A health disparity is a particular type of difference in health (or in the determinants of health that could be shaped by policies) in which disadvantaged social groups systematically experience worse health or more health risks than do more advantaged social groups (Braveman, 2009, p. 1).
Over the past several years, health policy-makers have directed increased attention to issues of health disparities; an issue that has concerned the nursing profession for over a century. Indeed, the nursing profession is uniquely suited to address these issues of healthcare disparities through research and practice. According to The International Council of Nursing (2010), nurses are concerned with the “… advocacy [and] promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education. …” to improve the health and well being of others. Nursing has made a substantial contribution of research in health related concerns of vulnerable populations (Flaskerud, et al., 2002). Reuter and Kushner (2010) advocate that addressing health inequities are well within the nursing mandate, and yet is an underutilized role. The authors suggest that a “…’critical care approach’ that will assist nurses to understand the social, political, economic and historical context of health inequities…” be adopted.
Nursing historical research lends insight into the complex health issues that nurses face today, and may guide policy and nursing practice. In a previous edition of Journal of Pediatric Nursing, Connolly and Gibson (2010) used an historical case exemplar to examine how policies and nursing practice for children with tuberculosis during 1900–1935 still has implications to nursing practice today. Using a similar approach, this article will address how the development of the public health nurses’ role and influence related to infant mortality during 1884–1920 can improve our understanding of current nursing practice. Despite not having full understanding about the cause (s) of infant mortality, nurses used creativity and ingenuity to address the conditions they knew were compounding the problem. Gaining a better understanding of how nurses delivered care and improved the health of a vulnerable population a century ago will help contemporary nurses explore the contributing factors of poverty, environment, and culture that make certain children more at risk for health problems in the United States today.
Methods
This research was completed using traditional historical methods with a social history framework and is an extension of the work of nurse historians Connolly (2005) and Brodie (1991). Questions that guided this research were: “What was the state of the art of medicine and nursing regarding childhood malnutrition in the late 19th and early 20th century?” “How did ethnicity and class influence the care given and what were the socio-economic and political issues of the time?” The historical records of the Providence District Nurses Association, housed at the Rhodes Island Historical Society, were used as a case study to examine these questions. Other sources included the online records of the Children’s Bureau (Lathrop, 1918–1919); as well as articles from professional journals covering the time span of 1885–1920, such as The American Journal of Nursing, Public Health Nurse, Public Health Nursing Quarterly and The Trained Nurse and Hospital Review. In addition, secondary sources used were from noted nursing, medical and social historians such as Cynthia Connolly, Barbara Brodie, Karen Buhler-Wilkerson, Roma Apple, Howard Markel, Richard Meckel, and Nancy Tomes. Data were subjected to external and internal criticism, then organized and examined for emerging themes, and subsequently analyzed within the social, political, and economic context of the early 20th century. The state of the art of medicine and nursing at the turn of the century were also taken into account. The results were written into a cohesive narrative.
Understanding the Problem
Another important duty the nurse had to perform was to help lay out the baby. It was not unusual to lay out several in one week. Mothers in poor sections were helpless. Johnnie had to die - it was his second summer. It did not occur to any one that he probably would have died in his first summer had he been subjected to the same diet as in his second (Mary S. Gardner, 1913, p. 31).
In 1913, public health nurse (PHN) Mary Gardner wrote in the Annual Report of the Providence District Nursing Association, expressing the reality of infant mortality nearly a century ago. The mortality rate of children less than two years of age was estimated to be over 15–20%; and of those infant’s who died, 40–50% of deaths were due to digestive related illnesses (Meckel, 1990). Especially during the summer months, infant mortality rates soared as infants perished from “summer diarrhea,” also known as “summer complaint” or “cholera infantum.” This illness consisted of 8–12 days of diarrhea followed by vomiting, thirst, dehydration and emaciation. Sick infants would be unable to retain any nourishment and would continue having vomiting and diarrhea until they fell into a coma and eventually died.
The precise cause of summer diarrhea is still unknown today; however, it was most likely a gastrointestinal infection from a strain of E. coli, Salmonella or Shigella bacteria, or possibly Rotavirus (Meckel, 1990). Although Pasteur had introduced the germ theory of disease in the 1860s, it was not fully accepted and integrated into medical practice until the 1900s. Prior to the acceptance of germ theory, the prevailing disease theory was miasmata, or zymotic theory of disease, linking disease with noxious elements in the air from putrid decay of filth and debris. Medical care was directed at ameliorating the effects of living in unsanitary conditions. Keeping homes and persons sanitary was seen as the best way to ward off disease. Child welfare took on an unprecedented importance during this time, as sanitation and hygiene were seen as a means to combat infant mortality. In fact, this is often referred to as the “child-saving” movement (Meckel).
