Abstract
Tourniquets are commonly used in limb surgeries, be it orthopedic or plastic surgeries. But the inflation pressures, the duration, and release guidelines are still not clear. According to a survey, majority of orthopedic surgeons inflate the tourniquet to fixed pressures for the upper and the lower limbs without considering the baseline blood pressure of the patient on whom the tourniquets are being applied. This review was designed to recall and review the safe use of tourniquets and the various techniques that can be employed to minimize the complications of tourniquet use. Google, science direct, and pubmed were searched for appropriate literature and relevant articles were identified.
Keywords: Tourniquet, orthopaedic surgery, tourniquet and complications
INTRODUCTION
The word tourniquet was derived from the French word tourner which means “to turn.” Earliest known usage of tourniquet dates back to 199 BCE–500 CE. It was used by the Romans to control bleeding, especially during amputation. These were narrow straps made of bronze, using only leather for comfort.1 Clinicians previously used Esmarch tourniquet which was a type of rubber band that was wrapped around the extremity to exsanguinate the blood and tied it at the proximal end so as to facilitate relatively bloodless surgery in the distal extremity. But it was capable of generating very high pressures and shearing forces during application, leading to skin trauma, underlying nerve trauma, and even fatal complications like pulmonary embolism.2 All these complications led to the abandoning of its use.
To overcome these shortcomings, the pneumatic tourniquets were introduced in 1904 by Harvey Cushing.3 The problems with such tourniquets are less frequent if applied under direct supervision of experienced personnel and if proper inflation pressures and tourniquet times are observed. Tourniquet inflation leads to local effects due to compression and effects on all the organ systems. Tourniquet pain is one of the most intriguing pains for the anesthesiologist and also a cause of concern for the orthopedic surgeons.
This review article was aimed to discuss (1) physiological changes of tourniquet application, (2) complications of tourniquet use, (3) pre-application precautions, (4) proper application of tourniquet, (5) the safe duration and pressure for tourniquet use, (6) recommendations for the safe use of tourniquet, (7) tourniquet pain: its cause and management, (8) timing of tourniquet release, (9) the effects of deflation of tourniquet.
SEARCH STRATEGY
A search of literature was done using pubmed, EMBASE, google, Cochrane databases, and science direct for the last ten years (2000–2010). Key words such as tourniquet orthopaedic surgery, physiological changes, tourniquet pain, intravenous regional anaesthesia and tourniquet pain, additives to relieve tourniquet pain, duration of inflation, local anaesthetics and tourniquet pain, tourniquet and complications, safe use of tourniquet, and deflation of tourniquet were used. Forty six randomized controlled trials were retrieved, out of which four were excluded from the review as they were conducted on patients undergoing plastic surgeries and three were excluded as they were conducted on animals. Out of the remaining 39, 25 were full text articles and the rest were abstracts. Three review articles on the subject were also included, along with case reports of complications of tourniquet use. Recommendations from the Association of perioperative Registered Nurses (AORN) practice committee and the AORN board of directors were also included in the review process as these are updated from time to time according to the evidence collected over the last few years. Studies on antibiotic levels and prophylaxis were not included in the review process.
Physiological changes of tourniquet application
The limb should be exsanguinated by elevating and using an Esmarch bandage or tourniquet exsanguinators (S-MART)4 for emptying the blood vessels from the distal end to the proximal end prior to tourniquet inflation. There are numerous advantages of this, including establishing a clear operating field, reducing overall blood loss, and reducing the risk of microemboli at the time of release.4 This exsanguination results in autotransfusion of blood from the peripheral circulation into the central circulation.5 The optimal timing and angle of elevation for maximal exsanguinations of arm6 has been shown to be 5 min at 90° and the same for leg7 is 5 min at 45°. There is progressive cellular hypoxia, acidosis, and cooling in the occluded limb. Muscle is more susceptible to ischemic damage than nerve. Histological evidence of muscle damage is evident 30–60 min after tourniquet inflation. Decreased pH (<6.5),8 decreased pO2,9 increased pCO2, increased K+, increased lactate,5 occur progressively. These changes are generally mild and well tolerated. Tourniquet pain develops in up to 66% of patients, 30–60 min after cuff inflation.10 Tourniquet-induced hypertension occurs in 11–66% of cases. The onset is analogous to the onset of tourniquet pain.10 Tissue edema develops if the tourniquet time exceeds 60 min.11 After deflation, the return of circulation leads to the development of the reperfusion injury.12
Complications of tourniquet
Nerve injury is the most common complication.13 Although the pathophysiology of nerve injury associated with tourniquet use remains unclear, it is likely that both mechanical compression and neural ischemia play an important role.14 It can range from mild transient loss of function to irreversible damage and paralysis.
