Abstract
Purpose
In this retrospective study, we evaluated the treatment effect of ankle joint fracture surgery involving the posterior malleolus, and discuss relevant factors influencing the occurrence of traumatic arthritis of the ankle joint.
Methods
A total of 102 cases of ankle joint fractures involving the posterior malleolus in five large-scale skeletal trauma centres in China, from January 2000 to July 2009, were retrospectively analysed in terms of surgical treatment and complete follow-up. Ankle joint mobility, posterior malleolus fragment size, articular surface evenness, Ankle-Hindfoot Scale of the American Orthopedic Foot and Ankle Society (AOFAS) score, and imaging scale score for arthritis were recorded. The degree of fracture pain during rest, active movement, and weight-bearing walking, and satisfaction with treatment were evaluated using a visual analogue scale (VAS).
Results
The average AOFAS score was 95.9, excellence rate was 92.2 %, and average VAS scores for degree of fracture pain during rest, active movement, and weight-bearing walking were 0.15, 0.31, and 0.68, respectively. Thirty-six cases showed arthritic manifestations. Ankle joint mobility along all directions on the injured side was lower than that on the unaffected side. There was no obvious difference in treatment effect between the fixed and unfixed posterior malleolus fragment groups for all and for fragment size of <25 %; between fixing the posterior malleolus fragment from front to back or from back to front; or between elderly patients (≥60 years old) and young patients (<60 years old). There was a distinct difference in the treatment effect between articular surface evenness and unevenness for all and for fragment size of ≥25 %.
Conclusions
For all 102 cases of ankle joint fracture involving the posterior malleolus, the treatment effect was satisfactory. Restoration of an even articular surface, especially when fragment size ≥25 %, should be attempted during treatment.
Introduction
Ankle joint fractures are clinically common and account for 3.92 % of all fractures sustained in the entire body [1]. Approximately 7 % to 44 % of ankle joint fractures are accompanied by posterior malleolus fractures [2, 3], which are rarely seen alone [4]. Ankle joint fractures can reportedly easily cause traumatic arthritis if it involves the posterior malleolus, and the fracture prognosis is poor [3, 5]. Some scholars have suggested that arthritis is triggered by change in the stress distribution on the articular surface, which is caused by change in the articular surface area at the distal end of the tibia after posterior malleolus fracture [6, 7]. The indications for fixation of posterior malleolus fragments are controversial. Most scholars consider that the posterior malleolus fragment should be fixed when it accounts for ≥25 % of the articular surface at the distal end of the tibia [3, 8–10]. Langenhuijsen et al. [11] believe that the posterior malleolus fragment should be fixed surgically when the fragment is ≥10 % and the articular surface at the distal end of the tibia is still uneven after internal fixation of the medial and lateral malleolus. However, reported cases are few and dependability of results needs further verification.
In this multicentre retrospective study, we evaluated the treatment effect of ankle joint fractures involving the posterior malleolus, analysed the impact of different posterior malleolus fragment sizes on the treatment effect (respectively taking 25 % and 10 % as the dividing lines), and studied the impact of screw direction during posterior malleolus fragment fixation and articular surface evenness after reduction on prognosis. The influencing factors causing traumatic arthritis during posterior malleolus fracture are also herein discussed.
Materials and methods
Patients and inclusion criteria
Patients with ankle joint fractures treated between January 2000 and July 2009 at skeletal trauma centres of five large-scale hospitals (People’s Hospital of Peking University, Jishuitan Hospital of Peking University, Xuanwu Hospital of Capital Medical University, West China Hospital of Sichuan University, and South Hospital of Southern Medical University) were evaluated.
The inclusion criteria were patients (1) with a definitive diagnosis of ankle joint fracture based on clinical and imaging technologies, (2) undergoing open reduction internal fixation surgery, (3) with involvement of the posterior malleolus, and (4) with complete clinical follow-up data.
Study method
Data collection
All workers participating in this study received unified training to fully understand the purpose and specific process of the study. All workers visited patients postoperatively, according to a unified ankle joint fracture surgery treatment follow-up form. The follow-up activity included acquisition of outpatient follow-up information. All follow-up results were inserted into a database; 102 cases of ankle joint fracture involving the posterior malleolus with complete follow-up information were selected; and further analysis was performed.
