Abstract
Purpose:
To determine the factors responsible for patient delay and treatment delay in newly diagnosed sputum smear-positive pulmonary tuberculosis (TB) patients.
Methods:
Study subjects (N = 150) were randomly selected from municipal health centers in Mumbai, India. Duration of symptoms, treatment, and reason for delay were assessed using interviews and medical records. We defined patient delay as presentation to a health care provider (HCP) >20 days of the onset of TB-related symptoms and treatment delay as therapy initiated more than 14 days after the first consultation (for TB-related symptoms) with an HCP.
Results:
Of the 150 subjects, 29% had patient delays and 81% had treatment delays. In multivariable analysis, patient delay was significantly associated with the self-perception that initial symptoms were due to TB [odds ratio (OR) = 3.8, 95% confidence interval (CI) = 1.1–12.6] and perceived inability to pay for care (OR = 2.9, 95% CI = 1.2–7.1). Treatment delay was significantly associated with consulting a non-allopathic provider (OR = 12.3, 95% CI = 1.4–105) and consulting >3 providers (OR = 5.0, 95% CI = 1.4–17.4). Patient interval was half the treatment interval (median days: 15 vs. 31). Women were slightly more likely to experience patient and treatment delays than men. For two-thirds of the patients, another TB patient was a source of TB-related knowledge, while health education material (16%) and television (10%) played a smaller role.
Conclusion:
Treatment delay, primarily due to diagnosis delay, was a greater problem than patient delay. Expanding public–public and public–private partnerships and regular training sessions for HCPs might decrease treatment delay. Media coverage and cured TB patients as peer advocates may help to reinforce TB-related health education messages.
Keywords: Patient delay, pulmonary tuberculosis, India, treatment delay
INTRODUCTION
India has more new tuberculosis (TB) cases annually than any other country.[1] The annual incidence of sputum smear-positive cases is estimated to be 168/100,000 persons. Every day in India, >5000 develop TB and >1000 die from TB.[2] TB kills more women than all causes of maternal mortality combined.[3]
It is estimated that an untreated smear-positive patient may infect >10 contacts annually.[4] Delay in diagnosis and treatment leads to more advanced disease, more complications, higher mortality,[5–7] and has resulted in community outbreaks.[8] We undertook the present study to determine the factors responsible for “patient delay” and “treatment delay” in newly diagnosed sputum smear-positive pulmonary TB and to compare gender differences in these delays.
METHODS
Study site
Mumbai (India) with a population of approximately 12 million is divided into 23 wards (administrative areas). The Brihan-Mumbai Municipal Corporation (BMC) operates 243 health centers (BMCCs) within these wards, providing Directly Observed Treatment-Short course (DOTS) therapy in addition to primary health care; the TB clinics are also referred to as DOT centers. An estimated 50% of the population of Mumbai belonging to low to low-middle income groups seeks care from these health centers. In addition, at the time of the study (2002), BMC had involved 50 private physicians and/or non-governmental organizations (NGOs) [non-municipal centers (NMCs)] to implement the national TB program in Mumbai.
Study design and subject selection
We conducted a cross-sectional study in early 2002. Eligible subjects were ≥18 years of age; sputum smear-positive, newly diagnosed, with pulmonary TB alone, i.e. without any concomitant chronic lung disease such as asthma, bronchitis, emphysema, or lung cancer; had received anti-TB treatment for <6 months; and were non-pregnant.
We randomly selected 12 municipal wards and then randomly selected up to three DOT centers within that ward. This selection was made using the “DOTS Directory” (maintained by the BMC) that lists all DOT centers. Within each center, we randomly selected up to 15 patients using “treatment cards” that contained information on patient's demographic, diagnostic, and treatment history on the day of our visit. The final study size was 75 men and 75 women (1:1 ratio) selected from 29 BMCC/DOTS centers.
Of 150 subjects initially selected, 18 could not be contacted. Of the remaining 132 subjects, 126 (95%) agreed to participate in the study. We replaced all the 24 subjects with re-recruitment. In addition, subjects (totally 10) were interviewed from three randomly selected NMCs to examine the differences between BMCCs and NMCs; the three centers selected were run by NGOs.
Interview
One physician (AT) conducted all 150 interviews in person at the DOT centers using a pre-tested questionnaire in Marathi or Hindi language, as preferred by the subject. The questionnaire elicited information about seeking care and initiating treatment, socio-demographic characteristics, lifestyle and health care access factors, presenting symptoms, knowledge and perceptions about TB, and sources of information about TB. Patients were particularly asked about TB-related symptoms such as cough, hemoptysis, fever, loss of appetite and weight, chest pain, shortness of breath, and tiredness. In addition, they were asked about any other symptoms/signs they attributed to TB that were experienced before seeking treatment. In addition to physicians practicing modern medicine (allopath) or alternative medicine (non-allopaths), a health care provider (HCP) was defined as any person/facility from where the patient sought care for his symptoms/signs. Pharmacies/drug stores, acupressurist, acupuncturist, and traditional healers were also included as HCPs.
We also abstracted information from the medical records available at the health centers (especially treatment cards) and records carried by subjects. Treatment cards included information on patient's socio-demographic characteristics, dates, results of sputum microscopy, and radiological and other investigations. Medical records available with subjects included information on visits and treatment received in and out (other HCPs) of the health center. We used this data to supplement information obtained from patient interviews.