Intraoperative bleeding may occur due to an under-pressurized cuff, insufficient exsanguination, improper cuff selection, loosely applied cuff, calcified vessels or too slow inflation or deflation.13 Compartment syndrome, pressure sores, chemical burns, digital necrosis,15 deep venous thrombosis leading to pulmonary or venous embolization,5 tourniquet pain, thermal damage to tissues, and rhabdomyolysis16 are the other potential complications. High pressures and forgotten digital tourniquets can lead to severe ischemic injuries of the digits.15,17
Massive pulmonary embolism has also been reported during inflation and patients with deep vein thrombosis (DVT) must be closely monitored during limb exsanguination.18
“Post-tourniquet syndrome” may occur in patients who have had tourniquets applied for prolonged times.13 The presenting features of the syndrome are swollen, stiff, pale limb with weakness but no paralysis usually after 1–6 weeks of tourniquet application.5 Postoperative edema is the main etiology.5
Pre-application precautions
The pressure source, cuff, regulator, tubing, and connectors need to be checked before use and as wide a cuff as possible should be used. Wider cuffs provide better transmission of tissue compression and lower cuff pressures are required to compress the artery and hence minimize potential pressure-related complications.19 In a cross-over volunteer study of 20 patients, all the patients were subjected to wide as well as narrow cuffs and it was found that wider cuffs (14 cm) were less painful than narrow cuffs (7 cm) if inflated at lower pressures and they were still effective at occluding blood flow.20 The cuff should not directly overlie bony prominences like the head of fibula or malleoli as there is risk of direct nerve compression.21 Hence, it is recommended that the edge of the tourniquet should be at least 2 cm distal to the head of fibula and 2 cm proximal to the malleoli in case of calf cuffs.21 It is recommended that tourniquets be avoided in fixation of simple isolated fractures of fibula as it may increase the time of recovery and postoperative complications.22 The length of the cuff should be individualized, according to the size and circumference of the patient's limb. It is recommended that the shape should allow a snug fit at both proximal and distal edges. The width should be the widest possible but it should not encroach upon the surgical site. The length should be the minimum that assures overlap around the limb sufficient to fully engage the fasteners.23,24 The cuff should overlap at least 3 inches, but not more than 6 inches as it may cause generation of high pressures.25
Limbs with severe infection, patients with poor cardiac reserve, and traumatized limbs are relative contraindications to tourniquet use.5 Peripheral neuropathy, DVT in the limb, Reynaud's disease, and peripheral vascular disease should be ruled out before considering tourniquet application.5 Tourniquets have been used in patients with sickle cell disease and trait, and a complication rate of 12.5% was observed in four studies included in a review article, which included 96 patients.26 Uneventful use of the tourniquet in such cases has been reported by other investigators.27–29 Extra caution in the perioperative period should be practiced in such patients.
Proper application of tourniquet
The tourniquet should be applied very carefully to the proximal part of the limb at the greatest circumference because the muscle bulk at that site is the greatest, and hence it affords a greater protection against nerve injury. The tourniquet should be first deflated and smoothened out. Adequate padding should be done at that site. Various types of skin protection padding are available such as the Soffban skin protection (BSN Medical, Melbourne, Australia), Atlantech skin protection drape (Atlantech Medical Devices, Harrogate, UK), Velbands, etc. Velbands were found to be safe and cost-effective skin protection beneath the tourniquet.30 Soffban and Atlantech skin protection drapes have been found to decrease the rate of skin complications as compared to direct application of tourniquet on the skin.31 Stretched sleeves made of two-layer tubular elastic material and matched to the specific tourniquet cuffs produced significantly lesser and less severe pinches and wrinkling of the skin as compared to other limb protection devices studied in 55 different trials using five types of limb protection devices.19 Any solution applied to the skin must not be allowed to run underneath the tourniquet as it may lead to skin burns. A circumferential adhesive backed plastic drape applied just distal to the tourniquet can help in preventing this. The tourniquet should be inflated after the limb has been exsanguinated and prepared for surgery.32
The safe duration and pressure for tourniquet
Safe duration and pressure for tourniquet use remains a controversy. No strict guidelines have been laid down. A safe time limit of 1–3 h has been described.33 Horlocker et al. (2006) have found a strong correlation of nerve injury with prolonged total tourniquet time with an approximate threefold increase in risk of neurological complications for each 30 min increase in tourniquet inflation. The duration of uninterrupted tourniquet inflation also increased the likelihood of neural dysfunction.14 Use of tourniquet for >2 h and pressures of >350 mm Hg in lower extremity and >250 mm Hg in upper extremity increases the risk of compression neurapraxia. If >2 h is required, the tourniquet should be deflated for 5 min for every 30 min of inflation time.34
Orthopedic surgeons generally practice fixed inflation pressures (typically 250 mm Hg for upper arm and 300 mm Hg for thigh) or fixed amount of pressure above systolic arterial pressure (typically +100 mm Hg for upper arm and 100–150 mm Hg for thigh).35 These practices should not be followed as these do not take into account the age in both and the blood pressure (BP) of the patient in the former technique. As it has been hypothesized by Horlocker et al. (2006), younger patients have lower systolic blood pressures (SBP), and hence inflating the tourniquets to fixed pressures leads to a larger difference between tourniquet inflation pressure and arterial pressure, leading to excessive compression.13 Use of lowest effective inflation pressure has been advocated to minimize tourniquet-related nerve injury.36
Limb occlusion pressure (LOP) has been utilized to calculate the tourniquet inflation pressure by the AORN. It is the pressure in the tourniquet at which the distal arterial blood flow, as assessed by a Doppler probe held over a distal artery, is occluded. This value is generally higher than the SBP. The AORN guidelines recommend that the tourniquet be inflated intraoperatively to a pressure higher than the LOP. A safety margin is added to cover intraoperative fluctuations in arterial pressure. If LOP is <130 mm Hg, the safety margin is 40 mm Hg; for LOP 131–190 mm Hg, the margin is 60 mm Hg; and if LOP is >190 mm Hg, the margin is 80 mm Hg.37 For pediatric patients, adding 50 mm Hg has been recommended.38 Studies have shown that cuff pressure based on LOP measured immediately prior to surgery is generally lower than the commonly used cuff pressures and is sufficient to maintain a satisfactory surgical field.39 Shaw et al. (1982) recommend that lowest tourniquet pressure that maintains a bloodless field should be used.40 Levy et al. (1993) found that the mean calculated tourniquet pressure was 202.3 ± 34.2 mm Hg for adequate hemostasis in the upper limb, which was well below the 250–300 mm Hg previously recommended and frequently employed.41 Clonidine has been found to exacerbate the reduction in mean arterial BP and delayed BP recovery following tourniquet deflation probably associated with clonidine-induced inhibition of noradrenaline release.42 Tourniquet release allowing a reperfusion interval of 10–30 min, followed by re-inflation is recommended to extend the duration of total tourniquet time.43 Since the deflation for 5 minutes after every 30 min seems impractical from the surgical point of view, so for all practical purposes it should be deflated for at least 10 minutes if the surgical time is more than 2 hr. This is also supported by a survey by Odinnson et al. wherein it has been shown thatmost of the orthopedic surgeons felt that a 15-min deflation time after 2 h tourniquet time was safe. The incidence of reported complications in this survey was 26 in 63,484 cases. Fifteen out of these were neurological in nature, out of which two were permanent.44 Longer duration of deflation has been associated with a modest decrease in frequency of neurological complications.14 It is concluded that the tourniquet should be inflated according to the LOP and should be deflated after 2 h for the lower limb and after 1½ h for the upper limb for at least 10 minutes.
