Figure 1.
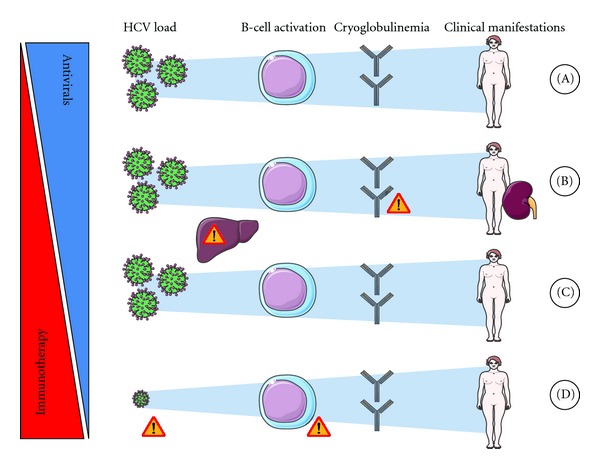
Immunotherapy to manage HCV-induced vasculitis. (A) Antiviral regimen, ideally a combination of interferon plus ribavirin, is the first-line treatment for HCV-induced cryoglobulinaemic vasculitis (CV) when the severity of its manifestations is mild-to-moderate. In addition, short-term low-dose corticotherapy may sometimes be used initially. (B) In cases of severe or life-threatening manifestations (i.e., severe renal involvement), immunotherapy must be initiated immediately. Rituximab has become a preferred choice but, as with other immunosuppressive drugs, careful monitoring of viral load and hepatic functions is necessary. Worsening of vasculitis has been reported in patients just after administration of rituximab, especially in those with serious cryocrit levels, thus, in these patients, corticosteroids and/or plasmapheresis may be initiated before B-cell depletion. An antiviral regimen is initiated either simultaneously or secondarily/sequentially in these patients. (C) When an antiviral regimen is contraindicated, poorly tolerated, or fails to induce a sustained viral remission, immunotherapy is also initiated. Corticosteroids should be avoided when possible. Careful monitoring of viral load/hepatic function is necessary. A prolonged antiviral regimen may be considered when clinical and biological manifestations of MC show an improvement under this regimen in spite of the absence of viral remission. (D) In cases where CV is still active in spite of obtaining a sustained viral response, B-cell malignancy and low-level viremia should be ruled out before considering that the vasculitis is autonomous and before initiating immunotherapy.