Time intervals and delays [Figure 1]
Figure 1.
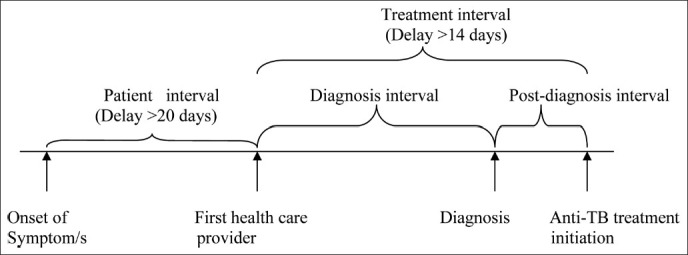
Patient and treatment (diagnosis and post-diagnosis) time intervals and operational definitions of corresponding delays (indicated in parenthesis)
There is no consensus on what might be called “delay” with regard to seeking care and initiating treatment for TB; some have suggested this period to be ≤1 month or <2 months.[9–11] We defined patient delay as presentation to an HCP >20 days of onset of TB-related symptoms (patient interval >20 days). Considering local health infrastructures, we defined treatment delay as therapy initiated more than 14 days after the first consultation (for TB-related symptoms) with an HCP (treatment interval >14 days).
Analysis
Delays were classified both as continuous and dichotomous variables. We compared median time-intervals between men and women using Wilcoxon rank-sum test. For the dichotomous outcome, we compared the presence/absence of delay and the presence/absence of a risk factor using crude prevalence odds ratio (POR) with its corresponding 95% confidence interval (CI). Proportions were compared using Fisher's exact test. Unconditional multiple logistic regression was used to calculate adjusted PORs for risk factors. A factor was included in the logistic model if it was statistically significant (P < 0.05, two-tailed) or had moderate association (crude POR was ≤0.5 or ≥2.0) with outcome. Power calculations, based on a study conducted in Mumbai (India),[12] indicated that a study of 75 men and 75 women would have 82% power to detect a 20% difference in patient delay and 76% power to detect 20% difference in treatment delay between men and women. Data analysis was performed using SAS statistical software, version 8.0 (SAS, Inc., Cary, NC, USA).
RESULTS
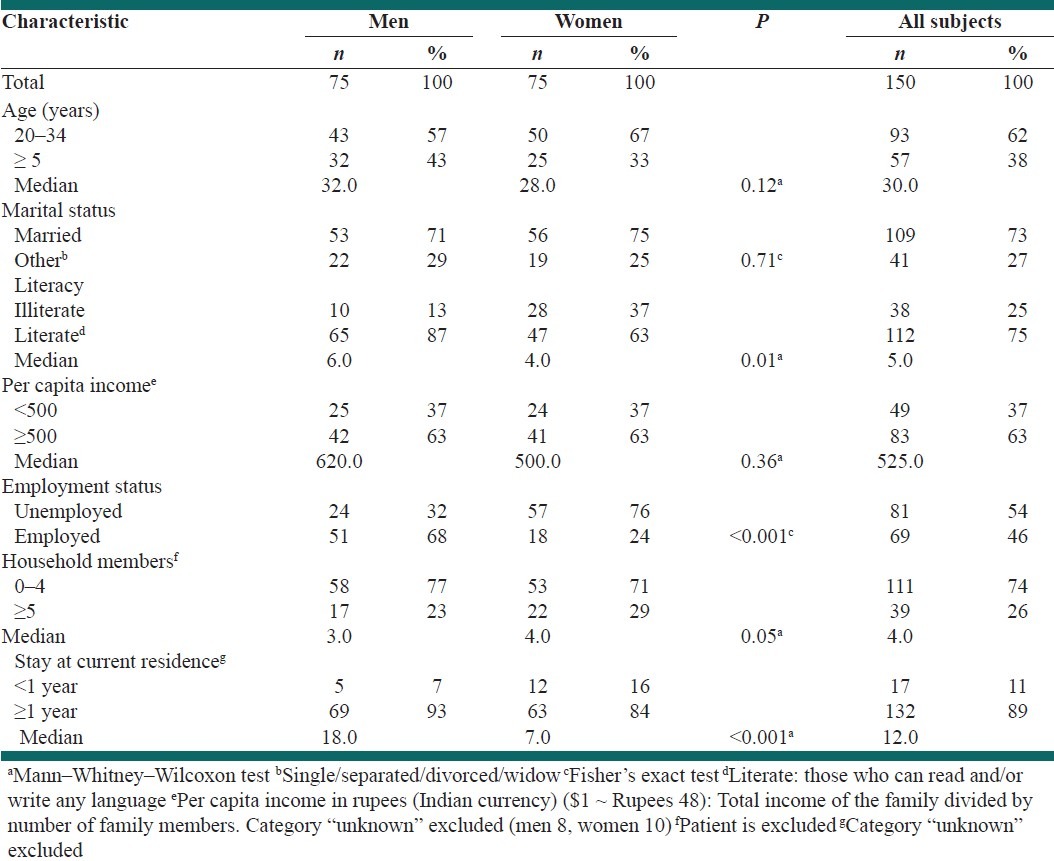
The study subjects had a median age of 30 years [Table 1]. They were of low socioeconomic status with a median per capita monthly income of 525 (≈US $11). Men were likely to be more literate (87% vs. 63%), to be employed (68% vs. 24%), and to be resident in the immediate area (18 years vs. 7 years) than women. Differences in age, marital status, per capita income, and number of household members between men and women were small. Families of 97% subjects, relatives of 56% subjects, and neighbors of 48% subjects were aware of the patient's TB status, indicating perceived social stigma by the patient.