Recommendations for the safe use of tourniquet
The AORN board of directors has approved the following practices for the safe use of tourniquets.24 These are effective from January 1, 2007.
Patient safety should be the primary consideration in evaluation, selection, purchase and use of the pneumatic tourniquet and accessories. The tourniquet and its accessories should be inspected, tested and maintained according to manufacturers’ written instructions. The perioperative nurse should assess the patient preoperatively for risks and report potential contraindications to the surgeon. The pneumatic tourniquet should be connected to the appropriate power/gas source, the components should be handled and the cuff applied in a manner to minimize the risk of patient injury. The extremity should be exsanguinated before inflation of the tourniquet. Tourniquet inflation pressure should be kept to the minimum effective pressure. Inflation time should be kept to a minimum and deflation managed to minimize risks to the patient. The patient should be monitored continuously with special consideration to parameters like hypertension and tachycardia as a surrogate of tourniquet pain and temperature of the limb while the tourniquet cuff is inflated. The perioperative registered nurse should evaluate the outcome of the patient care at the end of the procedure. Additional care should be taken in procedures involving tourniquet control on two extremities because the risk of complications and the systemic effects of tourniquet use may be increased. Potential patient injuries and complications associated with intravenous regional anesthesia (IVRA, Bier's block) should be identified and safe practices established. The tourniquet user should have a very clear understanding as to the sequence of inflation and deflation when using a dual bladder cuff or two single bladder cuffs. Allergies to local anesthetic solutions should be ruled out before hand. Severe injuries and even deaths have been reported when the wrong cuff was deflated.45 The tourniquet and accessories should be cleaned after each use. Patient assessments, plan of care, interventions implemented, and evaluation of care related to use of a pneumatic tourniquet should be documented. Education, competency assessment, and validation should be conducted before the perioperative registered nurse manages the care of a patient using a pneumatic tourniquet. Policies and procedures for pneumatic tourniquets should be developed, reviewed periodically, revised and updated as necessary and should be available for ready reference in the practice setting. The health care organization's quality management program should include investigation of adverse events and near misses associated with the use of a pneumatic tourniquet.
The Association of Surgical Technologists (AST) has also recommended that the surgical team members should complete training to demonstrate the knowledge and competency in proper use of the pneumatic tourniquet. Documentation of the use of tourniquet should be included in the patient's operation theater records.23
Thigh tourniquet should not be inflated with the knee in the flexed position followed by leg straightening as this fixates the sciatic nerve to the femur and causes extreme traction on the nerve.46
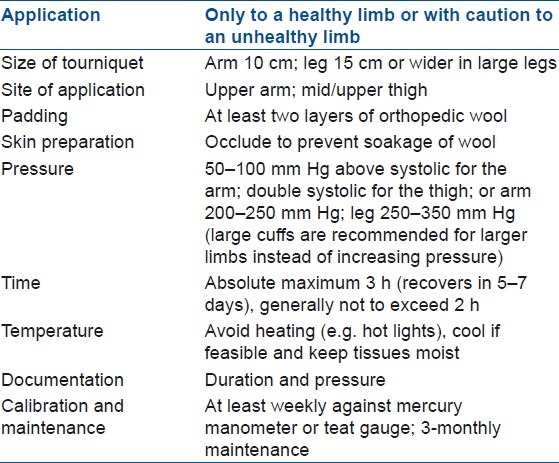
Bruner had laid down 10 rules for the safe use of tourniquet, which have been modified by Braithwaite and Klenerman and are given in Table 1.47
Table 1.