Measurement and evaluation indices
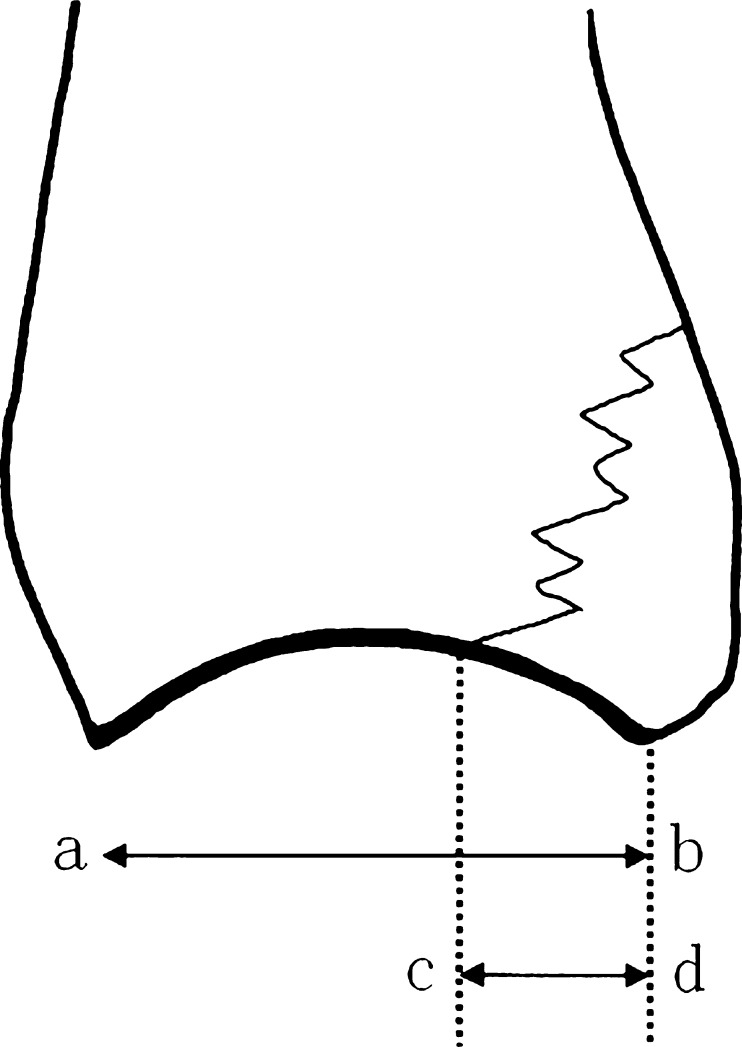
The posterior malleolus fragment size was calculated as the percentage of the involved distal tibial articular surface. The proportion of the articular surface of the fragment compared with the entire articular surface at the distal end of the tibia was measured on the lateral X-ray of the ankle joint (see Fig. 1). The articular surface was checked for evenness after reduction of the posterior malleolus fragment. The surface was determined to be even at a level of ≤1 mm and uneven at a level of >1 mm [11].
Fig. 1.
On side photograph of ankle joint, if we assume the horizontal distance between front and back points on articular surface at distal end of tibia is ab, and the horizontal distance between posterior malleolus fracture line and back point of articular surface is cd, then the percentage of fracture-involved articular surface in the whole articular surface at distal end of tibia (cd/ab) represents the size of posterior malleolus fracture block. (The Figure is provided by Langenhuijsen et al. [11])
The arthritis imaging score according to X-ray films of the ankle joint taken during the postoperative follow-up was recorded: 0 indicated a normal joint, 1 indicated osteophytes but no joint space narrowing, 2 indicated joint space narrowing with or without osteophytes, and 3 indicated disappearance or deformation of the joint space [12–14].
The evaluation indices also included the Ankle-Hindfoot Scale of the American Orthopedic Foot and Ankle Society [15] (AOFAS scale) score (excellent, ≥90; good, 75–89; acceptable, 50–74; poor, <50); fracture pain during rest, active movement, and weight-bearing walking based on a visual analogue scale (VAS) (0, pain-free; 10, the most unbearable pain); and ankle joint mobility (angle of dorsiflexion, plantar flexion, varus, and valgus during follow-up).
Statistical methods
Statistical analysis was conducted with SPSS 15.0 for Windows software and included the paired t-test, nonparametric Mann–Whitney test, and Kruskal–Wallis test. A p-value of <0.05 represented a statistically significant difference.
Results
General data
This study included 41 males and 61 females with a mean age of 43.4 (15–80) years. Causes of injuries included 13 cases of traffic injury, 36 cases of sprain, 50 cases of fall-down injury, nine cases of crush injury, and one case of falling injury. The fractures were divided into different types according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) fracture classification system [16]: there were two cases of type A (2 %), 78 cases of type B (76 %), and 22 cases of type C (22 %). The average posterior malleolus fragment size was 19.1 %. Sixteen cases (6.3 %) had a fragment size of <10 %, 24 cases (34.7 %) had a fragment size of ≥25 %, and 62 cases (16.3 %) had a fragment size of 10 % to 25 %. The posterior malleolus fragment was surgically fixed in 42 cases (41.2 %). The articular surface after reduction of the posterior malleolus fragment was even in 78 cases (76.5 %) and uneven in 24 cases (23.5 %).
