Abstract
Context:
Caregivers play an important role in supporting people with illness either acute or chronic. It is important to explore caregiver's emotional turmoil as it helps in exploring their burden which can have impact on the patient's illness and functioning apart from their own.
Aims:
The current study aimed at assessing the predictors of anxiety and depression among caregivers of patients with stroke.
Settings and Design:
Seventy-five consecutive patient-caregiver dyads were recruited in the study.
Materials and Methods:
Patients and caregivers were assessed using a semi-structured proforma for the sociodemographic details. Subsequently these dyads were assessed for anxiety and depression levels using the Hospital Anxiety and Depression Scale.
Statistical Analysis Used:
Chi-square tests (for categorical variables) were used to find difference between the patients and the caregivers on different variables. Additionally Cramer's V-test and phi test were used for 2*4 contingency tables. Linear regression model was used.
Results:
Linear regression revealed that anxiety level in caregivers was predicted by the sex of care giver.
Conclusions:
Caring for the patients with stroke presents increased burden to the care givers which manifests as increased rate of anxiety and depression among them. It is important to assess the care givers along with the patients for emergence of these negative affective states. One needs to be extra cautious if the patient happens to be the primary earning member of the family.
Keywords: Anxiety, caregivers, depression, stroke
INTRODUCTION
Caregivers play an important role in supporting people with illness either acute or chronic. It is important to explore caregiver's emotional turmoil as it helps in exploring their burden which can have impact on the patient's illness and functioning apart from their own. The survivors of acute stroke experience long-term impairments in physical, psychosocial, and cognitive function.[1,2] Stroke is also associated with an increased prevalence of anxiety and depression. Survivors of stroke rely mainly on the caregivers for practical and emotional support concerning activities of daily living.[3,4] Thus the well being of caregivers is important because the patients depend on them to uphold in the community.
Additionally hospitalization puts burden on caregivers of patient as well. Caregivers of patients with neurological disorders have been found to be at higher risk of social isolation, emotional burden and a reduction in quality of life.[5–7] Burden of care of stroke patients impacts the physical as well as psychological well being of the caregivers adversely.[8] The caregivers have been found to have an increased rate of affective and anxiety disorders.[9–11]
Studies in stroke caregivers recognize the burden and impact on their physical and psychological well-being including high levels of psychological distress and depression; increased rates of physiological illness and personal, financial, family, and social problems.[8,12–14]
It is important to assess the mental health status and attend to the needs of caregivers. In spite of neurological conditions being one of the most common causes of disability very few studies have addressed the impact of these conditions on caregivers.[14] As earlier study by our group found a significant correlation between anxiety level of male caregivers and depression level of stroke patients. Also, anxiety level of female caregivers was related to anxiety level of stroke patients.[15]
The current study aimed at exploring the predictors of anxiety and depression among patients with stroke and their caregivers.
MATERIALS AND METHODS
The study was conducted at the in-patient setting of a tertiary care multispecialty hospital. Seventy five consecutive patient–caregiver dyads were recruited in the study. The patients selected for the study were diagnosed with stroke. Patient–caregiver dyads consenting for participation in the study were recruited. Patients or caregivers with any past history of psychiatric illness were excluded. Those having any language deficit or any cognitive deficit due to stroke, as assessed by Mini Mental Status Examination (MMSE), were also excluded from the study. This was done in order to ensure full participation of the subjects in the study. Additionally, subjects having history of prior stroke or any cardiovascular event were also excluded from the study.
Following inclusion in the study, patients and caregivers were assessed using a semi-structured proforma for the socio-demographic details. Subsequently these dyads were assessed for anxiety and depression levels using the Hospital Anxiety and Depression Scale (HADS). The assessments were carried out around one week after admission to the ward.
HADS is a self-report questionnaire commonly used to assess levels of anxiety and depression developed by Zigmond et al, in 1983.[16] The HADS comprises statements which the patient rates based on their experience over the past week. The 14 statements are relevant to generalized anxiety (7 statements) or ‘depression’ (7 statements), the latter being largely (but not entirely) composed of reflections of the state of anaerobia. Each question has 4 possible responses. Responses are scored on a scale from 3 to 0. The two subscales, anxiety (HADS-A) and depression (HADS-D), have been found to be independent measures. In its current form the HADS is now divided into four ranges: normal (0–7), mild (8–10), moderate (11–15), and severe (16–21).
