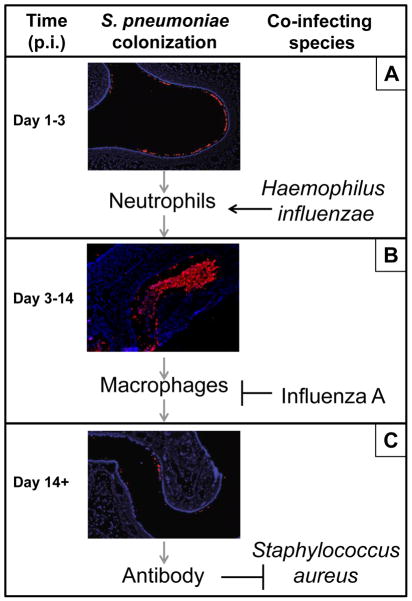
Figure 1. Co-infection alters immune responses to S. pneumoniae colonization in the upper respiratory tract.
(A) S. pneumoniae establishes colonization on the mucosal epithelium of the upper respiratory tract at day 1 post inoculation (p.i.) into the nares. Pneumococcal colonization elicits a neutrophil response that peaks around day 3 p.i. but is insufficient to clear the pneumococcus. However, co-colonization with H. influenzae results in a synergistic amplification of the neutrophil response that leads to elimination of pneumococci from the nasopharynx at this time-point. These enhanced host responses also drive the evolution of opsonophagocytosis-resistance determinants in the pneumococcus that contribute to this organism’s pathogenicity. (B) During mono-inoculation with S. pneumoniae, a gradual monocyte/macrophage influx peaks around day 7 p.i. and is responsible for pneumococcal clearance. However, co-infection with influenza A results in a synergistic induction of type I interferon expression which inhibits macrophage recruitment and results in an increase in pneumococcal colonization density. Influenza-induced increases in S. pneumoniae in the nasopharynx lead to an increased risk of invasive pneumococcal disease and pneumococcal transmission. (C). A robust antibody response to a diversity of antigens is mounted by two weeks following S. pneumoniae colonization. Cross-reactive antibody could explain why S. aureus carriage is negatively associated with S. pneumoniae colonization in immunocompetent, but not immunocompromised, hosts. Immunofluorescent microscopy images generated and kindly shared by Dr. Aoife Roche (Univ. of Pennsylvania) and adapted from Ref.#5. Host cells, blue (DAPI); S. pneumoniae cells, red.