New Era in Public Health
Due to a massive number of people immigrating to the United States, by the late 19th century major cities had difficulties meeting the housing and sanitation needs of their residents. Tenements were closely spaced, lacked ventilation and natural light and had no hot water for bathing. Disease spread rapidly and poor health was a natural consequence of living in these conditions (Meckel, 1990). Among the charitable organizations formed to relieve the suffering of the urban poor, were district nursing organizations modeled after the English system implemented by William Rathbone in 1859. Following the sanitation leadership of Florence Nightingale, the District Nurses used “elements of modern hygiene,” including sunshine, cleanliness, fresh air and wholesome food (Buhler-Wilkerson, 2001). Nurses, who were trained in “… understanding of children, nutrition, psychology, education and social policy courses” (McClelland, 1913, p 19), provided home visiting services to the sick. Many of the nurses who worked in these district nursing organizations called themselves public health nurses (PHN) and is the term used hereafter in this article.
With the acceptance of germ theory, in the late 19th century medical care began to change with the understanding that germs “the seeds of contagion,” not filth, were the cause of disease. A new era in public health began where disease prevention looked not only at the home environment, but also outward towards the many potential sources of infection. Public health practitioners advocated for broader changes to prevent the spread of disease, such as “land drainage, sewer construction and the like.…” (Tomes, 1998, p. 23). It became clear that an interplay of factors, biological, environmental and economic, were contributing to the high infant mortality rate. Nurses played an important role in identifying these causative factors and finding solutions that eventually reversed the infant mortality rate.
Inadequate Nutrition
By the late 19th century, the medical profession began to recognize the role that adequate nutrition played in infant health and mortality (Meckel, 1990). Although public health nurses and physicians were working with mothers to encourage breast feeding, which was understood to be the best food for baby, rates of breastfeeding were declining. As a result, the need for cow’s milk formulas that would adequately meet infants’ nutritional needs was a growing concern (Schwab, 1996). The demand for clean milk was especially high in the homes of the poor, where it was a necessity for the mother to work, or the mother was too ill to breastfeed the child. In some cases, mothers took matters into their own hands and fed their infant proprietary foods, such as Mellin’s milk modifier or Borden’s sweetened condensed milk, which were advertised directly to mothers through magazines and at grocery stores (Apple, 1987). Although these foods were advertised to be a “perfect substitute for Mother’s milk,” in reality they did not meet the nutritional needs of infants. Infants fed on these diets suffered malnutrition and scurvy and/or rickets was often a consequence (Apple, p. 8).
Thus in 1884 a Philadelphia physician, Arthur Meig, began searching for the best substitute for mother’s milk. Meig identified the components of cow’s milk and human milk and recommended modification of cow’s milk for infants to make it more closely resemble human milk. (Apple, 1987).1 However, the right composition of formula was not the only concern. With the advent of germ theory, medical scientists discovered that diseases such as typhoid, scarlet fever, diphtheria and tuberculosis were being transmitted via cow’s milk (Meckel, 1990) and physicians debated over the best method for producing clean, healthy cow’s milk. Some physicians advocated for certified raw milk, a process whereby milk was produced in clean dairy farms, where cows received standard feeding and living conditions and milk was processed cleanly (Apple). Other physicians advocated for the pasteurization of milk to kill off harmful bacteria. Despite concerns that important nutrients in the milk were lost during pasteurization, a perfected version of this method was eventually adopted as the acceptable method to provide clean, safe milk, which retained the important nutrients (Meckel).2
Milk Dispensaries: Finding Something That Worked
In 1893 Nathan Straus, a New York City philanthropist, established milk stations to better regulate the sale and distribution of clean, pasteurized cow’s milk to infants (Connolly, 2005). Before the advent of milk stations, milk was often days old before it reached the small groceries in the city neighborhoods. Milk would be collected from cows with unwashed utters and transported to cities unrefrigerated for days in uncovered containers (Meckel, 1990). By the time mothers bought the milk it was grey colored and tasted bad. To the spoiled milk, middleman buyers added chalk, bicarbonate of soda, molasses and sugar to improve the color and hide the spoiled milk taste. In addition, middleman buyers would often skim the cream off the milk and added water without buyer’s knowledge. In the early 1900s, with the scientific methods of analyzing milk and the new laws governing the sale of milk, the pure milk dispensary was a vital means for infants to obtain the nutrition they needed.
Nursing’s Role in the Milk Dispensaries
In June 1908, the New York Milk Committee of the Association for Improving the Condition of the Poor opened a new kind of milk station that not only gave out pure milk, but also encouraged breastfeeding, provided medical exams, and dispensed information on infant hygiene along with milk (Meckel, 1990, p. 93). Public health nurses established new roles within these milk dispensaries as they proliferated in the United States (in 1900 there were 100 dispensaries and by 1915 over 700 were reported) (Goldwater, 1915). Nurses would take charge of handing out milk to families for one hour every day (Fiske, 1910). Some dispensaries required a physician’s order for the milk formula. Other times, nurses would weigh the child and prescribe the formula based on the child’s weight (Goler, 1904; Goldwater). Often the nurses were also responsible for pasteurization of the milk and the elaborate formula preparations. In addition, the nurses educated mothers by distributing “Little Books” written in different languages to help them be more independent in their child’s care. These books covered areas of infant care and feeding.