Bruner's ten rules for the safe use of tourniquet (Modified by Barithwaite and Klenerman)47
Digital tourniquets in the form of rolled glove, Penrose drain, or catheters have been shown to generate wide ranges of pressures.48 Hence, safe use guidelines were laid down by Shaw et al. by measuring physiological pressures.48 Tourniquets have also been used in fixation of closed fractures and intramedullary nailing,49 diabetic foot amputations50 and trauma and war situations in the absence of shock,51 reimplantation, and microvascular procedures.52
Tourniquet pain: Its cause and management
The clinical syndrome of tourniquet pain consists of several components and is not just due to the pain and pressure under the tourniquet.53 The smaller unmyelinated C-fibers are more resistant to local anesthetic (LA) induced conduction block as compared to the larger myelinated A-fibers.54 After intrathecal administration of an adequate dose of LA, conduction in both A- and C-fibers is blocked. But as the concentration of LA in the cerebrospinal fluid (CSF) decreases, the C-fibers start conducting impulses before the A-fibers, resulting in a dull tourniquet pain in the presence of an anesthetic, which when assessed by pin prick appears adequate.35
Eutectic mixture of local anesthetic (EMLA) cream application,55,56 LAs given via the neuraxial route with or without opioids,57–62 or IVRA63,64 have been used to attenuate tourniquet-induced pain. Magnesium sulfate,65,66 ketamine, and ketorolac66 have also been used as adjuvants in IVRA, with variable results.66,67 Clonidine has also been successfully used.68–70 Various agents including dexmedetomidine and ketamine67–68 have also been used intravenously to attenuate this pain.
Alternative techniques like electropuncture71,72 and meditation72 have also been used for tourniquet pain.
Timing of tourniquet release
There are different schools of thought regarding the timing of release of tourniquet. Three studies on timing of tourniquet release were found including 120 knees (80 patients with unilateral procedures and 20 patients with bilateral total knee arthroplasty) and 18 patients for bilateral carpel tunnel release. The study group was divided into two equal groups (40 patients in each group in one study and 20 patients in the second study with 20 knees where tourniquet was released before and 20 knees where tourniquet was released after the closure). In one group, the tourniquet was deflated before wound closure, and in the other, after wound closure. There are no significant differences in complications like pain or ecchymosis in patients in whom the tourniquet was released prior to or after skin closure. Hemostasis control was better if it was released after wound closure and it also helped decrease the operative time by reducing the time lost in achieving hemostasis if the tourniquet was released prior to skin closure.73–75
The effects of deflation of tourniquet
Deflation leads to a decrease in mean arterial BP significantly, partly owing to the release of metabolites from the ischemic limb into the circulation and the decrease in peripheral vascular resistance. A transient increase in EtCO2, decrease in temperature, and central venous oxygen tension are seen.
The re-establishment of blood flow following deflation of tourniquet can induce a paradoxical extension of ischemic damage12 mediated by oxygen free radicals and is known as the “reperfusion syndrome.” There is interaction between the activated neutrophils and the surface adhesion molecules on the vascular endothelium.76–78 Leukocyte infiltration begins,79 and the expression of isolated neutrophils CD11b, CD18, endothelial cell adhesion molecule-1 (CAM-1) occurs.80 This has local and widespread systemic effects.81 Acute Respiratory Distress Syndrome (ARDS), renal and cardiac injuries may occur and may lead to other severe and often fatal complications.81,82 Reperfusion injury also occurs during organ transplantation, aortic cross clamping, cardiac bypass, tissue grafting, and intestinal resections. Treatment with hydrogen sulfide83 and l-arginine,84 and pre-treatment with individual monoclonal antibodies85 has been shown to limit the ischemia reperfusion injury.
Venous embolization is another complication reported after deflation of tourniquet, especially of the lower limbs.86
CONCLUSION
Tourniquets are useful aids for limb procedures as they decrease the blood loss during surgery and provide a relatively bloodless field for the surgeon if used properly. Safe use of tourniquets by implementation of proper padding underneath the tourniquet, not exceeding the safe limit of tourniquet pressure and duration, deflating the tourniquet for short intervals of 10–15 min if the safe tourniquet time has elapsed, and providing adequate analgesia by blocks, regional techniques, or LA drugs or creams, IV opioids, or analgesics can go a long way in reducing the complications associated with tourniquet use. Pre-determination of LOP and inflating tourniquets accordingly can help reduce the complications associated with the use. It should be avoided in patients with DVT, peripheral neuropathies, peripheral vascular disease, sickle cell disease, and Reynaud's disease, or in small surgeries of fibula. Proper patient monitoring and care after deflation and careful search for neurological deficit postoperatively, if any, can definitely minimize the complications associated with tourniquet usage. All these measures to reduce the complications of tourniquet need to be proved by conducting large-scale randomized controlled clinical trials. More number of randomized controlled trials and prospective studies need to be done to evaluate the differential nerve injuries after tourniquet use. The newer tourniquet deflation devices like S-MART have recently come in the market and larger trials and studies need to be done to prove their efficacy.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Noordin S, McEwen JA, Kragh JF, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91:2958–67. doi: 10.2106/JBJS.I.00634. [DOI] [PubMed] [Google Scholar]
- 2.Lu CW, Chen YS, Wang MJ. Massive pulmonary embolism after application of an Esmarch bandage. Anesth Analg. 2004;98:1187–9. doi: 10.1213/01.ANE.0000104583.77388.02. [DOI] [PubMed] [Google Scholar]
- 3.Murphy CG, Winter DC, Bouchier-Hayes DJ. Tourniquet injuries: pathogenesis and modalities for attenuation. Acta Orthop Belg. 2005;71:635–45. [PubMed] [Google Scholar]
- 4.Tourniquet – A S-MART concept. Simon Axon. From: http://usmorthopaedic.blogspot.in/2009/06/tourniquet-s-martconcept.html .