Table 1.
Selected subject characteristics by gender
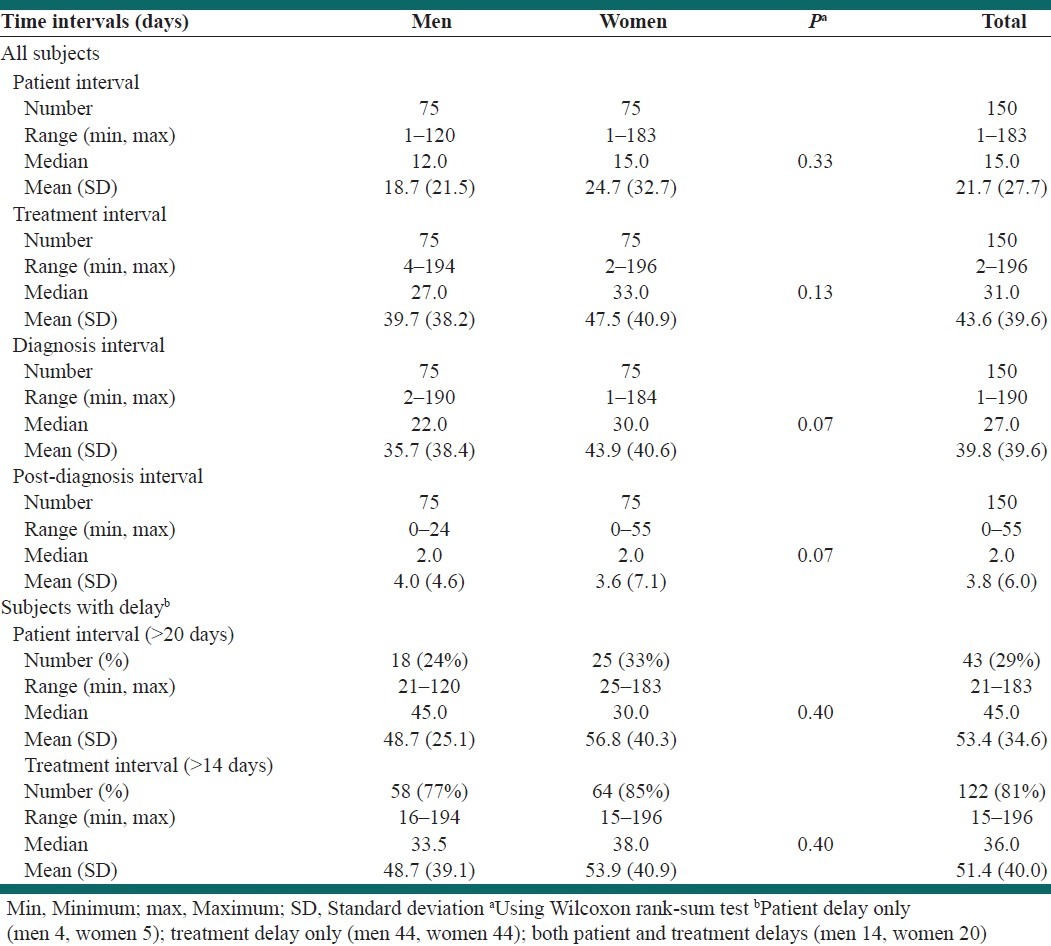
Time intervals and delays
Patient interval was half the treatment interval (median days: 15 vs. 31) [Table 2]. The long treatment interval was primarily due to longer diagnosis interval than post-diagnosis interval (median days: 27 vs. 2). Women had slightly longer patient and treatment intervals than men. Of the 150 subjects, 43 (29%) had patient delay and 122 (81%) had treatment delay [Table 2]. As compared to men, women were more likely to experience both patient delay (POR = 1.6, 95% CI = 0.8–3.2; P = 0.28) and treatment delay (POR = 1.7, 95% CI = 0.7–3.9; P = 0.30); however, the differences were not statistically significant.
Table 2.
Patient and treatment time intervals for all subjects and for those with delay according to gender
Risk factors for patient delay
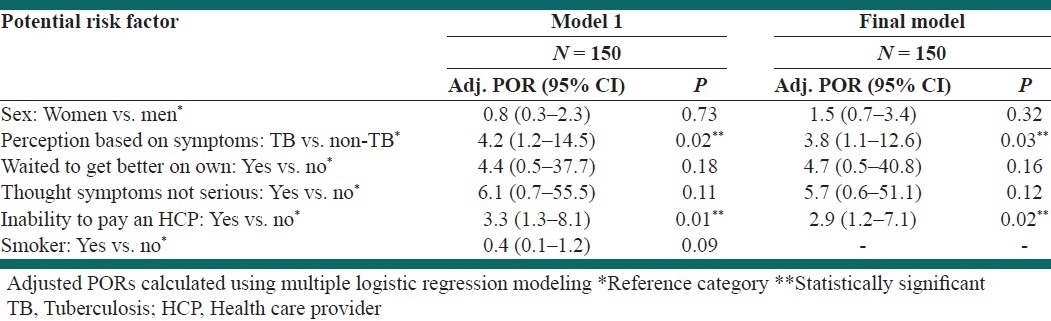
Thirteen risk factors were moderately associated with patient delay (crude or gender stratified POR: ≤0.5 or ≥2.0) [Table 3]. Of these risk factors, those who waited to get better on their own, those who thought initial symptoms were not serious, and those who reported inability to pay an HCP were statistically significant.