Treatment effect
The follow-up period was 6.9 to 102.3 months (average, 33.8 months), and clinical union of the fracture was achieved in all patients. The AOFAS score was 95.9 ± 5.7 and included 70 excellent cases (68.6 %), 24 good cases (23.6 %), and eight acceptable cases (7.8 %); the excellence rate was 92.2 %. The average VAS score for fracture pain under different conditions was 0.15 ± 0.56 during rest, 0.31 ± 0.90 during active movement, and 0.68 ± 1.47 during weight-bearing walking. There were statistically significant differences in the VAS scores under these three conditions (χ2 = 32.125, p < 0.01). However, the average of the three groups was <1, indicating only slight pain. The average satisfaction with treatment was 9.62 ± 0.56 (7–10). Thirty-six cases (35.2 %) showed arthritic manifestations according to imaging results, including 31 cases (86.1 %) with a score of 1, and 5 cases (14.9 %) with a score of 2. For cases with or without arthritic manifestations, the VAS fracture pain score under different conditions showed no statistical differences (p > 0.05).
Statistical analysis
Ankle joint mobility was compared between the injured and unaffected sides. The paired t-test results showed significant differences in ankle joint mobility along all directions between the injured and unaffected sides (p < 0.05). (see Table 1).
Table 1.
Comparison of ankle joint mobility on injured side and unaffected side
| Dorsiflexion | Plantar flexion | Valgus | Varus | |
|---|---|---|---|---|
| Injured side | 17.2 ± 9.0° | 45.4 ± 9.8° | 8.2 ± 5.1° | 15.4 ± 6.7° |
| Unaffected side | 24.1 ± 8.7° | 49.5 ± 7.1° | 9.5 ± 5.3° | 16.3 ± 6.2° |
| t value | −9.501 | −5.293 | −2.161 | −2.494 |
| P value | 0.000 | 0.000 | 0.033 | 0.014 |
Comparison was also performed between the fixed and unfixed posterior malleolus fragment groups. The fixed group comprised 42 cases with an average fragment size of 28.5 % (11.1 %–55.0 %); the unfixed group comprised 60 cases with an average fragment size of 12.5 % (1.5 %–24.3 %). The posterior malleolus fragment size and arthritis score of the two groups showed statistically significant differences, while the difference in the AOFAS score, VAS rating under various conditions, and patient satisfaction rating showed no statistically significant differences (see Table 2). The average surgically fixed posterior malleolus fragment size was larger than the average unfixed posterior malleolus fragment size, which indicates that the larger the posterior malleolus fragment, the greater the potential for successful surgical fixation. Comparison of the AOFAS score, VAS rating, and patient satisfaction showed that there was no statistical difference in the treatment effect between the fixed and unfixed posterior malleolus fragment groups. The difference in the arthritis score may have been related to the posterior malleolus fragment size, which was further statistically analysed (below). In the fixed and unfixed posterior malleolus groups, the articular surface after fracture reduction was even in 27 and 49 cases, respectively. Comparison showed that the difference was statistically significant (p = 0.047); i.e., the even articular surface accounted for a higher number of cases in the unfixed group. In the fixed group, a large posterior malleolus fragment, serious injury, and difficult reduction of the articular surface may have caused the low proportion of even articular surfaces.
Table 2.
Comparison between fixed and unfixed posterior malleolus fragment groups
| Fixed (n = 42) | Unfixed (n = 60) | P value | |
|---|---|---|---|
| Size of posterior malleolus fragment (%) | 28.5 ± 9.2 | 12.5 ± 4.9 | 0.000 |
| AOFAS scale | 95.0 ± 6.1 | 96.5 ± 5.5 | 0.203 |
| VAS during rest | 0.15 ± 0.50 | 0.15 ± 0.60 | 0.995 |
| VAS during active movement | 0.37 ± 0.80 | 0.26 ± 0.96 | 0.537 |
| VAS during weight-bearing | 0.73 ± 1.31 | 0.64 ± 1.59 | 0.771 |
| Patient satisfaction | 9.57 ± 0.63 | 9.69 ± 0.44 | 0.328 |
| Arthritis scale | 1 (0–2) | 0 (0–2) | 0.000 |
Note: The arthritis scale is expressed in modal numbers, with the scale range in brackets.