- 5.Duffy PJ. The arterial tourniquet. Department of Anaesthesia, Ottawa General Hospital. Accessed from: http://www.uam.es/departamentos/medicina/anesnet/gtoa/hm1.html .
- 6.Warren PJ, Hardiman PJJ-P, Woolf VJ. Limb exsanguination. I. The arm: effect of angle of elevation and arterial compression. Ann R Coll Surg Engl. 1992;74:320–2. [PMC free article] [PubMed] [Google Scholar]
- 7.Warren PJ, Hardiman PJJ-P, Woolf VJ. Limb exsanguination. II. The leg: Effect of angle of elevation. Ann R Coll Surg Engi. 1992;74:323–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Hampson NB, Piantadosi CA. Near infrared monitoring of human skeletal muscle oxygenation during forearm ischemia. J Appl Physiol. 1988;64:2449–57. doi: 10.1152/jappl.1988.64.6.2449. [DOI] [PubMed] [Google Scholar]
- 9.Ikemoto Y, Kobayashi H, Usui M, Ishii S. Changes in serum myoglobin levels caused by tourniquet ischemia under normothermic and hypothermic conditions. Clin Orthop Relat Res. 1988;234:296–302. [PubMed] [Google Scholar]
- 10.Micheal K. Urban. Anaesthesia for orthopaedic surgery. In: Miller RD, editor. Miller's Anesthesia. 7th ed. Philadelphia: Churcill Livingstone Publishers; 2010. p. 2252. [Google Scholar]
- 11.Wilgis EF. Observations on the effects of tourniquet ischemia. J Bone Joint Surg Am. 1971;53:1343–6. [PubMed] [Google Scholar]
- 12.Hearse DJ. Reperfusion of the ischemic myocardium. J Mol CellCardiol. 1977;9:605–16. doi: 10.1016/s0022-2828(77)80357-x. [DOI] [PubMed] [Google Scholar]
- 13.Estebe JW. Complications of tourniquet use. [Accessed on 09/06/2011]. From: http://www.tourniquets.org/complications_preventive.php .
- 14.Horlocker TT, Hebl JR, Gali B, Jankowski CJ, Burkle CM, Berry DJ, et al. Anesthetic, patient and surgical risk factors for neurologic complications after prolonged total knee arthroplasty. Anesth Analg. 2006;102:950–5. doi: 10.1213/01.ane.0000194875.05587.7e. [DOI] [PubMed] [Google Scholar]
- 15.Avci G, Akan M, Yildirim S, Aköz T. Digital neurovascular compression due to a forgotten tourniquet. Hand Surg. 2003;8:133–6. doi: 10.1142/s0218810403001595. [DOI] [PubMed] [Google Scholar]
- 16.Palmer SH, Graham G. Tourniquet-induced rhabdomyolysis after total knee replacement. Ann R Coll Surg Engl. 1199;76:416–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Durrant C, Townley WA, Ramkumar S, Khoo CT. Forgotten digital tourniquet: Salvage of an ischemic finger by application of medicinal leeches. Ann R Coll Surg Engl. 2006;88:462–4. doi: 10.1308/003588406X117052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Song JE, Chun DH, Shin JH, Park C, Lee JY. Pulmonary thromboembolism after tourniquet inflation under spinal anesthesia -A case report. Korean J Anesthesiol. 2010;59(Suppl):S82–5. doi: 10.4097/kjae.2010.59.S.S82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McEwen JA, Inkpen K. Tourniquet safety preventing skin injuries. Surgical Technol. 2002;34:6–15. [Google Scholar]
- 20.Estebe JP, Le Naoures A, Chemaly L, Ecoffey C. Tourniquet pain in a volunteer study: Effect of changes in cuff width and pressure. Anaesthesia. 2000;55:21–6. doi: 10.1046/j.1365-2044.2000.01128.x. [DOI] [PubMed] [Google Scholar]
- 21.Groah . Perioperative nursing. 3rd ed. Stamford, Conn: Appleton & Lange; 1996. 304. [Google Scholar]
- 22.Maffulli N, Testa V, Capasso G. Use of a tourniquet in the internal fixation of fractures of the distal part of the fibula. A prospective, randomized trial. J Bone Joint Surg Am. 1993;75:700–3. doi: 10.2106/00004623-199305000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Recommended Standards of Practice for safe use of Pneumatic Tourniquets. [Last accessed on 2012 May 29]. Available From: http://www.ast.org .
- 24.Recommended Practices for use of the pneumatic tourniquet in the perioperative practice setting. Equipment and product safety. 2009. [Last accessed on 2010 Aug 07]. Available From: http://www.Gnmhealthcare.com .