The HADS questionnaire has been translated into many languages, and for many of these translations validation studies confirm the internationally applicable nature of this Questionnaire.[16] The HADS-A has been found to have an optimal cut off ≥8 (sensitivity 0.89, specificity 0.75), in relation to GAD. The HADS-D has been found to have optimal cut off ≥8 (sensitivity 0.80 and specificity 0.88) in relation to major depressive episode in general practice patients.[17]
The data were analyzed using SPSS ver 17.0. Descriptive analysis was done for sociodemographic profile. Pearson's correlation was used to find correlation between anxiety/depression level of patients and caregivers. Regression analysis was carried out to explore the relation between anxiety/depression scores of caregivers and study variables. The level of statistical significance was kept at P < 0.05.
RESULTS
We recruited seventy-five patient-caregiver dyads in the study. The mean age of the patients and caregivers was 52.43 (±3.29) years and 45.22 (±10.34) years, respectively. Eighty-eight percent patients and sixty seven percent caregivers were male. Majority of the patients and caregivers belonged to nuclear family (90%). Fifty six percent of patients were primary earning member of the family. Among the caregivers 30% were the primary earning member of the family. Seventy five percent of patients and forty three percent of caregivers were currently employed. There was no statistically significant difference between the two groups (t= 1.40, P = 0.16). The two groups did not differ significantly with regards to gender (χ2 4.01, df =1, P =0.05) and marital status (χ2 1.70, df =1, P =0.19).
Frequency distribution of the scores on HADS-Anxiety and HADS-Depression scales for the patients and caregivers has been given in Table 1 and Figure 1. Twenty four percent of the patients were diagnosed as having mild level of anxiety while 12% had moderate level of anxiety. Forty four percent of the patients were diagnosed as having clinically significant depression. It included mild (20%), moderate (18%) and severe (6%). Twenty four percent of the caregivers were diagnosed with significant anxiety features. It included mild (16%), moderate (6%), and severe (2%). Eighteen percent of the caregivers met the criteria for depression using HADS-Depression scale. It included mild (14%), moderate (2%), and severe (2%). Cramer's V- test and Phi test for 2*4 contingency table did not reveal any significant difference between the patient and care giver groups for HADS-Anxiety and HADS- Depression scales [Table 1].
Table 1.
Anxiety and depression scores of the patients and caregivers
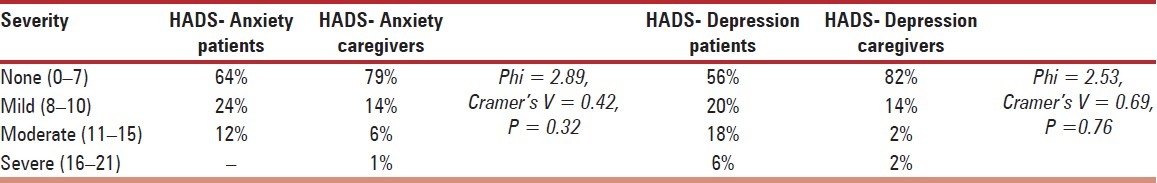
Figure 1.
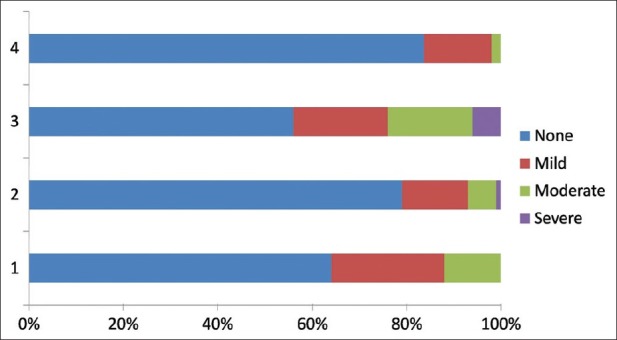
Distribution of patients and caregivers as per HADS-Anxiety and HADS-Depression scores. (1) HADS-Anxiety (Patients); (2) HADS- Anxiety (Caregivers); (3) HADS-Depression (Patients); (4) HADS-Depression (Caregivers)
No significant correlations were observed between the anxiety and depression levels of patients and caregivers. Regression analysis revealed that sex of caregivers was only significant predictor of anxiety level among caregivers (beta = 0.44, P < 0.05). No other socio-demographic variables and anxiety/ depression level of patients failed to predict anxiety level in caregivers. None of the variables was found to be a significant predictor of depression level in caregivers.
