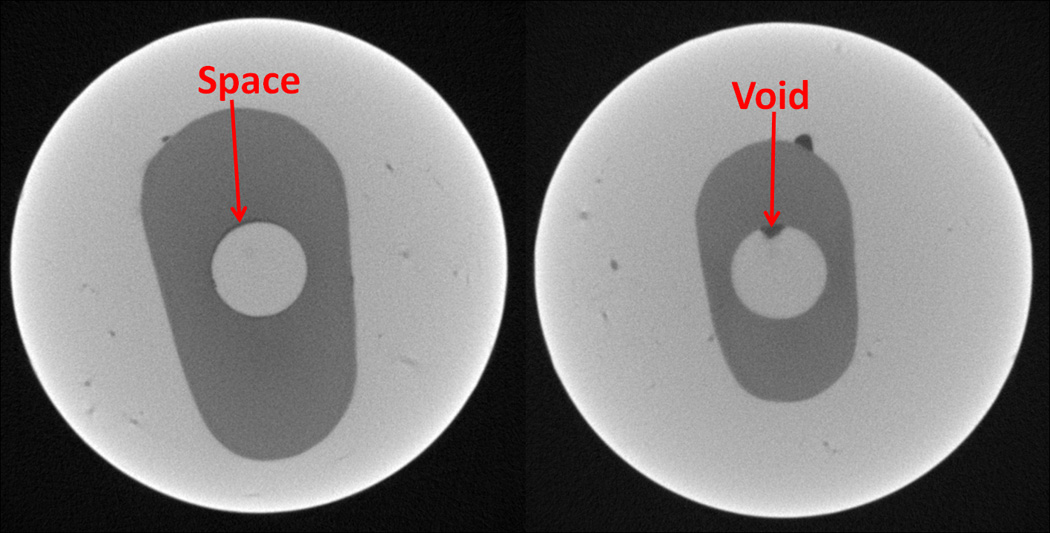
a. Micro-CT images of specimens with direct resin-filling showing the void and gap space between resin and dentin.
b. Micro-CT image of specimen with a fiber post showing good integration between the post and dentin.
4. Discussion
The results of this study demonstrated that the interfacial bond strength between endodontic posts and dentin could be measured using the diametral compression test with a modified disk specimen. One of the requirements for this test to be applicable is that the material or specimen must fail in a brittle manner. From the load-displacement curves (Fig. 5), which are rather linear up to the point of fracture, we can see that the specimens we used were brittle. Another requirement for using the test is that the disk diameter-to-thickness ratio should be larger than 4 [15]. This ratio was 5 for our specimens. There had been concern that fracture of the disks was simply caused by the high tangential stresses in the dentin, with interfacial debonding playing no part in the fracture initiation process. This was shown not to be the case by the use of image correlation, which clearly showed, through the evolution of surface strain maps, the initiation and propagation of debonding at the post-dentin interface prior to final fracture. Together with the load and acoustic emission data, the results showed that whole-specimen fracture followed almost immediately failure at the post-dentin interface. Therefore, it was reasonable to calculate the interfacial bond strength from the final failure force, and the hypothesis of this study was proven and accepted.
As discussed previously, post loosening and tooth fracture are the two main causes for failure of endodontically treated teeth, with the former possibly being the precursor to the latter. Both of these phenomena, i.e. interfacial debonding and dentin fracture, were involved in the failure of the disk in diametral compression, and in the same order, which makes this test more relevant to the clinical situation than the other test methods.
Stainless steel posts, fiber posts and direct resin fillings were chosen for this study. The bond strength values calculated for these materials interfacing with dentin were comparable with those reported in other studies [9, 16]. Further, the coefficients of variation of the bond strength values in our study (22% in the fiber-post group) were smaller than those provided by other methods, e.g. the microtensile test (85%) and the micro-push-out test (55%) [5]. This was attributed to the simpler specimen shape and, thus, the smaller amount of machining required to fabricate the specimens. Consequently, the presence of defects resulting from machining could be minimized. More importantly, the post-dentin interface of the disk specimen forms a smooth, closed loop surrounded completely by materials. In contrast, specimens such as those for micro-tensile and shear bond tests have their interface terminating abruptly at the free surfaces. These are places where localized stress concentrations, that are very sensitive to surface finishing and significantly contribute to the variation in bond strength, can exist. Another advantage of this experimental method is that it can also be used to test the tensile strength of dentin and monolithic composite resin. The strength of dentin obtained from the group of specimens with no posts was within the range of values reported in other studies (104±27.6MPa [17] and 86.6±18.8MPa [14]).