- 25.Kam PC, Kavanagh R, Yoong FF. The arterial tourniquet: pathophysiological consequences and anaesthetic implications. Anaesthesia. 2001;56:534–45. doi: 10.1046/j.1365-2044.2001.01982.x. [DOI] [PubMed] [Google Scholar]
- 26.Fisher B, Roberts CS. Tourniquet use and sickle cell hemoglobinopathy: How should we proceed? South Med J. 2010;103:1156–60. doi: 10.1097/SMJ.0b013e3181efaf3b. [DOI] [PubMed] [Google Scholar]
- 27.Al-Ghamdi AA. Bilateral total knee replacement under tourniquet in a homozygous sickle cell patient. Anesth Analg. 2003;98:543–4. doi: 10.1213/01.ANE.0000099363.42829.0A. [DOI] [PubMed] [Google Scholar]
- 28.Adu-Gyamfi Y, Sankarankutty M, Marwa S. Use of a tourniquet in patients with sickle-cell disease. Can J Anaesth. 1993;40:24–7. doi: 10.1007/BF03009313. [DOI] [PubMed] [Google Scholar]
- 29.Stein RE, Urbaniak J. Use of the tourniquet during surgery in patients with sickle cell hemoglobinopathies. Clin Orthop. 1980;151:231–3. [PubMed] [Google Scholar]
- 30.Guo S. Is Velband still a safe and cost effective skin protection beneath the tourniquet in hand surgery? Hand Surg. 2011;16:5–8. doi: 10.1142/S0218810411004996. [DOI] [PubMed] [Google Scholar]
- 31.Din R, Geddes T. Skin protection beneath the tourniquet. Aprospective randomized trial. ANZ J Surg. 2004;74:721–2. doi: 10.1111/j.1445-1433.2004.03143.x. [DOI] [PubMed] [Google Scholar]
- 32.Crenshaw AH. Surgical Technique and approaches. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopaedics. 11th edition. Philadelphia USA: Mosby Elsevier; 2010. pp. 4–6. [Google Scholar]
- 33.Pedowitz RA. Tourniquet-induced neuro-muscular injury.Arecent review of rabbit and clinical experiments. Acta Orthop Scand Suppl. 1991;245:1–33. [PubMed] [Google Scholar]
- 34.Wheeless CR., 3rd In Wheeless Textbook of Orthopedics. Extremity Tourniquets. Available on internet http://www.wheelessonline.com/ortho/extremity_tourniquets .
- 35.Deloughry JL, Griffiths R. Arterial tourniquets. Continuing Education in Anaesthesia. Crit Care Pain (Indian Edition) 2009;2:64–8. [Google Scholar]
- 36.Mohler LR, Pedowitz RA, Myers RR, Ohara WM, Lopez MA, Gershunni DH. Intermittent reperfusion fails to prevent post tourniquet neurapraxia. J Hand Surg Am. 1999;24:687–93. doi: 10.1053/jhsu.1999.0687. [DOI] [PubMed] [Google Scholar]
- 37.AORN Recommended Practices Committee. Recommended practices for the use of the pneumatic tourniquet in the perioperative practice settings. AORN J. 2007;86:640–55. doi: 10.1016/j.aorn.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Tredwell SJ, Wilmink M, Inkpen K, McEwen JA. Pediatric tourniquets: Analysis of cuff and limb interface, current practice, and guidelines for use. J Pediatr Orthop. 2001;21:671–6. [PubMed] [Google Scholar]
- 39.McEwen JA, Inkpen KB, Younger A. Thigh tourniquet safety: LOP measurement and a wide contoured cuff allows lower cuff pressure. Surg Tech. 2002;34:8–18. [Google Scholar]
- 40.Shaw JA, Murray DG. The relationship between tourniquet pressure and underlying soft-tissue pressure in the thigh. JBone Joint Surg. 1982;64:1148–52. [PubMed] [Google Scholar]
- 41.Levy O, David Y, Heim M, Eldar I, Chetrit A, Engel J. Minimal tourniquet pressure to maintain arterial closure in upper limb surgery. J Hand Surg Br. 1993;18:204–6. doi: 10.1016/0266-7681(93)90111-r. [DOI] [PubMed] [Google Scholar]
- 42.Sarkar S, Acharya A, Pahari S. Effect of oral clonidine pre-medication on hemodynamic response to tourniquet deflation following epidural anesthesia for lower extremity surgeries. Indian J Anaesth. 2006;50:266–70. [Google Scholar]
- 43.Sapega AA, Heppenstall B, Chance B. Optimising tourniquet application and release times in extremity surgery. J Bone Joint Surg Am. 1985;67:303–14. [PubMed] [Google Scholar]
- 44.Odinnson A, Finsen V. Tourniquet use and its complications in Norway. J Bone Joint Surg Br. 2006;88:1090–2. doi: 10.1302/0301-620X.88B8.17668. [DOI] [PubMed] [Google Scholar]
- 45.Pneumatic tourniquets used for regional anesthesia. Health Devices. 1982;12:48–9. [Google Scholar]
- 46.Hamid B, Zuccherelli L. Nerve injuries. In: Boezaert AP, editor. Anaesthesia and Orthopaedic surgery. New York: McGraw Hill publishers; 2006. p. 409. [Google Scholar]
- 47.Kutty S, McElwain JP. Padding under tourniquets in tourniquet controlled surgery: Bruner's ten rules revisited. Injury. 2002;33:75. doi: 10.1016/s0020-1383(01)00072-9. [DOI] [PubMed] [Google Scholar]