All posterior malleolus fracture cases were divided into two groups, according to articular surface evenness after reduction to compare the posterior malleolus fragment size, AOFAS score, VAS score, patient satisfaction, and arthritis score. Distinct differences were shown in the posterior malleolus fragment size, AOFAS score, arthritis score, and patient satisfaction, while there was no statistical difference in the VAS score under the three conditions (see Table 3). These results indicate that the articular surface reduction level affects the prognosis of the posterior malleolus fracture, and that the posterior malleolus fragment size influences articular surface evenness.
Table 3.
Comparison between patients with even and uneven articular surfaces after reduction
| Even (n = 24) | Uneven (n = 78) | P value | |
|---|---|---|---|
| Age of patients | 41.9 ± 16.4 | 48.2 ± 15.4 | 0.100 |
| Size of posterior malleolus fragment (%) | 17.8 ± 10.2 | 23.1 ± 11.2 | 0.033 |
| AOFAS scale | 96.9 ± 4.8 | 92.6 ± 7.3 | 0.010 |
| VAS during rest | 0.08 ± 0.36 | 0.38 ± 0.92 | 0.128 |
| VAS during active movement | 0.17 ± 0.50 | 0.75 ± 1.56 | 0.086 |
| VAS during weight-bearing | 0.59 ± 1.47 | 0.97 ± 1.47 | 0.277 |
| Patient satisfaction | 9.71 ± 0.43 | 9.33 ± 0.80 | 0.037 |
| Arthritis scale | 0 (0–1) | 1 (0–2) | 0.000 |
All cases were divided into three groups (<10 %, 10 %–25 %, and ≥25 %) by taking 10 % and 25 % (posterior malleolus fragment size) as the dividing lines to compare the treatment effect among the three groups. There were no statistical differences in the AOFAS and VAS scores under various conditions, while there were statistically significant differences in patient satisfaction and arthritis score (see Table 4). Patient satisfaction was lowest when fragments were <10 % and highest when fragments were 10 % to 25 %. The average patient satisfaction value was >9 in all groups, indicating that the overall treatment effect was satisfactory. The arthritis score for different posterior malleolus fragment sizes differed greatly, indicating that the posttraumatic arthritis may be related to the fragment size.
Table 4.
Treatment effect comparison between different posterior malleolus fragment groups by size
| <10 % (n = 16) | 10–25 % (n = 62) | ≥25 % (n = 24) | P value | |
|---|---|---|---|---|
| AOFAS | 95.6 ± 7.0 | 96.8 ± 4.8 | 93.7 ± 6.6 | 0.141 |
| VAS during rest | 0.29 ± 1.00 | 0.09 ± 0.33 | 0.21 ± 0.64 | 0.415 |
| VAS during active movement | 0.51 ± 1.74 | 0.18 ± 0.45 | 0.51 ± 0.95 | 0.105 |
| VAS during weight-bearing | 0.52 ± 1.23 | 0.60 ± 1.47 | 0.98 ± 1.65 | 0.240 |
| Patient satisfaction | 9.25 ± 0.84 | 9.73 ± 0.47 | 9.60 ± 0.09 | 0.023 |
| Arthritis scale | 0 (0–1) | 0 (0–2) | 1 (0–2) | 0.001 |
We respectively analysed the relationship between articular surface evenness after fracture reduction and prognosis among the three above-described posterior malleolus fragment groups (<10 %, 10 %–25 %, and ≥25 %) (see Table 5). The AOFAS and VAS scores in the three groups showed no significant differences. Comparison of the arthritis score showed that this index was significantly different among the various fragment groups. Patient satisfaction differed greatly only in the group with a fragment size of <10 %, but the reliability of statistical results was not high because of the small sample number in this group. According to the average value of the different evaluation indices in these groups, for patients with even articular surfaces, AOFAS score and patient satisfaction were higher, while VAS score for fracture pain under different conditions was lower than that of patients with uneven articular surfaces.
Table 5.