Comparing the three groups with restoration showed that the bond strength of specimens with direct resin fillings was significantly lower than the other two post groups. This can be explained by considering the effect of polymerization shrinkage. The volume of the direct resin filling was much greater than the layer of resin cement surrounding the posts. Therefore, it had probably produced more shrinkage stress following polymerization and thus reduced the bond strength [18]. Another reason was difficulty associated with the restorative procedures: it was not easy to apply evenly the adhesive agent and filling resin within the long tubular space. Therefore, more voids and gaps were seen within the direct resin-fillings group, as shown in the CT images (Fig. 6a). These operative defects must have reduced the bond strength of this group significantly. To minimize these defects, resin composite could be placed after the disks are machined out from the cylindrical column. The difference in bond strength between the metal post and fiber post groups were not statistically significant, possibly because they both used indirect restorations and the same cement.
Most bond strength test methods assume the measured bond strength to be independent of the other material properties. However, the mismatch in elastic modulus between the two substrates will cause stress concentration at the interface, especially on the free surfaces. Therefore, posts with a higher modulus and thus a higher stress concentration can have their bond strength underestimated if this effect is not taken into account [19, 20]. With the disk in diametral compression proposed in this study, the interfacial bond strength was calculated using experimental data and numerical results from the finite element analysis. The finite element analysis would already have considered the effect of any elastic modulus mismatch between the post and dentin on the interfacial stress distribution. As a result, we have minimized any uncertainty in the measured bond strength associated with such an effect. This might be the reason why the bond strengths obtained for the metal- and fiber-post groups, which used the same adhesive cement, were not significantly different.
Most of the specimens with restoration tested in this study fractured from the post-dentin interface, but two specimens fractured from the point of loading. Most brittle materials fracture more easily in tension than in compression [21], so fracture from the loading points, which were under a high level of compressive stress, could be unexpected. However, the highly localized contacts between the flat plates and the round disk do indeed produce high tensile and shear stresses that can exceed the material’s strength and induce fracture. There are modifications to the test configuration that can help reduce the contact stresses at the loading points; for example, using a curved loading plate or flattening the disk surface at the loading points [10]. These modifications to prevent failure at the loading points will be considered in future studies.
A major disadvantage of the method proposed here is that finite element analysis is required to calculate the bond strength from the failure load. The same mechanical properties for dentin were assumed for all the specimens in our analysis. It is recognized that deviations from these assumed values, due to natural variations in tooth properties, could introduce errors to the calculated bond strength values. However, the smaller standard deviations in the results produced by the new method indicated that these errors were probably smaller than those encountered in the other bond tests. In a follow-up paper, more detailed solutions will be provided linking the interfacial stress with the external load to assist researchers with the bond strength calculation. The effects of the mismatch in elastic modulus, errors in the assumed material properties, and the size and shape of the dentin layer will also be considered to assess the uncertainties in the estimated bond strength.
The present study considered only debonding under a monotonically increasing load, whereas most clinical failures are caused by cyclic fatigue loadings. The effect of shrinkage in the adhesive cement and composite resin has also not been fully considered. Despite these limitations, we have established the feasibility of using the composite disk in diametral compression to measure the bond strength between intracanal posts and dentin. In addition, we have shown that the new specimen can also be used for measuring the bond strength of direct filling materials such as composite resins. Compared to those used for the micro-tensile or shear bond tests, the new specimen shape is also closer to that of an actual composite restoration. We can therefore readily use it to assess the effects of other clinical challenges such as shrinkage stress, the resulting partial debonding, micro-leakage, thermal and mechanical cycling, or even the interaction with biofilms on the degradation of the tooth-restoration interface.
5. Conclusions
Failure of the modified disk in diametral compression was shown to be caused by debonding at the post-dentin interface. The final failure load can be used directly to calculate the bond strength.
The test can also be used for measuring the tensile strength of dentin and monolithic composite resin. The advantages of this new method include simpler specimen preparation, no premature specimen failure, more consistent failure mode, and smaller variations in the calculated bond strength.