- 48.Shaw JA, DeMuth WW, Gillespy AW. Guidelines for the use of digital tourniquet based on physiological pressure measurements. J Bone Joint Surg Am. 1985;67:1086–90. [PubMed] [Google Scholar]
- 49.Ryf C, Melcher GA, Rüedi T. Pneumatic tourniquet as a repositioning aid in closed intramedullary nailing. Unfallchirurg. 1995;98:617–9. [PubMed] [Google Scholar]
- 50.Zgonis T, Stapleton JJ, Girard-Powell VA, Hagino RT. Surgical management of diabetic foot infections and amputations. AORN J. 2008;87:935–46. doi: 10.1016/j.aorn.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 51.Kragh JF, Jr, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249:1–7. doi: 10.1097/SLA.0b013e31818842ba. [DOI] [PubMed] [Google Scholar]
- 52.Dumanian GA, Chen A. Microvascular surgery in a bloodless field. Microsurgery. 2000;20:221–4. doi: 10.1002/1098-2752(2000)20:5<221::aid-micr2>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 53.Hagenouw RR, Bridenbaugh PO, Egmond J, Stuebing R. Tourniquet pain: A volunteer study. Anesth Analg. 1986;65:1175–80. [PubMed] [Google Scholar]
- 54.Gissen AJ, Covino BG, Gregus J. Differential sensitivities of mammalian nerve fibres to local anesthetic agents. Anesthesiology. 1980;53:467–74. doi: 10.1097/00000542-198012000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Lowrie A, Jones MJ, Eastley RJ. Effect of eutectic mixture of local anaesthetic agents (EMLA) on tourniquet pain in volunteers. Br J Anaesth. 1989;63:751–3. doi: 10.1093/bja/63.6.751. [DOI] [PubMed] [Google Scholar]
- 56.Ogufere WE, Giddins GE, Thom JS. Upper arm tourniquet pain in local anesthesia surgery. J Hand Surg (European Volume) 1995;20:413–4. doi: 10.1016/s0266-7681(05)80106-8. [DOI] [PubMed] [Google Scholar]
- 57.Choi IH, Koh H, Kwak IY. A comparison of tourniquet pain in spinal anaesthesia. Korean J Anaesthesiol. 1996;31:371–5. [Google Scholar]
- 58.Concepcion MA, Lambert DH, Welch KA, Covino BG. Tourniquet pain during spinal anesthesia: A comparison of plain solution of tetracaine and bupivacaine. Anesth Analg. 1988;67:828–32. [PubMed] [Google Scholar]
- 59.Lee Y, Tung MC, Who LH, Lai KB, Wong KL, Wu KH, et al. The effect of epidural anesthesia on tourniquet pain: A comparison of 2% lidocaine and 0.5% bupivacaine. [Article in Chinese] Ma Zui Xue Za Zhi. 1990;28:459–64. [PubMed] [Google Scholar]
- 60.Bonnet F, Diallo A, Saada M, Belon M, Gilbaud M, Baico O. Prevention of tourniquet pain by spinal isobaric bupivacaine with clonidine. Br J Anaesth. 1989;63:93–6. doi: 10.1093/bja/63.1.93. [DOI] [PubMed] [Google Scholar]
- 61.Cherng CH, Wong CS, Chang FL, Ho SJ, Lee CH. Epidural morphine delays the onset of tourniquet pain during epidural lidocaine anesthesia. Anesth Analg. 2002;94:1614–6. doi: 10.1097/00000539-200206000-00046. [DOI] [PubMed] [Google Scholar]
- 62.Okamoto T, Mitsuse T, Kashiwagi T, Iwaane E, Sakata Y, Masuda K, et al. Prophylactic epidural administration of fentanyl for the suppression of tourniquet pain. J Anaesthesia. 1996;10:5–9. doi: 10.1007/BF02482060. [DOI] [PubMed] [Google Scholar]
- 63.James NK, Khoo CT, Fell RH. The “mini-Bier's block”: a new technique for prevention of tourniquet pain during axillary brachial plexus anaesthesia. J Hand Surg Br. 1994;19:347–9. doi: 10.1016/0266-7681(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 64.Estèbe JP, Gentili ME, Langlois G, Mouilleron P, Bernard F, Ecoffey C. Lidocaine priming reduces tourniquet pain during intravenous regional anaesthesia: A preliminary study. RegAnaesth Pain Med. 2003;28:120–3. doi: 10.1053/rapm.2003.50123. [DOI] [PubMed] [Google Scholar]
- 65.Narang S, Dali JS, Agarwal M, Garg R. Evaluation of the efficacy of magnesium sulfate as an adjuvant to lignocaine for upper limb surgery. Anaesth Intensive Care. 2008;36:840–4. doi: 10.1177/0310057X0803600614. [DOI] [PubMed] [Google Scholar]
- 66.Bose S, Sunder RA, Rewari V, Saksena R. Study of magnesium, ketamine, ketorolac as adjuvants to lidocaine in intravenous regional anaesthesia. Annual Meeting Abstracts American Society of Anaesthesiologists. 2008 Oct 19; [Google Scholar]
- 67.Viscomi CM, Friend A, Parker C, Murphy T, Yarnell M. Ketamine as an adjuvant in lidocaine intravenous regional anesthesia: a randomised, double-blind, systemic control trial. Reg Anaesth Pain Med. 2009;34:30–3. doi: 10.1097/AAP.0b013e31819bb006. [DOI] [PubMed] [Google Scholar]
- 68.Lurie SD, Reuben SS, Gibson CS, DeLuca PA, Maciolek HA. Effect of clonidine on upper extremity tourniquet pain in healthy volunteers. Reg Anaesth Pain Med. 2000;25:502–5. doi: 10.1053/rapm.2000.8460. [DOI] [PubMed] [Google Scholar]
