Figure 1. The potential estrogenic effects on glial cells in the ischemic brain.
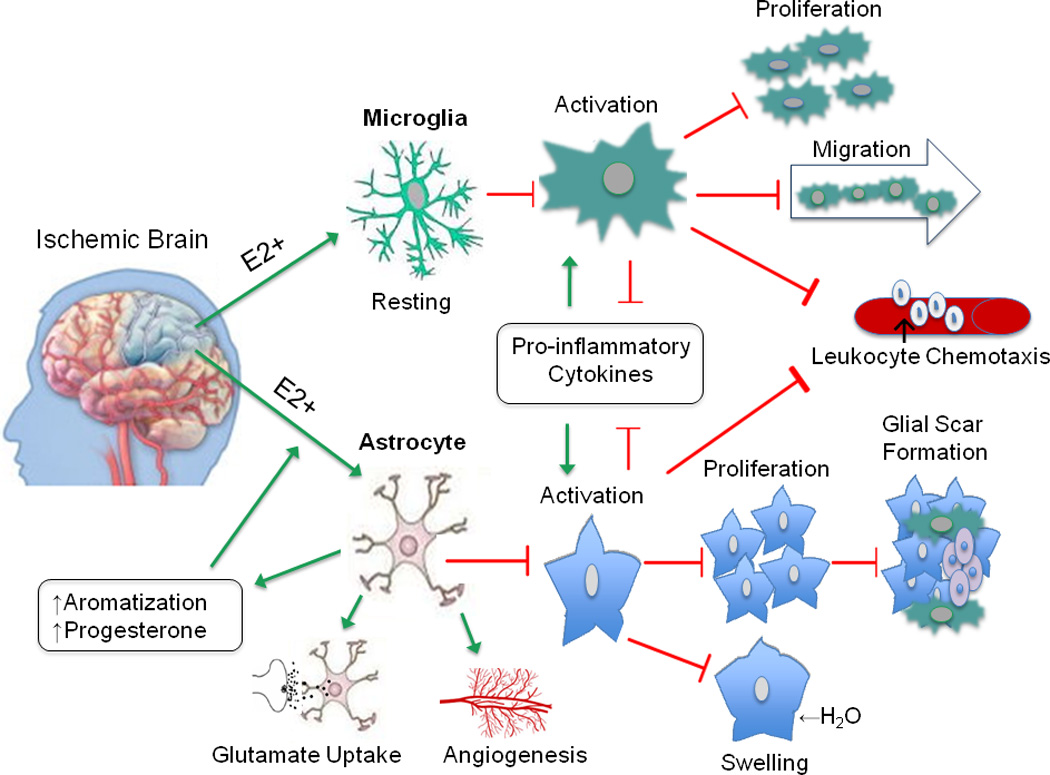
The anti-inflammatory effects of estrogen in the brain are primarily mediated by glial cells. Estrogen promotes a resting phenotype in microglia, as evidenced by increased ramified morphology and decreased MHCII expression. These actions serve to limit microglial activation, proliferation, and migration toward the injured site. Similar changes occur in astrocytes, ultimately leading to decreased glial scar formation. Estrogen-mediated decrease in aquaporin expression prevents osmotic imbalance and may lower risk of edema. Pro-inflammatory cytokines and chemoattractant signals normally released by activated astrocytes and microglia are suppressed in the presence of estrogen, thereby reducing extravasation of infiltrating immune cells. As well, estrogen enhances astrocytic expression of glutamate transporters which facilitates glutamate uptake, mitigating injury due to neuronal excitoxicity. In addition, astrocytes increase synthesis of endogenous steroid production after injury, and secrete growth factors like VEGF, which promote angiogenesis. Together, these actions have a profound impact on curbing neuronal injury due to ischemia by conferring protection via local immunosuppression. The green arrow represents enhancing or promoting action, and the red arrow represents inhibitory action.
Abbreviations: E2 (17 beta-estradiol), MHCII (major histocompatibility complex class II), VEGF (vascular endothelial growth factor)