Supplementary Material
Acknowledgements
This study was supported by the Minnesota Dental Research Center for Biomaterials and Biomechanics, 3M ESPE Company, NIH (Grant 1R01DE021366-01) and National Science Council of Taiwan (Grant No.NSC98-2917-I-002-146). The authors would also like to thank Dr Scott B. McClanahan, Director of the Division of Endodontics at the University of Minnesota School of Dentistry, for providing the restorative materials for sample preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ingle JI, Bakland LK, Baumgartner JC. Ingle's Endodontics. 6th ed. BC: Decker Inc; 2008. [Google Scholar]
- 2.Santos AFV, et al. Can Fiber Posts Increase Root Stresses and Reduce Fracture? Journal of Dental Research. 2010;89:587–591. doi: 10.1177/0022034510363382. [DOI] [PubMed] [Google Scholar]
- 3.Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endodontic Topics. 2006;13:57–83. [Google Scholar]
- 4.Goracci C, Grandini S, Bossu M, Bertelli E, Ferrari M. Laboratory assessment of the retentive potential of adhesive posts: a review. J Dent. 2007;35:827–835. doi: 10.1016/j.jdent.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Soares CJ, Santana FR, Castro CG, Santos-Filho PCF, Soares PV, Qian F, Armstrong SR. Finite element analysis and bond strength of a glass post to intraradicular dentin: Comparison between microtensile and push-out tests. Dental Materials. 2008;24:1405–1411. doi: 10.1016/j.dental.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Nomoto R, Carrick TE, McCabe JF. Suitability of a shear punch test for dental restorative materials. Dental Materials. 2001;17:415–421. doi: 10.1016/s0109-5641(00)00101-9. [DOI] [PubMed] [Google Scholar]
- 7.Lin G, Geubelle PH, Sottos NR. Simulation of fiber debonding with friction in a model composite pushout test. International Journal of Solids and Structures. 2001;38:8547–8562. [Google Scholar]
- 8.Chandra N, Ghonem H. Interfacial mechanics of push-out tests: theory and experiments. Composites Part A: Applied Science and Manufacturing. 2001;32:575–584. [Google Scholar]
- 9.Goracci C, et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. European Journal of Oral Sciences. 2004;112:353–361. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 10.Fahad MK. Stresses and failure in the diametral compression test. Journal of Materials Science. 1996;31:3723–3729. [Google Scholar]
- 11.Tong J, Wong KY, Lupton C. Determination of interfacial fracture toughness of bone-cement interface using sandwich Brazilian disks. Engineering Fracture Mechanics. 2007;74:1904–1916. doi: 10.1016/j.engfracmech.2006.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davison TS, Wadley HNG, Pindera M-J. Elastic response of a layered cylinder subjected to diametral loading. Composites Engineering. 1994;4:995–1009. [Google Scholar]
- 13.Kamst GF, Vasseur J, Bonazzi C, Bimbenet JJ. A new method for the measurement of the tensile strength of rice grains by using the diametral compression test. Journal of Food Engineering. 1999;40:227–232. [Google Scholar]
- 14.Procopio AT, Zavaliangos A, Cunningham JC. Analysis of the diametrical compression test and the applicability to plastically deforming materials. Journal of Materials Science. 2003;38:3629–3639. [Google Scholar]
- 15.Jonsén P, Häggblad HÅ, Sommer K. Tensile strength and fracture energy of pressed metal powder by diametral compression test. Powder Technology. 2007;176:148–155. [Google Scholar]
- 16.Zicari F, et al. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008;24:967–977. doi: 10.1016/j.dental.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Sano H, Ciucchi B, Matthews WG, Pashley DH. Tensile Properties of Mineralized and Demineralized Human and Bovine Dentin. Journal of Dental Research. 1994;73:1205–1211. doi: 10.1177/00220345940730061201. [DOI] [PubMed] [Google Scholar]
- 18.Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH. Geometric Factors Affecting Dentin Bonding in Root Canals: A Theoretical Modeling Approach. Journal of endodontics. 2005;31:584–589. doi: 10.1097/01.don.0000168891.23486.de. [DOI] [PubMed] [Google Scholar]
- 19.Perdigao J, Geraldeli S, Lee IK. Push-out bond strengths of tooth-colored posts bonded with different adhesive systems. American journal of dentistry. 2004;17:422–426. [PubMed] [Google Scholar]
- 20.Bitter K, Priehn K, Martus P, Kielbassa AM. In vitro evaluation of push-out bond strengths of various luting agents to tooth-colored posts. The Journal of prosthetic dentistry. 2006;95:302–310. doi: 10.1016/j.prosdent.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Sathorn C, Palamara JE, Messer HH. A comparison of the effects of two canal preparation techniques on root fracture susceptibility and fracture pattern. J Endod. 2005;31:283–287. doi: 10.1097/01.don.0000140580.03121.61. [DOI] [PubMed] [Google Scholar]
- 22.Peyton FA, Mahler DB, Hershenov B. Physical properties of dentin. J Dent Res. 1952;31:366–370. doi: 10.1177/00220345520310031401. [DOI] [PubMed] [Google Scholar]
- 23.Chung SM, Yap AU, Koh WK, Tsai KT, Lim CT. Measurement of Poisson's ratio of dental composite restorative materials. Biomaterials. 2004;25:2455–2460. doi: 10.1016/j.biomaterials.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 24.Lanza A, Aversa R, Rengo S, Apicella D, Apicella A. 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent Mater. 2005;21:709–715. doi: 10.1016/j.dental.2004.09.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.