Table 3.
Crude prevalence odds ratio (POR) and corresponding 95% confidence interval (CI) of potential risk factors for patient delay by gender
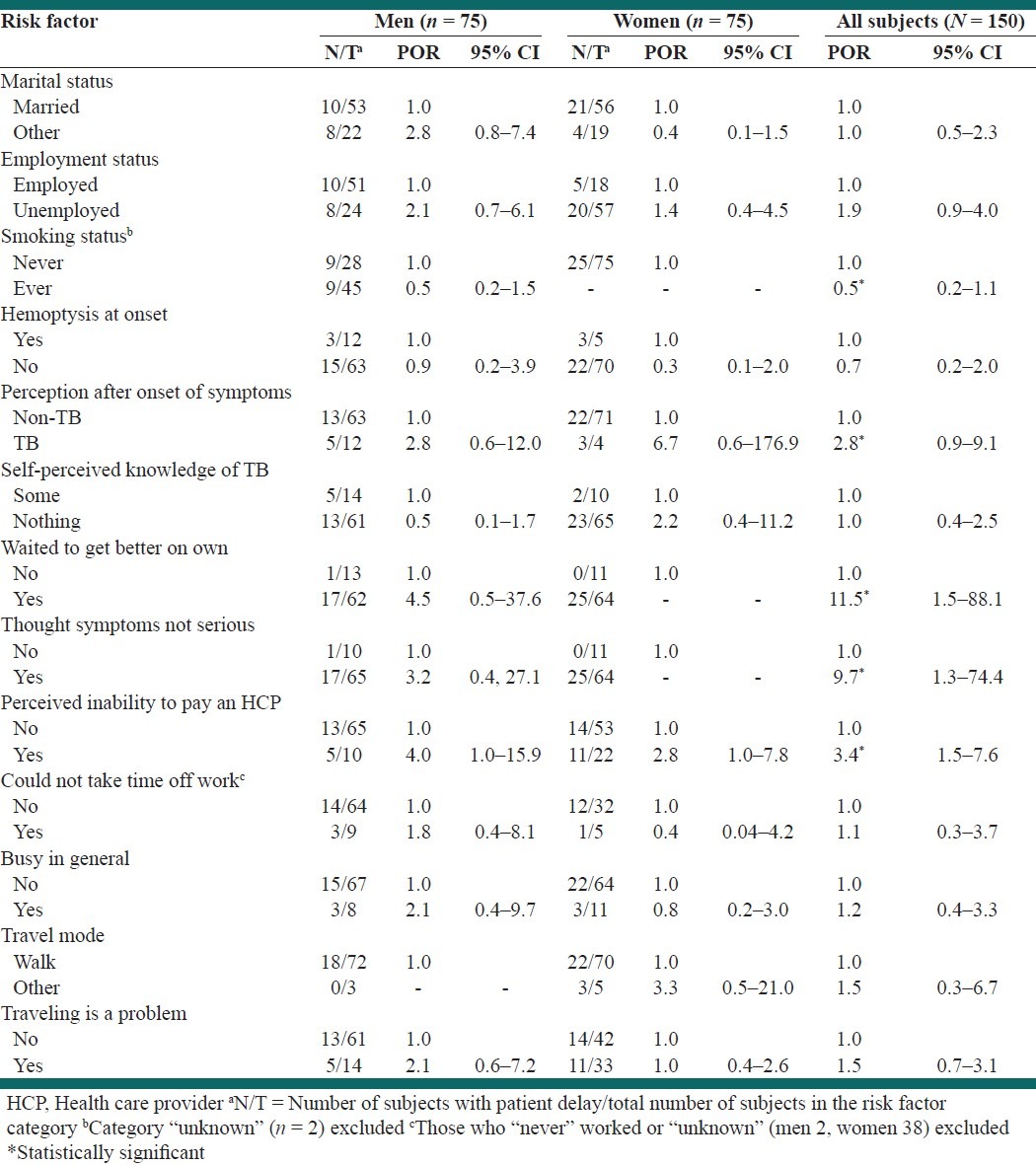
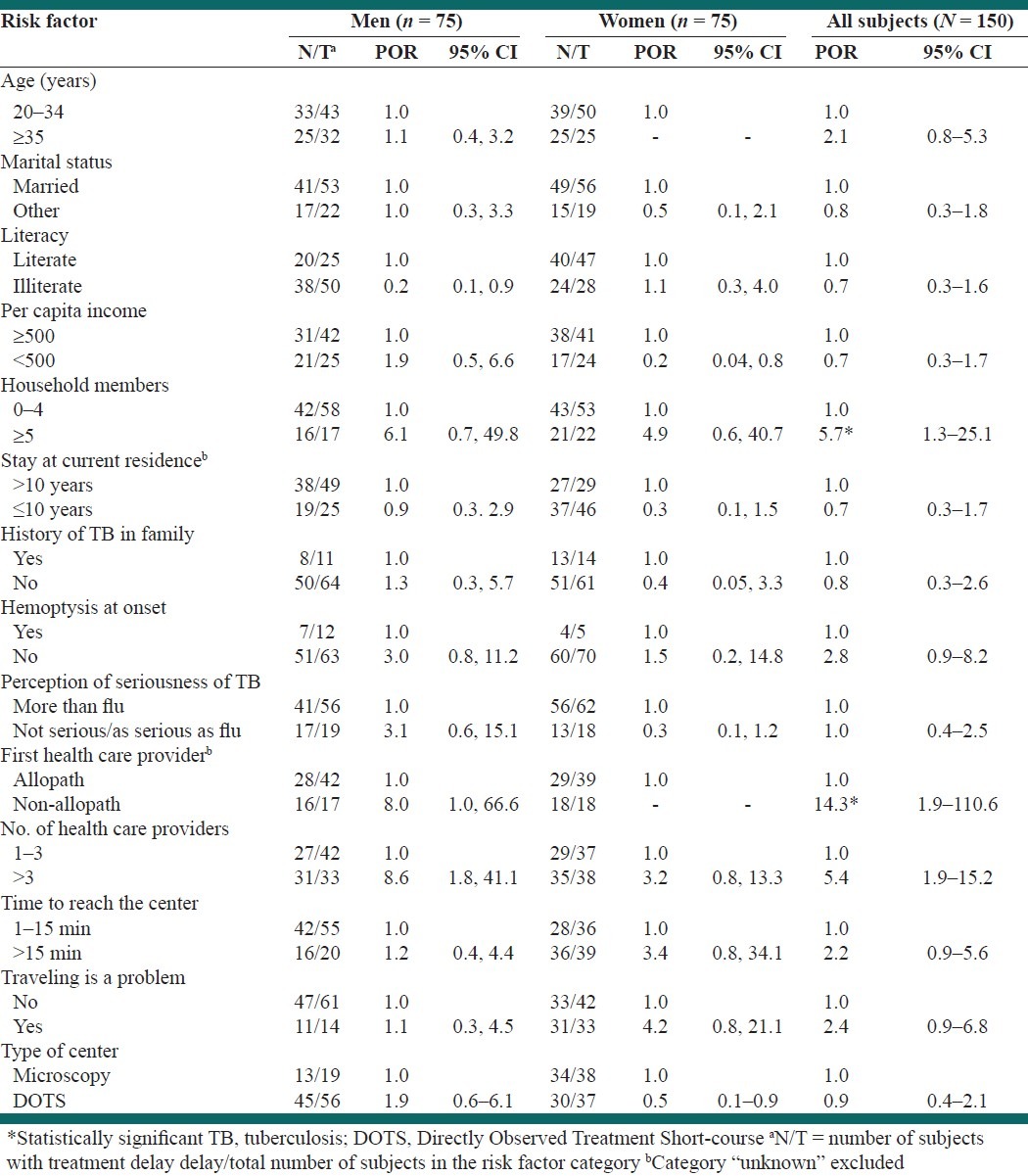
In multivariable analysis, perception of initial symptoms to be of TB (adjusted POR = 3.8, 95% CI = 1.1–12.6) and perceived inability to pay an HCP (adjusted POR = 2.9, 95% CI = 1.2–7.1) were significant [Table 4]. Gender differences were not significant for these risk factors. Patients whose neighbors were not aware of the patient's TB status, an indicator of social stigma, were almost equally likely to have delay as compared to those whose neighbors were aware (OR = 1.1, 95% CI = 0.5–2.4).
Table 4.
Adjusted prevalence odds ratio (POR) and 95% confidence interval (CI) for selected risk factors of patient delay