DISCUSSION
The study aimed at exploring predictors of anxiety and depression levels among caregivers of patients with stroke.
While a sizable proportion of patients as well as caregivers were found to having clinically significant levels of anxiety and depression, no significant correlation were observed between anxiety/ depression level of caregivers and patients.
Caregivers play an important role in supporting people with illness either acute or chronic. It is important to explore caregiver's emotional turmoil as it helps in exploring their burden which can have impact on the patient's illness and functioning apart from their own. The survivors of acute stroke experience long-term impairments in physical, psychosocial, and cognitive function[1,2] and rely mainly on the caregivers for practical and emotional support concerning activities of daily living.[3,4] Thus the well being of caregivers is important because the patients depend on them to uphold in the community.
Studies indicates that many factors are associated to depression and other negative outcomes in stroke patients including functioning of patient and family, stress, cognitive and behavioral problems.[18,19–21] Thus, there is a need to understand the nature, stressfulness, and effectiveness of coping in caregivers providing care to stroke patients at different times during the trajectory of recovery in order to understand the overall impact of illness.
Study from India by Raju et al,[22] found that presence of anxiety and depression were predictors of impaired quality of life in stroke survivors. Anxiety was seen in 24% patients and depression in 37% patients. In another study among 199 stroke survivors by Das et al,[23] anxiety and depression were found in 70% and 76% of caregivers, respectively. An earlier report by our group on a smaller sample of stroke patients and caregiver dyads reported significant correlation between anxiety level of male caregivers and depression level of stroke patients. Also, anxiety level of female caregivers was related to anxiety level of stroke patients.[15] However, the current study failed to find any such significant correlations.
A multitude of problems have been reported from caring such as fatigue, emotional distress, restricted social life, changes in family life, relationship difficulties, balancing responsibilities, obtaining services,[24–27] insufficient information availability, uncertainty about recovery, lack of support from clinicians, lack of caregiving skills, and financial issues.[28,29] All these factors contribute to the burden on caregivers, hence increasing their stress.
Studies in stroke caregivers recognize the burden and impact on their physical and psychological well-being.[8,12–14] The early caregiving period while feeling unprepared, the dealing with new roles, problems, and responsibilities are reported to be most difficult.[28,30] Hospitalization period following a stroke and the transition to home life are reported as the most difficult caregiving issues during the first two years by stroke caregivers with prevalence of strain in about 25–28% during the first 3–4 months of caregiving.[24,26]
The unpreparedness for stroke caregiving has been correlated with negative mood states and stress in caregivers[31,32] which show significant improvement with a problem-solving intervention.[31]
Studies report that spouses of stroke patients, especially of those who were dependent, were more likely to have symptoms of depression as compared to matched control subjects from the same community.[14]
Dennis et al,[33] reported that being severely dependent or emotionally distressed themselves on patient's part led more likely to emotional distress or depression in stroke caregivers. Studies in patients with traumatic brain injury, dementia or stroke have reported female caregivers reporting more anxiety and depression than their male counterparts.[34] Although caregiver's levels of anxiety were not observed to be clearly related to the patients’ degree of physical disability as their levels of depression.[33]
Community-based studies also report anxiety and depression in stroke caregivers along with restriction in their social activities.[8,13] Discordance in relation of anxiety and depression levels has been seen in previous studies as well. Studies from western setting have demonstrated relation between the anxiety and depression level among the caregivers and the patients′ emotional status.[14,28] Studies from western settings have demonstrated that the spouse of the stroke patients are more likely to develop depression if they are dependent of the patient and the patient was the primary earning member of the family.[28]