Comparison of articular surface evenness with different posterior malleolus fragment sizes
| <10 % (n = 16) | 10 %–25 % (n = 62) | ≥25 % (n = 24) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Even n = 13 | Uneven n = 3 | P value | Even n = 48 | Uneven n = 14 | P value | Even n = 17 | Uneven n = 7 | P value | |
| AOFAS scale | 97.0 ± 6.1 | 89.3 ± 8.6 | 0.087 | 97.4 ± 4.2 | 94.7 ± 6.4 | 0.152 | 95.3 ± 5.4 | 89.7 ± 7.9 | 0.055 |
| Arthritis scale | 0 (0–1) | 1 | 0.016 | 0 (0–2) | 1 (0–2) | 0.000 | 1 (0–1) | 1 (1–2) | 0.007 |
| VAS during rest | 0.05 ± 0.14 | 1.33 ± 2.31 | 0.439 | 0.04 ± 0.15 | 0.29 ± 0.61 | 0.155 | 0.22 ± 0.73 | 0.17 ± 0.37 | 0.860 |
| VAS during active movement | 0.09 ± 0.19 | 2.33 ± 4.04 | 0.438 | 0.12 ± 0.37 | 0.36 ± 0.63 | 0.206 | 0.37 ± 0.84 | 0.86 ± 1.18 | 0.263 |
| VAS during weight-bearing | 0.26 ± 1.67 | 0.31 ± 2.89 | 0.488 | 0.58 ± 1.60 | 0.66 ± 0.90 | 0.870 | 0.85 ± 1.63 | 1.29 ± 1.78 | 0.571 |
| Patient satisfaction | 9.54 ± 0.48 | 8.00 ± 1.00 | 0.001 | 9.76 ± 0.41 | 9.61 ± 0.63 | 0.400 | 9.69 ± 0.43 | 9.36 ± 0.48 | 0.104 |
For a posterior malleolus fragment size of <25 %, the malleolus fracture was fixed in 18 cases and unfixed in 60 cases. Comparison of the treatment effect in the two groups shows a statistical significant difference in the posterior malleolus fragment size, while there were no statistical differences in the AOFAS score, VAS score, patient satisfaction, and arthritis score (see Table 6). This shows that among fragments of <25 %, larger fragments are inclined to fixation, but whether fixation occurs does not affect the treatment effect.
Table 6.
Comparison between fixation and nonfixation of posterior malleolus for fragments of <25 %
| Fixing (n = 18) | Unfixing (n = 60) | P value | |
|---|---|---|---|
| Size of posterior malleolus fragment (%) | 20.4 ± 3.4 | 12.4 ± 5.0 | 0.000 |
| AOFAS | 96.8 ± 5.0 | 96.5 ± 5.5 | 0.848 |
| VAS during rest | 0.08 ± 0.24 | 0.15 ± 0.60 | 0.611 |
| VAS during active movement | 0.19 ± 0.51 | 0.26 ± 0.96 | 0.759 |
| VAS during weight-bearing | 0.39 ± 0.52 | 0.64 ± 1.59 | 0.519 |
| Patient satisfaction | 9.80 ± 0.39 | 9.57 ± 0.63 | 0.066 |
| Arthritis scale | 0 (0–2) | 0 (0–2) | 0.134 |
Among 42 cases involving fixation of the posterior malleolus fragment, 23 underwent back-to-front fixation with an average fragment size of 29.4 % (14.8 %–55.0 %); the remaining 19 cases underwent front-to-back fixation with an average fragment size of 27.5 % (11.1 %–45.4 %). The impact of different fixation directions on the treatment effect was statistically analysed. The results showed no obvious difference (see Table 7), which indicates that fixation direction of the posterior malleolus fragment exerts no impact on the treatment effect. In the front-to-back fixation group, the articular surface was even in 13 cases and uneven in six cases; in the back-to-front fixation group, the articular surface was even in 15 cases and uneven in eight cases. No statistical significant difference was found after comparison of the two groups (χ2 = 0.048, p > 0.05).
Table 7.
Comparison between front-to-back and back-to-front fixation
| Back-to-front fixing (n = 23) | Front-to-back fixing (n = 19) | P value | |
|---|---|---|---|
| Size of posterior malleolus fragment (%) | 29.4 ± 10.1 | 27.5 ± 8.2 | 0.499 |
| AOFAS scale | 95.8 ± 6.7 | 94.1 ± 5.3 | 0.389 |
| VAS during rest | 0.22 ± 0.65 | 0.07 ± 0.23 | 0.333 |
| VAS during active movement | 0.32 ± 0.73 | 0.44 ± 0.89 | 0.648 |
| VAS during weight-bearing | 0.55 ± 0.70 | 0.95 ± 1.80 | 0.371 |
| Patient satisfaction | 9.70 ± 0.45 | 9.67 ± 0.44 | 0.874 |
| Arthritis scale | 0 (0–1) | 1 (0–1) | 0.557 |
The treatment effect between elderly and young patients was compared. We divided the cases into two groups: the elderly group (≥60 years of age, n = 18) and middle-aged/young group (<60 years of age, n = 84). The posterior malleolus fragment size, AOFAS score, VAS score, patient satisfaction, and arthritis score were analysed. There was no statistical difference in the above indices with the exception of the arthritis score (see Table 8). This indicates that the treatment effect between elderly and middle-aged/young patients was basically the same, but the arthritis score in elderly patients was higher than that in middle-aged/young patients.
