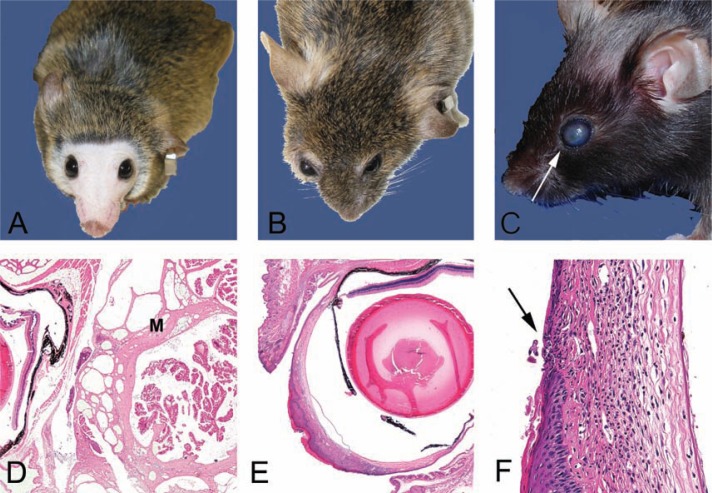
Fig. 3.
Clinical and histological presentations of common eye lesions. A. Normal periocular shape, eye size, and color in a 24-month-old CB6F1 mouse included here for contrast to the mouse in 3B. Note the lack of pelage and vibrissae due to extensive barbering by cage mates. Barbering is another relatively common skin presentation. It may lead to dermatitis in the victim and impaction of hair fragments into gingival sulcus of the barber. B. A 24-month-old CB6F1 mouse has periocular and retrobulbar swelling (between arrows) with bulopthalmia. This presentation may be a result of periocular cellulitis, conjunctivitis, or retrobulbar mass such as an abscesses or neoplasia. In this mouse, the swelling was due to a large retrobulbar mass (4C), which was diagnosed histologically as a Harderian adenoma (3D) C. Corneal opacity in a 28–month-old B6 mouse. The small foci (arrow) at the rostal aspect of the cornea is an ulcer, which was confirmed clinically with fluorescein dye test clinically and histologically (3F) D. Hematoxylin and eosin-stained section of the Harderian gland adenoma from the CB6F1 mouse in panel 3B. The mutliobulated and expansible mass (M) is located in the retro-orbital space compresses the eye (E). E. Hematoxylin and eosin-stained section of the eye from the B6 mouse in 3C. The opacity noted clinically is due to marked proliferative and ulcerative keratitis (box). The normal corneal epithelium is non-keratinized and 4–7 cell layers thick. F. Higher magnification of boxed region of a punctate corneal ulcer in 3C and E. The defect in the overlying corneal epithelium (arrow) exposes the stroma. The hydrophilic stroma will uptake fluorescein dye when the hydrophobic epithelial layer is breeched. Note the dense inflammatory infiltrate and neovascularization in the stroma. These also contribute to the corneal opacity noted clinically (3C).