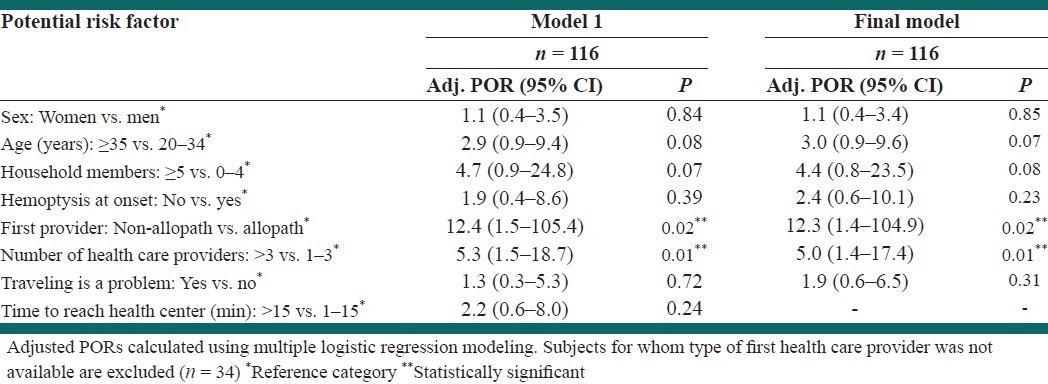
Risk factors for treatment delay
Fourteen risk factors were moderately associated with treatment delay [Table 5]. Of these, those with ≥5 household members, those who consulted a non-allopathic HCP on their first visit, and those who consulted >3 HCPs (prior to initiation of treatment) were significant.
Table 5.
Crude prevalence odds ratio (POR) and corresponding 95% confidence interval of potential risk factors for treatment delay by gender
In multivariable analysis, consulting a non-allopathic HCP on the first visit (adjusted POR = 12.3, 95% CI = 1.4–104.9) and consulting >3 HCPs (adjusted POR = 5.0, 95% CI = 1.4–17.4) remained significant [Table 6]. Gender differences were not significant.