Table 8.
Comparison between elderly and middle-aged/young groups
| Middle-aged and young group (n = 84) | Elderly group (n = 18) | P value | |
|---|---|---|---|
| Size of posterior malleolus fragment (%) | 18.9 ± 10.8 | 20.0 ± 10.1 | 0.673 |
| AOFAS scale | 96.1 ± 5.5 | 94.9 ± 6.8 | 0.417 |
| VAS during rest | 0.13 ± 0.44 | 0.24 ± 0.94 | 0.469 |
| VAS during active movement | 0.21 ± 0.58 | 0.76 ± 1.70 | 0.196 |
| VAS during weight-bearing | 0.67 ± 1.52 | 0.72 ± 1.29 | 0.888 |
| Patient satisfaction | 9.63 ± 0.55 | 9.57 ± 0.59 | 0.688 |
| Arthritis scale | 0 (0–2) | 1 (0–2) | 0.044 |
Discussion
This study showed that ankle joint mobility along all directions on the injured side was lower than that on the unaffected side, indicating that posterior malleolus fracture can greatly affect ankle joint mobility. However, from the perspective of overall treatment effect, the average AOFAS score was 95.9; the excellence rate was 92.2 %; and the average VAS scores for fracture position during rest, active movement, and weight-bearing walking were 0.15, 0.31, and 0.68, respectively, which are higher than those reported by other studies [11, 17]. Average patient satisfaction with treatment reached a score of 9.62, demonstrating that the treatment effect in this group was satisfactory.
Comparison of the fixed and unfixed posterior malleolus groups showed that the posterior malleolus fragment in the fixed group was significantly larger than that in the unfixed group. The arthritis score also differed greatly, but the AOFAS and VAS scores did not show obvious statistical differences. De Vries [9] and Langenhuijsen et al. [11] also reported that fragment sizes differ greatly, but there were no statistical differences in functional and VAS scores between fixed and unfixed posterior malleolus fragments. However, these papers evaluated few posterior malleolus fixation cases (11–14 cases), so the results reliability is low.
We analysed the relationship between articular surface evenness and prognosis of posterior malleolus fracture. The results showed that an even articular surface is accompanied by a smaller fragment and that its AOFAS score, patient satisfaction, and arthritis score are better than those of an uneven articular surface. This indicates that the posterior malleolus fragment size is related to the achievement of anatomical reduction of the articular surface. The larger the posterior malleolus fragment, the more damaging the force. Thus, the difficulty of achieving articular surface reduction is increased.
We divided the fragments into three groups (<10 %, 10 %–25 %, and ≥25 %), by taking 10 % and 25 % as the dividing lines. After statistical analysis of the treatment effect among the three groups, we found great differences in patient satisfaction and arthritis score. Arthritis was most serious when the fragment was ≥25 %, while satisfaction was highest when the fragment size was 10 % to 25 %. However, the average score of all three groups was >9. Lindsjo [8], and Broos and Bisschop [18] stated that the treatment effect is poor for patients with large fragments. De Vries [9] did not find a relationship between fragment size and long-term prognosis. He believes that this may have been due to an insufficient sample size. We further analysed the relationship between articular surface evenness and prognosis with various fragment sizes. Among the three groups, the arthritis score in patients with uneven articular surfaces was higher than that in patients with even articular surfaces. In the group with fragments of <10 %, satisfaction of patients with even articular surfaces was higher than that of patients with uneven articular surfaces. In the other fragment groups, there was no obvious correlation between articular surface evenness and prognosis. However, according to the average values, the treatment effect in patients with even articular surfaces was better in all groups. This reminds us to attempt anatomical reduction of the posterior malleolus fragment to reduce subsequent traumatic arthritis risk. When the posterior malleolus fragment is ≥25 %, arthritis severity exceeds that of fragments of <25 %, regardless of the surgical fixation effect. Analysis of all cases showed that articular surface evenness was related to prognosis, but the relationship was not obvious among different fragment sizes. One possibility is that the decreased number of samples after grouping caused deviation in the results.