After the morning work in the Milk Dispensaries, the nurses made home visits to examine the infants and offered advice on feeding and care of the child. During home visits, nurses monitored the progress of the infant. One nurse described the home visit as “… learning the relation of the environment to the welfare of the family” (McClelland, 1913, p. 18). Nurses made use of the home environment to teach mothers about ways to modify their feeding behaviors to prevent illness. This included keeping the milk “cool, covered and clean” (McClelland, p. 20). Nurses instructed mothers on home cow’s milk infant formula preparation that involved various modifications of a mixture of cream, milk, lime-water, boiled water and sugar.3 While physicians continued to debate over what formula method was best, what sugar additive was best tolerated, if the addition of proprietary foods was necessary or desired, and if certified or pasteurized milk was best (Haehnlen, 1919; Roby, 1901), nurses had the unique opportunity to monitor infants on a regular basis and see for themselves which preparation was working.
Visiting and public health nurses encountered daily challenges in their work to mitigate the infant mortality problem. One factor was the nurse’s ability to look past common stereotypes and prejudices, of the time, in order to address the issues that families were facing. Early 20th Century social reform was centered on the belief that people should be educated to be morally and hygienically more like the dominant white, middle class, as illness was believed to be due to poverty and ignorance (Howard, 1912; Van Igen, 1912). Mothers, whose behaviors fell outside the narrow, middle-class white description of motherhood, were considered by the dominant culture to be unfit (Ladd-Taylor and Umansky, 1998). Ideologically, early 20th century health reformers believed they could teach mothers how to be more “American” and their babies would not die. In 1911, Gallagher described the unique perspective the public health nurse gained through their intimate encounters with families:
Deaths … are frequent among Italian babies living in unsanitary houses, made so by the vile construction of the buildings rather than the poor housekeeping of the mothers. These little tenements are surprisingly clean, considering the large families and numerous boarders, [which is] often the only source of income during the winter months when the unskilled laborer is out of work. … Often the mother has to go to work in the factory to eke out the income, and when this happens the baby always suffers (p. 549).
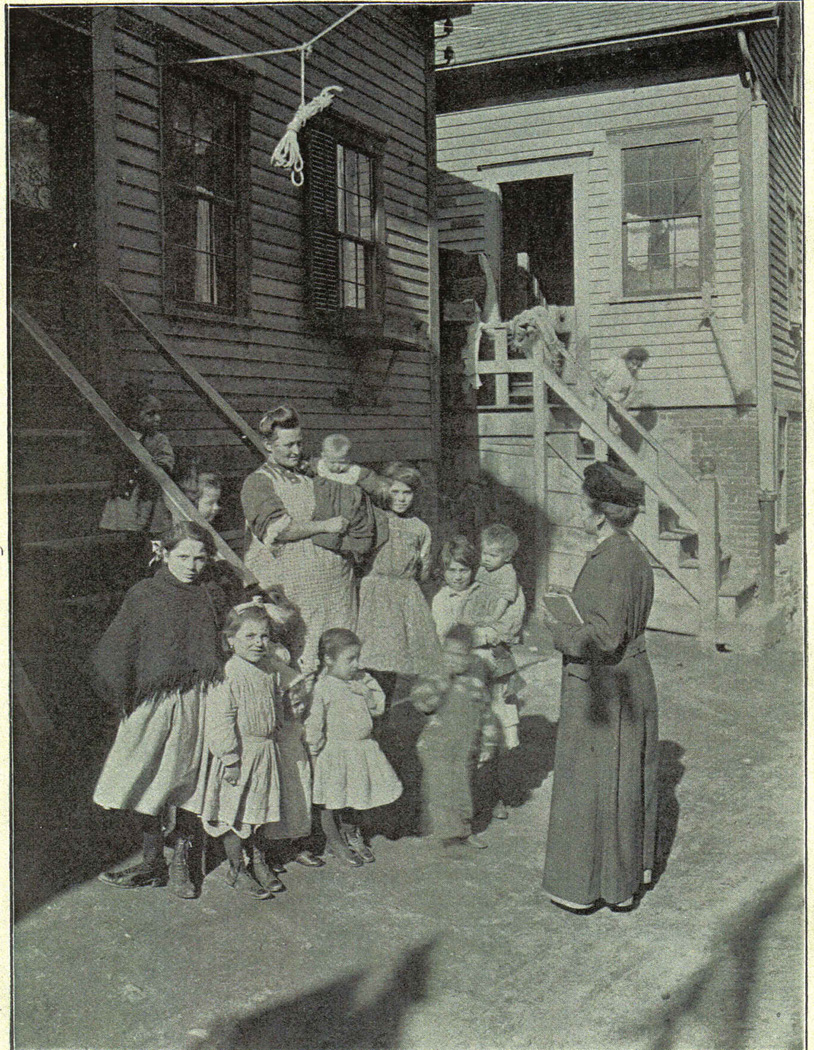
Example from the Providence District Nurses Association
The Providence District Nurses Association (PDNA) provides an excellent example of the creative and adaptive work that public health nurses did to meet the diverse needs of a city’s rapidly expanding population (see Figure 1). In the early 20th century, Providence, Rhode Island was known as the nation’s most industrialized city (From Town to City, n.d.). Employment opportunities in Providence’s many factories attracted both native-born citizens from local farms and newly arrived immigrants (Immigrants of German, Irish, French Canadian, Swedish, Portuguese and Italian heritage moved to Providence increasing the population from 54,595 in 1865 to 175,597 by 1900). As was seen in other major US cities, Providence had difficulties providing adequate housing and sanitation to meet the needs of its rapidly growing population. The formation of the PDNA, in 1900, was in direct response to meet the health needs of the City’s most vulnerable.