Levels of anxiety and depression among stroke patients has shown to impact the functional outcome.[35] Timely recognition and intervention for anxiety and depression symptoms may prevent more serious effects on neurological outcome in stroke patients.[36]
Most studies on problems faced by stroke caregivers are biased by recruiting convenience samples through clinical settings as they are likely to have greater impairment and distress than those not seeking care.[1]
The findings of the study should also be seen in light of certain limitations. We focused on certain specific predictors of association between the anxiety/ depression levels of the patients and caregivers. Certain other predictors, as noticed in other studies, were not included in the current study. Also we made cross sectional assessments. It would be interesting and insightful to follow up these patients and caregivers prospectively in order to explore the long-term outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bakas T, Austin JK, Okonkwo KF, Lewis RR, Chadwick L. Needs, concerns, strategies, and advice of stroke caregivers the first 6 months after discharge. J Neurosci Nurs. 2002;34:242–51. doi: 10.1097/01376517-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Lai SM, Studenski S, Duncan PW, Perera S. Persisting consequences of stroke measured by the Stroke Impact Scale. Stroke. 2002;33:1840–4. doi: 10.1161/01.str.0000019289.15440.f2. [DOI] [PubMed] [Google Scholar]
- 3.Sit JW, Wong TK, Clinton M, Lim LS, Fong YM. Stroke care in the home: The impact of social support on the general health of family caregivers. J Clin Nurs. 2004;13:816–24. doi: 10.1111/j.1365-2702.2004.00943.x. [DOI] [PubMed] [Google Scholar]
- 4.van Heugten C, Visser-Meily A, Post M, Lindeman E. Care for carers of stroke patients: Evidence based clinical practice guidelines. J Rehabil Med. 2006;38:153–8. doi: 10.1080/16501970500441898. [DOI] [PubMed] [Google Scholar]
- 5.Thommessen B, Aarsland D, Braekhus A, Oksengaard AR, Engedal K, Laake K. The psychosocial burden on spouses of the elderly with stroke, dementia and Parkinson's disease. Int J Geriatr Psychiatry. 2002;17:78–84. doi: 10.1002/gps.524. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Martin P, Benito-Leon J, Alonso F, Catalan MJ, Pondal M, Zamarbide I, et al. Quality of life of caregivers in Parkinson's disease. Quality of Life Research. 2005;14:463–72. doi: 10.1007/s11136-004-6253-y. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia S, Gupta A. Impairments in activities of daily living in Parkinson's disease: Implications for management. NeuroRehabilitation. 2003;18:209–14. [PubMed] [Google Scholar]
- 8.Anderson CS, Linto J, Stewart-Wynne EG. A population-based assessment of the impact and burden of caregiving for long-term stroke survivors. Stroke. 1995;26:843–9. doi: 10.1161/01.str.26.5.843. [DOI] [PubMed] [Google Scholar]
- 9.Lantz MS. Caregiver burden: When the family needs help. Clin Geriatr. 2004;12:29–32. [Google Scholar]
- 10.Ohaeri J. The burden of caregiving in families with a mental illness: A review of 2002. Curr Opin Psychiatry. 2003;16:457–65. [Google Scholar]
- 11.Cochrane JJ, Goering PN, Rogers JM. The mental health of informal caregivers in Ontario: An epidemiological survey. American Journal of Public Health. 2002;87:2002–7. doi: 10.2105/ajph.87.12.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brocklehurst JC, Andrews K, Morris PE, Richards B, Laycock PJ. Social effects of stroke. Soc Sci Med. 1981;15:35–9. doi: 10.1016/0271-7123(81)90043-2. [DOI] [PubMed] [Google Scholar]
- 13.Wade DT, Legh-Smith J, Langton Hewer R. Effects of living with and looking after survivors of a stroke. BMJ. 1986;293:418–20. doi: 10.1136/bmj.293.6544.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carnwath TCM, Johnson DAW. Psychiatric morbidity among spouses of patients with stroke. BMJ. 1987;294:409–11. doi: 10.1136/bmj.294.6569.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verma R, Sharma S, Balhara YP. A preliminary study of understanding psychological health of care givers for stroke patients. Int J Stud Res. 2011;1:118–22. [Google Scholar]