There are always disputes on the indication for posterior malleolus fragment fixation. Raasch et al. [19] and Fitzpatrick et al. [20] considered that posterior malleolus fractures can be stably reduced under general conditions without fixation, as long as the medial and lateral malleolus are intact or the fracture position is firmly fixed; posterior malleolus fractures with poor reduction during the first phase may subsequently undergo a natural reduction process if they are not fixed; the natural correction opportunity is lost if fixation is performed in poorer positions. Papachristou found that ankle joint stress is mainly concentrated in the two middle quarters of the articular surface area, while the rear quarter of the articular surface hardly bears a load [21]. Posterior malleolus fixation is performed in all cases with fragments of ≥25 %, so we cannot compare the treatment effect of fixed and unfixed fragments of ≥25 %. However, for fragments of <25 %, we compared the treatment effect with and without fixation. Fixation of the posterior malleolus fragment did not greatly affect the treatment effect. However, such a result based on a retrospective study is not adequate to indicate that no fixation is required when the fragment is <25 % and only provides a reference value. Lack of clear biomechanical proof and universal standard quantification indices for evaluation of the ankle joint fracture treatment effect is another reason for unclear posterior malleolus fixation indications [22–24].
There are also disputes on the posterior malleolus fixation mode, including front-to-back and back-to-front fixation. Both have advantages and disadvantages. The former is simple in operation and convenient in removal, but it is difficult to reach firm pressurisation. While the latter has a sound pressurisation effect, the operation and removal during the second phase are difficult. We statistically analysed the two fixation modes. There were no statistical differences in the AOFAS, VAS, arthritis, and patient satisfaction scores under the two modes, which reminds us to ensure a satisfactory effect by using front-to-back fixation. Mingo-Robinet et al. [17] reported 45 cases of posterior malleolus fracture, including 18 cases involving posterior malleolus fixation. Among 15 cases of front-to-back fixation, fragment reduction was affected in six because the screw thread appeared in the fracture line. Three cases of back-to-front fixation achieved anatomical reduction. We also noticed this problem during treatment; the thread must penetrate the rear cortex of the posterior malleolus when conducting front-to-back fixation. Back-to-front fixation should be adopted if the fracture bone is small enough to achieve good pressurisation. In this study, the proportion of articular surface evenness under different directions showed no statistical difference between the two.
In this study, 36 cases showed traumatic arthritis manifestations based on imaging, accounting for 35.2 % of all cases. When we compared the treatment effect in different posterior malleolus fracture groups, the arthritis score always showed a statistically significant difference, but a hybrid effect often existed between various factors. Comparison of the treatment effect with different articular surface evenness showed that the AOFAS score and patient satisfaction with treatment in patients with an even articular surface were significantly higher than those in patients with an uneven articular surface. This reminds us to pay more attention to the reduction quality of the posterior malleolus fragment when treating posterior malleolus fracture to acquire an even articular surface after reduction.
In terms of measurement of the posterior malleolus fragment size, Langenhuijse, Mingo-Robinet, other authors, and we ourselves adopted the proportion of linear distance between two points on the articular surface and the fracture line [11, 17]. However, this method may not be accurate because the posterior malleolus fracture line is not often perfectly perpendicular to the lateral X-ray plane, which results in overestimation or underestimation of the posterior malleolus fragment size. Ferries et al. [25] pointed out that the credibility for determining fragment size by common plane films is low, and the error rate is very high, even for experienced inspectors. Moreover, the articular surface at the distal end of the tibia is a curve surface rather than a flat surface; thus, estimation of fragment size using only the proportion of the distance between the two points can also cause error. Magid et al. [26] and Haraguchi et al. [27] proposed that the calculation method for fragment size based on CT images is more accurate.
Conclusion
For all 102 cases of ankle joint fracture involving the posterior malleolus, the treatment effect was satisfactory. After reduction of the posterior malleolus fragment, articular surface evenness at the distal end of the tibia will affect the treatment effect of posterior malleolus fracture; therefore, we should attempt to restore an even articular surface especially when fragment size ≥25 % during treatment.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Bao-guo Jiang, Email: jiangbaoguo@vip.sina.com.
Hui-liang Shen, Email: shenhuiliang@medmail.com.cn.