Figure 1.
A number of factors contributed to the PDNA success. In particular was the PDNA’s Board of Trustees early recognition of the need for a well trained and adept leader. In 1905, the PDNA hired Mary Sewell Gardner as its first superintendent of nurses. The well-educated leader came from a wealthy family from Newton, Massachusetts. At the age of thirty, she attended the Newport Hospital School of Nursing and was hired immediately after graduation as director of the PDNA (Gardner, 1906). Gardner later went on to become a leader in public health nursing and instrumental in the development of the National Organization of Public Health Nurses.4 Another important factor in the PDNA’s success was the collaborative working relationship between Gardner and the superintendent of the Providence Health Department, Charles V. Chapin, MD. Chapin, a leader in public health medicine, accepted the germ theory of disease before it was widely adopted by others in the medical community (Winslow, 1934). With this background, Chapin encouraged the PDNA to use progressive measures in their work with families (Gardner, 1925).
“Childern’s Special Nurse”
Mary Gardner was well aware of the health concerns of the poor. Early on, she advocated for a “summer children’s special nurse” to care for the infants with summer diarrhea. In 1906, Gardner acknowledged the importance of this nurse to “… lower the rate of infant mortality, prevent contagion and abnormalities and contribute much towards the strong, healthy lives of the future generation” (para 4). By 1907, the children’s nurse began to work with the “Pure Milk Stations” (Gardner, 1907). However, soon the nurse developed concerns about the families’ ability to properly modify and store the milk in the home. Gardner (1908, Annual Report) was concerned about the lack of sufficient education given to mothers in the milk stations and also that mothers were “very irregular about sending for the milk” (p. 25).
Addressing these concerns led to a number of initiatives. To meet the needs of an increasing number of poor families, Gardner appealed to The Committee on Infant Mortality of the Providence Medical Association to fund another children’s special nurse position at the PDNA and to provide clean milk to families who could not afford it (Gardner, 1908, Annual Report). Meanwhile, Superintendent Chapin made a list of milkmen whose “prepared” milk could be trusted. He also developed a pamphlet of simple milk formula modification procedures, printing it in various languages so that immigrant mothers could understand the directions.
Nurses made every attempt to teach mothers how to care for their babies with equipment they would have in their own homes. However, nurses had their doubts about being able to teach milk modification to mothers “who would have no particular desire to learn” (Gardner, p. 25). As Gardner noted:
All visiting nurses, however, know the hopelessness of entering a house, ready primed to teach milk modification and to preach fresh air and cleanliness when they find a dirty, stuffy house, an impossible back yard, and a mother who certainly may be taught, but with whom the process will undoubtedly be a prolonged one (Gardner, 1908, Baby Day Camp, p. 128).
The PDNA nurses recognized the challenges mothers faced in learning complex milk modification in the home environment. These concerns prompted the PDNA to find creative solutions to meet the special needs of the immigrant population.
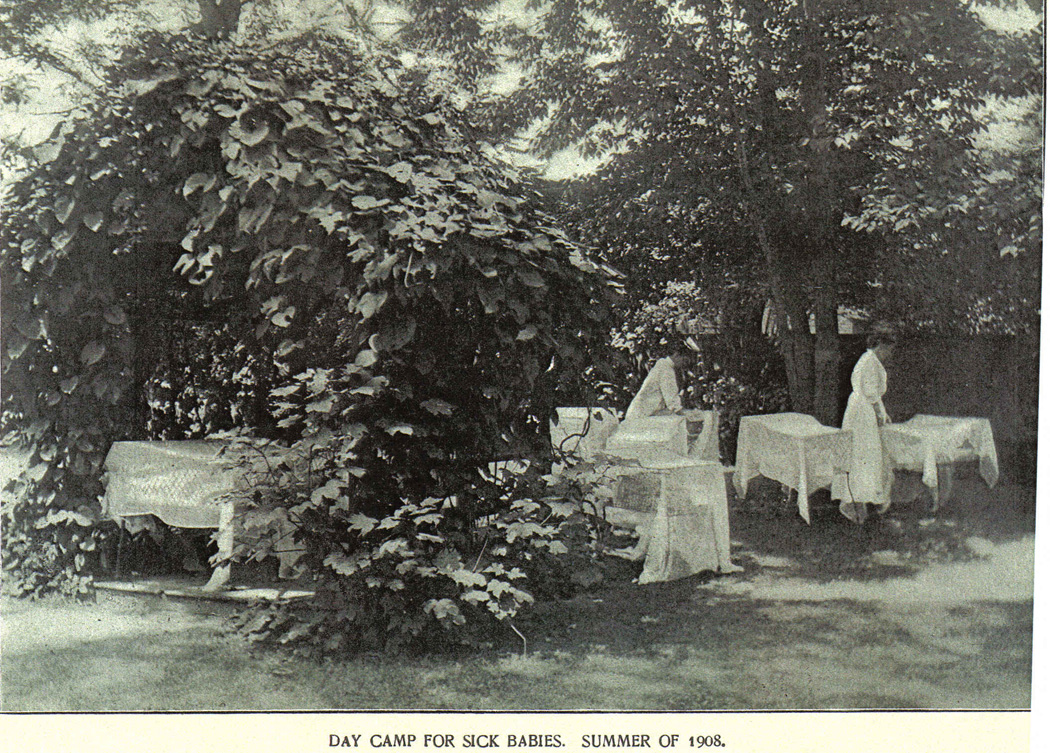
“Baby Day Camp”
The PDNA quickly found a creative solution and in the summer of 1908 they opened a Baby Day Camp (see Figure 2). There nurses cared for infants in a shaded area of the home of a wealthy family, who donated the use of their home for the summer. The Lying-In Hospital in Providence donated infant beds, bottle racks, and milk sugar, while the Superintendent of Public Health Chapin donated “two gross of bottles with corks and an ice chest” (Gardner, 1908, p. 27). Mothers brought babies at half past eight, every day including Sundays, with a set of clothes and a supply of diapers (Gardner, p. 129). Each morning, nurses modified the infant’s milk following the doctor’s orders, and each evening the mother took the bottles needed for the night. Nurse’s boiled the infants’ bottles, nipples, and night shirts each day. The very sick babies were kept overnight for nursing care. Mothers and family would visit throughout the day and once the infant was recovered, room was made for another sick infant. The first year the camp serviced fifty-three infants.