- 69.Gentili M, Bernard JM, Bonnet F. Adding clonidine to lidocaine for intravenous regional anesthesia prevents tourniquet pain. Anesth Analg. 1999;88:1327–30. doi: 10.1097/00000539-199906000-00024. [DOI] [PubMed] [Google Scholar]
- 70.Gorgias NK, Maidatsi PG, Kyriakidis AM, Karakoulas KA, Alvanos DN, Giala MM. Clonidine versus ketamine to prevent tourniquet pain during intravenous regional anaesthesia with lidocaine. Reg Anaesth Pain Med. 2001;26:512–7. doi: 10.1053/rapm.2001.27857. [DOI] [PubMed] [Google Scholar]
- 71.Musial F, Gabriel T, Amthor N, Rampp T, Michalsen A, Dobos G. Is electro-puncture a placebo in experimental tourniquet pain? European Journal of Integrative medicine. 2008;1(Suppl 1):16–7. [Google Scholar]
- 72.Choi A, Musial F, Amthor N, Lauche R, Rampp T, Saha J, et al. The effect of electro acupuncture and meditation on experimental tourniquet pain. Eur J Integr Med. 2008;1(Suppl 1):15–6. [Google Scholar]
- 73.Christodoulou AG, Ploumis AL, Terzidis IP, Chantzidis P, Metsovitis SR, Nikiforos DG. The role of timing of tourniquet release and cementing on Perioperative blood loss in total knee replacement. Knee. 2004;11:313–7. doi: 10.1016/j.knee.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 74.Hutchinson DT, Wang AA. Releasing the tourniquet in carpel tunnel surgery. Hand. 2010;5:57–9. doi: 10.1007/s11552-009-9202-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thorey F, Stukenborg-Colsman C, Windhagen H, Wirth CJ. The effect of tourniquet release timing on Perioperative blood loss in bilateral cemented total knee arthroplasty: A prospective randomized study. Technol Health Care. 2008;16:85–92. [PubMed] [Google Scholar]
- 76.Granger DN, Benoit JN, Suzuki M, Grisham MB. Leukocyte adherence to venular endothelium during ischemia reperfusion. Am J Physiol. 1989;257:G683–8. doi: 10.1152/ajpgi.1989.257.5.G683. [DOI] [PubMed] [Google Scholar]
- 77.Hernandez LA, Grisham MB, Twohig B, Arfors KE, Harlan JM, Granger DN. Role of neutrophils in ischemia reperfusion-induced micro vascular injury. Am J Physiol. 1987;253:H699–703. doi: 10.1152/ajpheart.1987.253.3.H699. [DOI] [PubMed] [Google Scholar]
- 78.Stokes KY, Abdih HK, Kelly CJ, Redmond HP, Bouchier-Hayes DJ. Thermo tolerance attenuates ischemia reperfusion induced renal injury and increased expression of ICAM-1. Transplantation. 1996;62:1143–9. doi: 10.1097/00007890-199610270-00020. [DOI] [PubMed] [Google Scholar]
- 79.Wakai A, Wang JH, Winter DC, Street JT, O’Sullivan RG, Redmond HP. Tourniquet induced systemic inflammatory response in extremity surgery. J Trauma. 2001;51:922–6. doi: 10.1097/00005373-200111000-00016. [DOI] [PubMed] [Google Scholar]
- 80.Yamazaki T, Seko Y, Tamatani T, Miyasaka M, Yazaki Y. Expression of intracellular adhesion molecule-1 in rat with ischemia/reperfusion and limitation of infarct size by treatment with antibodies against cell adhesion molecules. Am J Pathol. 1993;143:410–8. [PMC free article] [PubMed] [Google Scholar]
- 81.Lan W, Harmon D, Wang JH, Ghori K, Shorten G, Redmond P. The effect of lidocaine on in vitro neutrophils and endothelial adhesion molecule expression induced by plasma obtained during tourniquet-induced ischemia and reperfusion. Eur J Anaesthesiol. 2004;21:892–7. doi: 10.1017/s0265021504000249. [DOI] [PubMed] [Google Scholar]
- 82.Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg. 2003;38:1170–7. doi: 10.1016/s0741-5214(03)00918-2. [DOI] [PubMed] [Google Scholar]
- 83.Fitzpatrick DB, Karmazyn M. Comparative effects of calcium channel blocking agents and varying extracellular calcium concentration on hypoxia/reoxygenation and ischemia/reperfusion-induced cardiac injury. J Pharmacol Exp Ther. 1984;228:761–8. [PubMed] [Google Scholar]
- 84.Elrod JW, Calvert JW, Duranski MR, Lefer DJ. Hydrogen sulphide donor protects against acute myocardial ischemia-reperfusion injury. Circulation. 2006;114:172. [Google Scholar]
- 85.Huk I, Nanobashvili J, Neumayer C, Punz A, Mueller M, Afkhampour K, et al. L-arginine treatment alters the kinetics of nitric oxide and superoxide release and reduces ischemia/reperfusion injury in skeletal muscle. Circulation. 1997;96:667–75. doi: 10.1161/01.cir.96.2.667. [DOI] [PubMed] [Google Scholar]
- 86.McGrath BJ, Hsia J, Boyd A, Shay P, Graeter J, Conry K, et al. Venous embolization after deflation of lower extremity tourniquets. Anesth Analg. 1994;78:349–53. doi: 10.1213/00000539-199402000-00025. [DOI] [PubMed] [Google Scholar]