References
- 1.Salai M, Dudkiewicz I, Novikov I, Amit Y, Chechick A. The epidemic of ankle fractures in the elderly–is surgical treatment warranted? Arch Orthop Trauma Surg. 2000;120(9):511–513. doi: 10.1007/s004020000172. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures–an increasing problem? Acta Orthop Scand. 1998;69(1):43–47. doi: 10.3109/17453679809002355. [DOI] [PubMed] [Google Scholar]
- 3.Hai-lin XU, Li-min LIU, Bao-guo JIANG, et al. Multicenter follow-up study of ankle fracture surgery. Chinese Medical Journal. 2012;125(4):574–578. [PubMed] [Google Scholar]
- 4.Neumaier Probst E, Maas R, Meenen NM. Isolated fracture of the posterolateral tibial lip (Volkmann's triangle) Acta Radiol. 1997;38(3):359–362. doi: 10.1080/02841859709172083. [DOI] [PubMed] [Google Scholar]
- 5.Olerud C, Molander H. Bi- and trimalleolar ankle fractures operated with nonrigid internal fixation. Clin Orthop Relat Res. 1986;206:253–260. [PubMed] [Google Scholar]
- 6.McKinley TO, Rudert MJ, Koos DC, Brown TD. Incongruity versus instability in the etiology of posttraumatic arthritis. Clin Orthop Relat Res. 2004;423:44–51. doi: 10.1097/01.blo.0000131639.89143.26. [DOI] [PubMed] [Google Scholar]
- 7.Schatzker J, Tile M. The Rationale of Operative Fracture Care. New York: Springer-Verlag; 1987. [Google Scholar]
- 8.Lindsjö U. Operative treatment of ankle fracture-dislocations. A follow-up study of 306/321 consecutive cases. Clin Orthop Relat Res. 1985;199:28–38. [PubMed] [Google Scholar]
- 9.Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. 2005;44(3):211–217. doi: 10.1053/j.jfas.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Zhao H, Yang Y, Yu G, Zhou J. A systematic review of outcome and failure rate of uncemented Scandinavian total anklereplacement. Int Orthop. 2011;35(12):1751–1758. doi: 10.1007/s00264-011-1339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma. 2002;53(1):55–60. doi: 10.1097/00005373-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25(6):737–745. doi: 10.1177/036354659702500603. [DOI] [PubMed] [Google Scholar]
- 13.Morrey BF, Wiedeman GP., Jr Complications and long-term results of ankle arthrodeses following trauma. J Bone Joint Surg Am. 1980;62(5):777–784. [PubMed] [Google Scholar]
- 14.Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998;19(7):466–471. doi: 10.1177/107110079801900708. [DOI] [PubMed] [Google Scholar]
- 15.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 16.Lee YS, Chen SW. Lateral fixation of open AO type-B2 ankle fractures: the Knowles pin versus plate. Int Orthop. 2009;33(4):1135–1139. doi: 10.1007/s00264-008-0617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mingo-Robinet J, López-Durán L, Galeote JE, Martinez-Cervell C. Ankle fractures with posterior malleolar fragment: management and results. J Foot Ankle Surg. 2011;50(2):141–145. doi: 10.1053/j.jfas.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Broos PL, Bisschop AP. Operative treatment of ankle fractures in adults: correlation between types of fracture and final results. Injury. 1991;22(5):403–406. doi: 10.1016/0020-1383(91)90106-O. [DOI] [PubMed] [Google Scholar]
- 19.Raasch WG, Larkin JJ, Draganich LF. Draganich, Assessment of the posterior malleolus as a restraint to posterior subluxation of the ankle. J Bone Joint Surg Am. 1992;74(8):1201–1206. [PubMed] [Google Scholar]
- 20.Fitzpatrick DC, Otto JK, McKinley TO, Marsh JL, Brown TD. Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma. 2004;18(5):271–278. doi: 10.1097/00005131-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Papachristou G, Efstathopoulos N, Levidiotis C, Chronopoulos E. Early weight bearing after posterior malleolar fractures: an experimental and prospective clinical study. J Foot Ankle Surg. 2003;42(2):99–104. doi: 10.1016/S1067-2516(03)70009-X. [DOI] [PubMed] [Google Scholar]
- 22.Bekerom MP, Haverkamp D, Kloen P. Biomechanical and clinical evaluation of posterior malleolar fractures. A systematic review of the literature. J Trauma. 2009;66(1):279–284. doi: 10.1097/TA.0b013e318187eb16. [DOI] [PubMed] [Google Scholar]
- 23.Rukavina A. The role of fibular length and the width of the ankle mortise in post-traumatic osteoarthrosis after malleolar fracture. Int Orthop. 1998;22(6):357–360. doi: 10.1007/s002640050277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E. Distal tibia fractures: management and complications of 101 cases. Int Orthop. 2010;34(4):583–588. doi: 10.1007/s00264-009-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma. 1994;8(4):328–331. doi: 10.1097/00005131-199408000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Magid D, Michelson JD, Ney DR, Fishman EK. Adult ankle fractures: comparison of plain films and interactive two- and three-dimensional CT scans. AJR Am J Roentgenol. 1990;154(5):1017–1023. doi: 10.2214/ajr.154.5.2108536. [DOI] [PubMed] [Google Scholar]
- 27.Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88(5):1085–1092. doi: 10.2106/JBJS.E.00856. [DOI] [PubMed] [Google Scholar]