Figure 2.
The Baby Day Camp was found to be such a great success that the following year a second camp was opened in the Italian section of Federal Hill (Gardner, 1909). Actually, nurses noted that sick infants made greater progress and mothers seemed more cooperative with nursing care given at the camps than that provided in the home. In 1910, eighty-six babies were serviced by the Baby Day Camps during the summer months, two doctors were in “constant attendance,” and there were six children’s special nurses. Gardner (1910) noted, with the presence of the physicians, nurses were able to spend more “instructive” time with mothers resulting in “increased confidence of the mothers” in the nurses (p. 27).
Meeting their Needs
The PDNA success in reducing infant mortality was in part due to the nurses’ ability to create and adapt programs to meet the changing needs of the population. The PDNA was willing to work in cooperation with other agencies in the community to achieve its purpose. In 1911 when the Rhode Island Congress of Mothers and the Congress of Mothers for the Italians funded a babies’ consultation (or child health conference)5 in the “Italian section of town,” the PDNA nurses helped to staff the clinic. The babies’ consultations had such success in attendance that the following year, the agencies funded two consultations with plans for a third. PDNA nurses also made home visits which were an integral part of the consultations. The Baby Day Camps were closed in 1912 because of the success of the babies’ consultations and that Rhode Island hospital opened a new “babies ward” to care for sick infants (Gardner, 1912). Gardner, forever a public health nurse supporter, commented on the proposal for a large children’s hospital in Providence by stating that the goal of the community should be a low number of sick babies.
The tireless effort of the children’s nurses was rewarded when Dr. Chapin announced that the infant mortality rate in Providence dropped to 102 per thousand in 1917 as compared to 142 per thousand in 1907 (Gardner, 1919), attributing much of this success to the PDNAs’ work. Because of improvements in care and a decrease in the number of significantly ill infants, the role of the visiting children’s nurse remained viable. A year later, Gardner commented that the twelve children’s nurses working at the PDNA at the time could not begin to meet the needs of the city, “…for the mothers of Providence have apparently found in a children’s nurse a thing to their liking and they are calling upon her as never before” (1920, p. 17).
Discussion
It took many years of persistence on the part of public health nurses, doctors and city officials to identify and mitigate the factors contributing to the high rate of the infant mortality in Providence during the early 1900s. In this paper, a combination of issues was identified as contributing to infant mortality crises. These included: the environmental conditions of overcrowding due to high rates of immigration; inadequate public health regulations of milk; poverty; artificial feeding of infants; and mother’s lack of knowledge and resources to insure the best health for their infants. After decades of public health efforts and reforms, what public health nurses did to reverse the infant mortality rates was a combination of initiatives including: (a) modifying the home environment to improve the living conditions of the poor (immigrants), (b) implementing social programs to provide clean milk and food for families who could not afford it and, (c) educating mothers how to best feed and care for their children.
This historical account lends insight into child health issues facing the nation today. These insights can guide nurses who work with families facing the socio-economic barriers that put their children at increased risks for poor health outcomes. Finding creative solutions to current health issues using examples from the past may be particularly important as nurses look to address the issue of childhood obesity, as there is limited evidence for effective prevention measures (Oude-Luttikhuis et al., 2009; Summerbell et al., 2009). Michelle Obama’s timely announcement, on May 11, 2010, of the White House Task Force on Childhood Obesity’s Action Plan (Let’s Move), is further incentive for nursing to make childhood obesity a priority research and practice area.