Table 6.
Adjusted prevalence odds ratio (POR) and 95% confidence interval for selected risk factors of treatment delay
Other findings
Fever was the most common presenting symptom (85%) with cough >20 days in 23% and hemoptysis in 11% subjects. Of 116 subjects for whom the type of first HCP was known, 30% had consulted a non-allopathic HCP and the remaining (70%) had consulted an allopathic HCP (municipal/ government or private practitioner). Non-allopathic HCPs were less likely to suspect/diagnose TB than allopathic HCPs (POR = 0.2, 95% CI = 0.1– 0.4). In an analysis restricted to 27 subjects who presented with cough ≥3 weeks and for whom first HCP was known, 18 consulted a non-allopathic HCP on the first visit and 9 consulted an allopath. Non-allopathic HCPs provisionally diagnosed TB in 39% (7/18) while allopathic HCPs provisionally diagnosed TB in 78% (7/9) (P = 0.10). Similarly, in 17 subjects with hemoptysis at onset, non-allopathic HCPs were less likely diagnose TB as compared to allopathic HCPs (45% vs. 100%; P = 0.08). Of the 116 subjects, 65% consulted a private practitioner on the first visit. Those who consulted a government health facility were about equally likely to have patient delay (POR = 0.8, 95% CI = 0.3–1.9; P = 0.7), but were much less likely to have treatment delay (POR = 0.2, 95% CI = 0.1–0.6; P = 0.002) than those who consulted a private practitioner. Seventy percent of the subjects with perceived inability to pay an HCP consulted a private practitioner on the first visit.
Most (95%) of the subjects walked to the health center providing DOTS therapy [Table 3] and 61% subjects lived within a 15 min walking distance [Table 5]. About 31% subjects (women more than men) felt that traveling to the current health center was “problematic” (44% vs. 19%; P = 0.001).
When asked about the perceived level of TB-related knowledge (prior to onset of symptoms), 115 had “little” and 24 had “some” knowledge about TB, while the remaining 11 said they knew “nothing” about TB. Of the 139 subjects with “little/some” knowledge about TB, 66% had heard about TB from relatives/friends while 63% reported acquiring knowledge about TB from another TB patient. About 16% reported health education materials displayed in health care facilities/community as a source of knowledge. Media (television, 10%; radio, 2%) played a small role in educating patients about TB. More than two-thirds of subjects (men, 53/75; women, 63/75) knew that TB is propagated by cough. Most (70%) subjects thought that TB is more serious than the common cold/flu. Misconceptions about modes of transmission included sexual intercourse (53%), sharing blade/injection (66%), and using public toilets (43%). Thirteen percent of the subjects believed that evil eye/witchcraft causes TB.
Comparison between municipal and non-municipal health centers
No significant differences were found between BMCCs and NMCs with regard to age, demographics, employment, and household characteristics (data not shown). Median patient (BMCC = 15 days vs. NMC = 12.5 days; P = 0.41) and treatment (BMCC = 31 days vs. NMC = 24 days; P = 0.21) intervals were slightly shorter for the NMCs than BMCCs.
DISCUSSION
We found that 29% subjects had patient delay and 81% had treatment delay, slightly more in women than men. Significant risk factors for patient delay included perception of initial symptoms to be due to TB and perceived inability to pay an HCP. Significant risk factors for treatment delay included consulting non-allopathic HCP on the first visit and consulting >3 HCPs. Non-allopathic HCPs were less likely than allopathic HCPs to diagnose TB when present. About two-thirds of subjects acquired knowledge about TB from either relatives/friends or a TB patient; media and health education materials played only a small role.
Patient delay
In this study, the median time interval from the onset of symptoms to seeking care (15 days) is closer to lower bound of the range (10–119 days) reported in other studies.[12–17] We noted that 29% had patient delay based on a 3-week (>20 days) cut-off point. On the other hand, other studies report patient delay ranging from 20 to 81%[12,13,18–21] based on a 4-week/1-month cut-off point for patient interval. Using a 4-week cut-off point, we noted that 15% had patient delay, indicating that patient delay was less problematic in our study population as compared to others in the literature. This may be due to interplay of various factors such as easy availability and accessibility of health care facilities in Mumbai and higher (if still sub-optimal) community awareness about TB.
In our study, two factors were significantly associated with patient delay: perception of initial symptoms to be due to TB and perceived inability to pay an HCP. It might be expected that those who perceive the initial symptoms to be due to TB would seek care earlier to be diagnosed and treated at the earliest. However, fear of being diagnosed with TB itself can delay seeking care,[22] further compounded by fear of social stigmatization/ isolation.[23] In this study, patient's TB status was not known to his/her neighbors in >50% of subjects, indicating perceived social stigma by the patients in the community. However, social stigma was not associated with patient delay in this study in contrast to other studies.[21,24,25] Perceived inability to pay an HCP indirectly indicates preference for a private practitioner over a government health facility. When a patient consults a private practitioner, the direct out-of-pocket costs could include diagnostics, treatment, and consultation fees, which are free/ very minimal at a municipal/government health facility. In spite of this, paradoxically poverty can compel patients to seek care from private health sector than governmental clinics.[3] This could be related to hidden costs such as related to travel or longer distances.[26,27] In our study too, those subjects whose mode of travel to the DOTS center was other than walking and who reported that overall traveling was a problem were more likely to have patient delay; however, this association was not found to be significant. Other reasons, if any, for not consulting a governmental health care facility on first visit (e.g. dissatisfaction or distrust, crowding, long waiting time, and other) or preference for consulting a private practitioner were not explored in this study.