- 16.Zigmond AS, Snaith RP. The Hospital Anxiety & Depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 17.Olssøn I, Mykletun A, Dahl AA. The hospital anxiety and depression rating scale: A cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5:46. doi: 10.1186/1471-244X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark PC, Dunbar SB, Shields CG, Viswanathan B, Aycock DM, Wolf SL. Influence of stroke survivor characteristics and family conflict surrounding recovery on caregiver's mental and physical health. Nurs Res. 2004;53:406–13. doi: 10.1097/00006199-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 19.King RB, Carlson CE, Shade-Zedlow Y, Bares KK, Roth EJ, Heinemann AW. Transition to home care after stroke: Depression, physical health, and adaptive processes in support persons. Res Nurs Health. 2001;24:307–23. doi: 10.1002/nur.1032. [DOI] [PubMed] [Google Scholar]
- 20.Kotila M, Numminen H, Waltimo O, Kaste M. Depression after stroke: Results of the FINNSTROKE Study. Stroke. 1998;29:368–72. doi: 10.1161/01.str.29.2.368. [DOI] [PubMed] [Google Scholar]
- 21.Schulz R, Tompkins CA, Rau MT. A longitudinal study of the psychosocial impact of stroke on primary support persons. Psychol Aging. 1988;3:131–41. doi: 10.1037//0882-7974.3.2.131. [DOI] [PubMed] [Google Scholar]
- 22.Raju RS, Sarma PS, Pandian JD. Psychosocial problems, quality of life, and functional independence among Indian stroke survivors. Stroke. 2010;41:2932–7. doi: 10.1161/STROKEAHA.110.596817. [DOI] [PubMed] [Google Scholar]
- 23.Das S, Hazra A, Ray BK, Ghosal M, Banerjee TK, Roy T, et al. Burden Among Stroke Caregivers Results of a Community-Based Study From Kolkata, India. Stroke. 2010;41:2965–8. doi: 10.1161/STROKEAHA.110.589598. [DOI] [PubMed] [Google Scholar]
- 24.Bugge C, Alexander H, Hagen S. Stroke patients’ informal caregivers: Patient, caregiver, and service factors that affect caregiver strain. Stroke. 1999;30:1517–23. doi: 10.1161/01.str.30.8.1517. [DOI] [PubMed] [Google Scholar]
- 25.Grant JS, Glandon GL, Elliott TR, Newman Giger J, Weaver M. Caregiving problems and feelings experienced by family caregivers of stroke survivors the first month after discharge. Int J Rehabil Res. 2004;27:105–11. doi: 10.1097/01.mrr.0000127639.47494.e3. [DOI] [PubMed] [Google Scholar]
- 26.Ilse IB, Feys H, de Wit L, Putman K, de Weerdt W. Stroke caregivers’ strain: Prevalence and determinants in the first six months after stroke. Disabil Rehabil. 2008;30:523–30. doi: 10.1080/09638280701355645. [DOI] [PubMed] [Google Scholar]
- 27.MacKenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: Needs, knowledge, satisfaction, and competence in caring. Disabil Rehabil. 2007;29:111–21. doi: 10.1080/09638280600731599. [DOI] [PubMed] [Google Scholar]
- 28.King RB, Semik PE. Stroke caregiving: Difficult times, service use, and needs during the first two years. J Gerontol Nurs. 2006;32:37–44. doi: 10.3928/00989134-20060401-07. [DOI] [PubMed] [Google Scholar]
- 29.Davis LL, Grant JS. Constructing the reality of recovery: Family home care management strategies. ANS Adv Nurs Sci. 1994;17:66–76. doi: 10.1097/00012272-199412000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Johnson P. Rural Stroke Caregivers: A qualitative study of the positive and negative response to the caregiver role. Top Stroke Rehabil. 1998;5:51–68. doi: 10.1310/9WTW-R3RX-GT44-TM9U. [DOI] [PubMed] [Google Scholar]
- 31.Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002;33:2060–5. doi: 10.1161/01.str.0000020711.38824.e3. [DOI] [PubMed] [Google Scholar]
- 32.Ostwald SK, Bernal MP, Cron SG, Godwin KM. Stress experienced by stroke survivors and spousal caregivers during the first year after discharge from inpatient rehabilitation. Top Stroke Rehabil. 2009;16:93–104. doi: 10.1310/tsr1602-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dennis M, O’Rourke S, Lewis S, Sharpe M, Warlow C. A Quantitative Study of the Emotional Outcome of People Caring for Stroke Survivors. Stroke. 1998;29:1867–72. doi: 10.1161/01.str.29.9.1867. [DOI] [PubMed] [Google Scholar]
- 34.Kreutzer JS, Gervasio AH, Camplair PS. Primary Caregivers’ psychological status and family functioning after traumatic brain injury. Brain Inj. 1994;8:197–210. doi: 10.3109/02699059409150973. [DOI] [PubMed] [Google Scholar]
- 35.Lewis SC, Dennis MS, O’Rourke SJ, Sharpe M. Negative attitudes among short-term stroke survivors predict worse long-term survival. Stroke. 2001;32:1640–5. doi: 10.1161/01.str.32.7.1640. [DOI] [PubMed] [Google Scholar]
- 36.Gainotti G, Antonucci G, Marra C, Paolucci S. Relation between depression after stroke, antidepressant therapy, and functional recovery. J Neurol Neurosurg Psychiatry. 2001;71:258–61. doi: 10.1136/jnnp.71.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]