Similarities exist between the infant mortality problem of the early 20th century and childhood obesity in terms of the magnitude of the problem, the complex nature of factors contributing to the issue, the factors of health disparities and disproportional prevalence of the problem among immigrant and non-white populations. With the development of new knowledge concerning the safety of unpasteurized milk a century ago, important policy changes were made in order to provide clean, safe milk to children. It behooves child health advocates and legislators to implement policy changes today that might positively impact on the health of children by preventing obesity.
Similar to infant mortality a century ago, higher rates of obesity in children have been associated with poverty, poor living conditions, lack of education, lack of governmental policies, and a lack of evidence supporting interventions. Singh, Kogan, Van Dyck, and Siahpush (2008) identified children who were significantly more at risk for obesity as being “… Black and Hispanic ethnicity, non-metropolitan residence, lower household education and higher poverty levels, low neighborhood social capital, and increased levels of television viewing and physical inactivity” (p. 682). Higher obesity rates exist in children from non-Hispanic Black and Mexican-American heritage than non-Hispanic White children, regardless of socio-economic status (Kumanyika & Grier, 2006). This means that factors in the child’s environment other than economic are affecting his/her risk for obesity. According to Kumanyika and Grier: “Effectively addressing ethnic and socioeconomic disparities in childhood obesity requires understanding which causes of obesity might be especially prevalent or intensified in ethnic minority and low-income populations…” (p. 191). Nurses must continue to be effective and dynamic agents for research, intervention and advocacy for children who are most at risk for obesity and this encourages nurses to look at the past for answers to today’s problems.
Based on the results of this historical research, four areas of interest for nursing research and practice concerning childhood obesity are suggested: environmental, social-economic, education, and policy. The following are important factors to consider for nurses interested in pursuing these areas. One factor is for nursing research and interventions to be immersed in children’s and families’ daily lives-based in the home, day care, schools, churches and other community agencies where children and families interact. Current suggestions to improve child obesity outcomes propose that interventions “… should be implemented across the multiple contexts that can influence children’s eating, activity and weight” (Birch & Ventura, 2009, p. S75). Nurses are in an ideal position to intimately observe health related behaviors, environmental and socio-economic factors which may be contributing to a child’s risk for obesity, such as diet, activity level, accessibility of safe areas for outdoor play and the availability of healthy food choices. Historically, nurses have demonstrated that they have the training and opportunity to develop trusted relationships with families that will contribute to the success of interventions to promote health. Historically, they have also had an intimate understanding of the cultural, environmental and socio-economic influences that put children at risk for disease. As was true in the past, today nurses are advised to take an unbiased and open minded approach to accurately assess the important factors in the child’s environment.
Perhaps even more today than a century ago, nurses can be effective in improving the health of children living in the United States by actively participating in policy change. An essential element of any nursing intervention for childhood obesity is advocating for changes in policies that support families’ attempts to improve health behaviors. In addition to advocating for legislation such as the Child Nutrition Reauthorization Act which funds programs such as WIC (Nutrition Program for Women, Infants, and Children), the National School Lunch Program, the School Breakfast Program (NAPNAP, 2010); nurses can become involved in policy changes at a broader level. For example, legislation advocating for creative solutions, such as those programs suggested by journalist Michael Pollen (2007), that supports competitive prices for healthy foods, farm to school initiatives to feed school children local and fresh products, and setting food prices according to fair market pricing and not by subsidies. Another important policy area includes the support that government food assistance programs may have in providing healthier food options in community food markets (Andreyeva, Middleton, Long, Luedicke, & Schwartz, 2011). Programs, that collaborate with community resources and identify imaginative solutions, worked a century ago and might be an answer for child health challenges today.
Conclusion
PHNs were dedicated to the cause of reducing infant mortality by teaching mothers the way to care and feed their children. They worked in families’ homes, in milk stations, and other creative settings, to best meet the needs of the families they were caring for. PHNs demonstrated patience and adaptation in working with families from many different ethnic backgrounds. They functioned independently, often making important decisions in regards to patient’s health. It is because of their ingenuity, courage, intelligence and flexibility that they contributed so greatly to the reduction of infant mortality in the late 18th and early 19th century. Nurses made a significant impact on infant mortality a century ago, and today we can learn from their example to do the same for child health issues such as childhood obesity. Nurses and nurse practitioners, particularly, are an integral part of this fight against obesity in targeting at risk children from disadvantaged backgrounds who might not otherwise receive optimal care. As historian Arlene Keeling (2007) said “… for over a century nurses have been providing safe and effective care to impoverished Americans in both cities and towns a cross the country, providing access to care for those to whom it would otherwise be denied” (p. 156).
Acknowledgments
This research was supported by a National Institute of Nursing Research Award, National Research Service Award No. 1 F31 NR010664-01
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The basic formula Meig’s recommended included diluting the cow’s milk with lime-water to reduce the amount of casein, increase the amount of water and make the milk more alkaline which was more like human milk. In addition, he recommended adding extra cream and milk sugar to increase the fat and sugar content of the formula (Apple, 1987).
By 1921 over 90 percent of American cities with populations over 100,000 had the bulk of their milk supplies pasteurized (Meckel, 1990).