Initially consulting with a private practitioner is common in India.[17,24,28–33] In our study, 65% of subjects consulted a private practitioner on their first TB-related visit, of whom 32% had a patient delay. In addition, 70% of the subjects with perceived inability to pay an HCP consulted a private practitioner on the first visit. Probably those 70% could arrange money with extra efforts for private consultation, while the remaining 30% could not and had no “choice” but to consult a municipal/government facility. Nair et al.[31] in their study conducted in Mumbai observed that as the disease progressed, patients shifted from the private practitioner to municipal and NGO health services, the primary reason being cost of treatment. Economic constraints/poverty has been reported to be associated with patient delay in other studies too.[34,35]
Women were somewhat more likely to experience patient delay than men (33% vs. 24%; P = 0.28). Women had lower literacy, greater unemployment, lower median per capita income, and greater family size, as compared to men. Other studies also found delay occurring more in women than men,[13,27,34,36,37] though the magnitude of the differences found may have been due to chance alone, given our sample size.
Treatment delay
In our study, median treatment interval was 31 days. In other studies, median treatment interval varied from 15 to 60 days.[11,14,17,19,37] We found that 81% had treatment delay. Other studies have reported treatment delay from 18 to 62% subjects with 4 weeks/1 month cut-off point.[13,18,19,20] Using a 4-week criterion, 43% subjects in our study had treatment delay, suggesting the similarity of our findings with those elsewhere.
Our finding that consulting non-allopathic HCP on the first visit and consulting >3 HCPs were significantly associated with treatment delay is similar to the reports by others.[12,14,37] In our study, HCPs associated with government health facilities were allopaths, while private practitioners were a mixture of both allopaths and non-allopaths. Similar to other studies,[17,19,27,37] we also found that those who consulted a private practitioner on their first visit were significantly more likely to experience treatment delay than those who consulted a government health facility. Not all studies confirm this, as a previous study from Mumbai reported that TB management practices of non-allopaths did not differ significantly than that of allopaths.[12] Consulting multiple HCPs may reflect dissatisfaction with services,[31] failure to address the problem, or may be related to patient characteristics (e.g. not returning after initial consultation). We cannot distinguish these in our study.
As in other studies,[27,36,38] women were more likely to experience treatment delay than men; however, the difference was not significant. Other studies[13,34,37,39] have found significant gender differences. Several possible reasons have been suggested for observing treatment delay more in women than men. Low sputum positivity in women may be due to their inability to produce enough sputum,[40] social embarrassment about producing a sputum sample at the health center,[41] or family or social obligations limiting the time that they can spend.[3] In contrast, in a study conducted in southern part of India, it was found that men were more likely to experience treatment delay than women (32% vs. 23%).[17]
Lastly, though majority of the patients correctly knew about transmission of TB through cough, other misconceptions about transmission were prevalent too. Overall, majority of the patients reported relatives/friends and other TB patients being sources of knowledge, while media played a small role in educating patients about TB, which has been observed in other studies too.[22]
Strengths and limitations
Interviews were conducted by a single investigator to increase consistency and overall reliability. High participation rate (86%) and supplementation of interview with medical record reviews increased internal validity of the study. Due to inclusion of all municipal DOTS centers from Mumbai and random selection of the study centers and patients, we believe that our results may be applicable to the other patients attending municipal DOTS centers in Mumbai. Limitations of our study include possible recall bias, especially when medical records were unavailable to verify accuracy of information given by subjects, and lack of power to detect small differences between men and women with regard to time intervals/delays and some risk factors.
CONCLUSION
Thus, treatment delay, primarily due to diagnosis delay, was more of a problem than patient delay. Expanding public–public and public–private partnerships and conducting regular training sessions for both allopathic and non-allopathic HCPs, especially in the private sector, might be expected to decrease treatment delay. Media efforts may not be penetrating the community to reduce patient delays. Reinforcing TB-related health education messages with effective media coverage (e.g. involving movie stars) and using innovative methods of community education (e.g. training cured TB patients as peer advocates) might be beneficial.
ACKNOWLEDGMENTS
The study was supported in part by the John J. Sparkman Center for Global Health (University of Alabama at Birmingham, USA) and the Brihan-Mumbai Municipal Corporation (Mumbai, India). The authors are grateful to the staff of health centers of BMC who helped in contacting patients and scheduling interviews. We extend special thanks to the District Tuberculosis Officer of Mumbai, Dr. S. Mujumdar, for her active participation in the training associated with the study.