Lime-water was used to reduce the amount of casein, increase the amount of water and make the milk more alkaline which was more like human milk (Apple, 1987).
Gardner was instrumental in the development of the National Organization of Public Health Nursing in 1912 and she became the second President of the organization in 1913. Mary Gardner was an avid writer on public health nursing throughout her career (Gardner, 1919). Gardner was the director of the PDNS from 1905–1931. During the First World War, she was asked by the American Red Cross to head its Bureau of Public Health Nursing. In 1918 she received an honorary degree from Brown University in recognition of her work (Ferguson, n.d.).
With the founding of the Children’s Bureau in 1912, children health conferences were developed at the milk dispensaries (Lathrop, 1918–1919). At the conference, the child would be examined by a physician and the milk formula adjusted for their weight. The nurses attended the conferences assisting the physician and often providing classes for the mothers. Nurses reported favorable results from their teachings at the conferences: “Illustrative material in the form of charts and posters are provided at every clinic for demonstrations on hygiene or food preparation.… Separated from the home atmosphere and surrounded by the means for different stimuli, the mother is able to see her problem in a new light” (Edwards, 1926, p. 168).
Contributor Information
Mary E. Thompson, University of Virginia School of Nursing, Claude Moore Nursing Education Building, Rm3004, 225 Jeanette Lancaster Way, Charlottesville, VA 22903, Phone: (434) 825-9744, Met8f@virignia.edu.
Arlene A. Keeling, University of Virginia School of Nursing, Claude Moore Nursing Education Building, Rm2111, 225 Jeanette Lancaster Way, Charlottesville, VA 22903, Phone: (434) 924-5906, awk2z@Virginia.EDU.
References
- Andreyeva T, Middleton AE, Long MW, Luedicke J, Schwartz MB. Food retailer practices, attitudes and beliefs about the supply of healthy foods. Public Health Nutrition. 2011 Jan;:1–8. doi: 10.1017/S1368980011000061. [DOI] [PubMed] [Google Scholar]
- Apple RD. Mothers and medicine: A social history of infant feeding, 1890–1950. Madison, Wisconsin: University of Wisconsin Press; 1987. [Google Scholar]
- Birch LL, Ventura AK. Preventing childhood obesity: What works? International Journal of Obesity. 2009;33:S74–S81. doi: 10.1038/ijo.2009.22. [DOI] [PubMed] [Google Scholar]
- Braveman P. A health disparities perspective on obesity research. Preventing Chronic Disease, Public Health Research, Practice and Policy. 2009;6(3):1–7. Retrieved from http://www.cdc.gov/pcd/issues/2009/jul/09_0012.htm. [PMC free article] [PubMed] [Google Scholar]
- Brodie B. Baby’s milk: A source of trust between mothers and nurse. Public Health Nursing. 1991;8(3):161–165. doi: 10.1111/j.1525-1446.1991.tb00749.x. [DOI] [PubMed] [Google Scholar]
- Buhler-Wilkerson K. No place like home: A history of nursing and home care in the United States. Baltimore, MD: The Johns Hopkins University Press; 2001. [PubMed] [Google Scholar]
- Connolly C. Saving babies: Child-saving and infant nutrition. Pediatric Nursing. 2005;31(4):309–311. [PubMed] [Google Scholar]
- Connolly CA, Gibson ME. The “White Plague” and Color: Children, Race, and Tuberculosis in Virginia 1900–1935. Journal of Pediatric Nursing. doi: 10.1016/j.pedn.2010.01.011. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards BB. A nutrition program as part of a public health nursing service. The Public Health Nurse. 1926;18:168–170. [Google Scholar]
- Ferguson CC. A Century of Caring: VNA of Rhode Island 1900–2000. Rhode Island: RE Smith Printing Co; (n.d.) [Google Scholar]
- Fisk A. Milk stations. The Trained Nurse and Hospital Review. 1910;45:220–225. [Google Scholar]
- Flaskerud JH, Lesser J, Dixon E, Anderson N, Conde F, Kim S, Verzemnieks I. Health disparities among vulnerable populations: Evolution of knowledge over five decades in nursing research publications. Nursing Research. 2002;51(2):74–85. doi: 10.1097/00006199-200203000-00003. [DOI] [PubMed] [Google Scholar]
- From Town to City: 1790–1832. History and Facts: America’s Renaissance City. (n.d.). Retrieved from http://www.providenceri.com/history/centuries1.html.
- Gallagher MA. An Italian milk station. American Journal of Nursing. 1911;11:548–550. [Google Scholar]
- Gardner MS. Baby day camp of the Providence District Nursing Association. American Journal of Nursing. 1908;9(2):128–131. [Google Scholar]
- Gardner MS. Providence, RI: Rhode Island Historical Society; 1906–1913. Annual Reports of the Providence District Nursing Association, MSS 1068, Box 1, Mary Gardner’s Papers Folder, Private collection of the Rhode Island Visiting Nurses Association. [Google Scholar]
- Gardner MS. Public health nursing. New York: The MacMillan Co; 1919. [Google Scholar]
- Gardner MS. Providence, RI: Rhode Island Historical Society; 1925. History of Twenty-Five Years of Work. MSS 1068, Box 31, History Folder, Private collection of the Rhode Island Visiting Nurses Association. [Google Scholar]
- Gardner MS. Public health nursing 2nd Ed. New York: The MacMillan Co; 1927. [Google Scholar]
- Goldwater SS. Dispensaries: A growing factor in curative and preventative Medicine. The Boston Medical and Surgical Journal. 1915;172(17):613–617. [Google Scholar]
- Goler G. Nurse’s work in milk stations. American Journal of Nursing. 1904;4(6):417–422. [Google Scholar]
- Haehnlen A. The feeding of infants and young children. American Journal of Nursing. 1919;19(10):748–751. [Google Scholar]
- Howard AE. The importance of milk stations in reducing city infant mortality. Boston Medical and Surgical Journal. 1912 May;166(21):773–775. [Google Scholar]
- Ingen PV. The education of mothers and the saving of babies. Proceedings of the Academy of Political Science. 1912 Jul;2(4):669–672. [Google Scholar]
- Keeling AW. Nursing and the privilege of prescription, 1893–2000. Columbus: Ohio State University Press; 2007. [Google Scholar]
- Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. The Future of Children. 2006;16(1):187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- Ladd-Taylor M, Umansky L, editors. Bad Mothers: The Politics of Blame in Twentieth-Century America. New York: New York University Press; 1998. pp. 1–28. [Google Scholar]
- Lathrop JC. Children’s Health Centers. U.S. Department of Labor: Children’s Bureau, Children’s Year Leaflet No.3, Bureau Publication No 45: 3–7. 1918–1919 Apr; Retrieved from http://www.mchlibrary.info/history/chbu/20696.PDF.
- Let’s Move. America’s Move to make a healthier generation of kids. (n.d.). Retrieved from http://www.letsmove.gov/taskforce_childhoodobesityrpt.html.
- Markel H. Caring for the foreign born: The health of immigrant children in the United States, 1890–1925. Archives of Pediatric and Adolescent Medicine. 1998;152:1020–1027. doi: 10.1001/archpedi.152.10.1020. [DOI] [PubMed] [Google Scholar]
- McClelland MB. Milk fund association nursing. The American Journal of Nursing. 1913;14:18–21. [Google Scholar]
- Meckel RA. Save the Babies: American Public Health Reform and the Prevention of Infant Mortality, 1850–1929. Baltimore, MD: The Johns Hopkins University Press; 1990. [Google Scholar]
- National Association of Pediatric Nurse Practitioner and Associates (NAPNAP) Virginia Chapter Quarterly Newsletter. 2010 Summer;:6.
- Oude-Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children (Review) 2009 doi: 10.1002/14651858.CD001872.pub2. (The Cochrane Collaboration Issue 1). Retrieved from http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001872/frame.html. [DOI] [PubMed]
- Pollan M. You are what you grow. New York Times. 2007 Apr 22; Retrieved from http://nytimes.com.
- Reutter L, Kushner KE. ‘Health equity through action on the social determinants of health’: Taking up the challenge in nursing. Nursing Inquiry. 2010;17(3):269–280. doi: 10.1111/j.1440-1800.2010.00500.x. [DOI] [PubMed] [Google Scholar]
- Reverby SM. Ordered to care: The dilemma of American nursing, 1850–1945. New York, NY: Cambridge University Press; 1988. 1988. [Google Scholar]
- Roby J. The feeding of children. American Journal of Nursing. 1901;1(9):644–645. [Google Scholar]
- The International Council of Nurses. Definition of Nursing. 2010 Apr 12; Retrieved from http://www.icn.ch/about-icn/icn-definition-of-nursing/
- Schwab MG. Mechanical milk: An essay on the social history of infant Formula. Childhood. 1996;3:479–497. [Google Scholar]
- Singh GK, Kogan MD, Van Dyck PC, Siahpush M. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: Analyzing independent and joint associations. Annals of Epidemiology. 2008;18:682–695. doi: 10.1016/j.annepidem.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Summerbell CD, Waters E, Edmunds L, Kelly SAM, Brown T, Campbell KJ. Interventions for preventing obesity in children. 2009 doi: 10.1002/14651858.CD001871.pub2. (The Cochrane Colalboration, Issue 1). Retrieved from http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001871/frame.html. [DOI] [PubMed]
- Tomes N. The Gospel of Germs: Men, Women, and the Microbe in American Life. Cambridge, MA: Harvard University Press; 1998. pp. 23–27.pp. 45–50. [PubMed] [Google Scholar]
- Winslow CEA. The public health nurse: How she helps to keep the baby well. U.S. Department of Labor: Children’s Bureau, Children’s Year Leaflet No.6, Bureau Publication No 47. 1918 Apr; Retrieved from http://www.mchlibrary.info/history/chbu/20414.PDF.
- Winslow CEA. A review of public health realities: Papers of Charles V. Chapin, M. D.,”. American Journal of Public Health and the Nations Health. 1934;24:989–990. [Google Scholar]
- Van Ingen P. The education of mothers and the saving of babies. Proceedings of the Academy of Political Science. 1912;2(4):195–198. [Google Scholar]