This study was submitted as a masters’ level project toward requirement for the MSPH degree in public health (epidemiology) at the University of Alabama at Birmingham. In addition, it was presented in part as an oral presentation at the 131st Annual Meeting of the American Public Health Association, San Francisco, CA, USA (2003) and in the seminar series in global health organized by the John J. Sparkman Center of the University of Alabama at Birmingham, Birmingham, AL, USA.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Global tuberculosis control: surveillance, planning, financing. WHO Report 2006. Geneva: World Health Organization; World Health Organization. WHO/ HTM/ TB/2006.362. [Google Scholar]
- 2.Behera D. Textbook of pulmonary medicine. 2nd ed. Vol. 1. New Delhi, India: Jaypee Brothers Medical Publishers Ltd; 2010. p. 477. [Google Scholar]
- 3.Somma D, Auer C, Abouihia A, Weiss MG. Gender in tuberculosis research. Department of Gender, Women and Health, World Health Organization. 2004 [Google Scholar]
- 4.Styblo K. Epidemiology of tuberculosis; selected papers. The Royal Netherlands Tuberculosis Association. 1991:53–4. [Google Scholar]
- 5.Enarson DA, Grzybowski S, Dorken E. Failure of diagnosis as a factor in tuberculosis mortality. CMAJ. 1978;118:1520–2. [PMC free article] [PubMed] [Google Scholar]
- 6.Bakhshi SS, Hawker J, Ali S. Tuberculosis mortality in notified cases from 1989-1995 in Birmingham. Public Health. 1989;112:165–8. doi: 10.1016/s0033-3506(98)00222-4. [DOI] [PubMed] [Google Scholar]
- 7.Pablos-Mendez A, Sterling TR, Frieden TR. The relationship between delayed or incomplete treatment and all-cause mortality in patients with tuberculosis. JAMA. 1996;276:1223–6. doi: 10.1001/jama.1996.03540150025026. [DOI] [PubMed] [Google Scholar]
- 8.Raffalli J, Sepkowitz KA, Armstrong D. Community based outbreaks of tuberculosis. Arch Intern Med. 1996;156:1053–560. [PubMed] [Google Scholar]
- 9.Aoki M, Mori T, Shimao T. Studies on factors influencing patient's, doctor's and total delay of tuberculosis case detection in Japan. Bull Int Union Tuberc Lung Dis. 1985;60:128–30. [Google Scholar]
- 10.Pirkis J, Speed BR, Young AP, Dunt DR, MacIntyre CR, Plant AJ. Time to initiation of anti-tuberculosis treatment. Tuber Lung Dis. 1996;77:401–6. doi: 10.1016/s0962-8479(96)90111-2. [DOI] [PubMed] [Google Scholar]
- 11.Wandwalo ER, Morkve O. Delay in tuberculosis case-finding and treatment in Mwanza, Tanzania. Int J Tuberc Lung Dis. 2000;4:133–8. [PubMed] [Google Scholar]
- 12.Uplekar M, Juvekar S, Morankar S. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis. 1998;2:324–9. [PubMed] [Google Scholar]
- 13.Lawn SD, Afful B, Acheampong JW. Pulmonary tuberculosis: diagnostic delay in Ghanian adults. Int J Tuberc Lung Dis. 1998;2:635–40. [PubMed] [Google Scholar]
- 14.Calder L, Gao W, Simmons G. Tuberculosis: Reasons for diagnostic delay in Auckland. N Z Med J. 2000;113:483–5. [PubMed] [Google Scholar]
- 15.Sasaki Y, Yamagashi F, Yagi T, Yamatani H, Kuroda F, Shoda H. A study of patient's and doctor's delay in patients with pulmonary tuberculosis discovered by visiting doctors with symptoms in particular on doctor's delay. Kekkaku. 2000;75:527–32. [PubMed] [Google Scholar]
- 16.Demissie M, Lindtjorn B, Berhane Y. Patient and health services delay in the diagnosis of pulmonary tuberculosis in Ethiopia. BMC Public Health. 2002;2:23. doi: 10.1186/1471-2458-2-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. Int J Tuberc Lung Dis. 2002;6:789–95. [PubMed] [Google Scholar]
- 18.Mori T, Shimao T, Jin BW, Kim SJ. Analysis of case finding process of tuberculosis in Korea. Tuberc Lung Dis. 1992;73:225–31. doi: 10.1016/0962-8479(92)90091-W. [DOI] [PubMed] [Google Scholar]
- 19.Steen TW, Mazonde GN. Pulmonary tuberculosis in Kweneng district, Botswana: delays in diagnosis in 212 smear-positive patients. Int J Tuberc Lung Dis. 1998;2:627–34. [PubMed] [Google Scholar]
- 20.Lonnroth K, Thuong LM, Linh PD, Diwan VK. Delay and discontinuity-a survey of TB patients’ search of a diagnosis in a diversified health care system. Int J Tuberc Lung Dis. 1999;3:992–1000. [PubMed] [Google Scholar]
- 21.Godfrey-Faussett P, Kaunda H, Kamanga J, van Beers S, van Cleeff M, Kumwenda-Phiri R, et al. Why do patients with a cough delay seeking care at Lusaka urban health centers? A health systems research approach. Int J Tuberc Lung Dis. 2002;6:796–805. [PubMed] [Google Scholar]
- 22.Agboatwalla M, Kazi GN, Shah SK, Tariq M. Gender perspectives on knowledge and practices regarding tuberculosis in urban and rural areas in Pakistan. East Mediterr Health J. 2003;9:732–40. [PubMed] [Google Scholar]
- 23.Long NH, Johanson E, Diwan VK, Winkvist A. Fear and social isolation as consequences of tuberculosis in Vietnam: a gender analysis. Health Policy. 2001;58:69–81. doi: 10.1016/s0168-8510(01)00143-9. [DOI] [PubMed] [Google Scholar]
- 24.Juvekar S, Uplekar MW, Morankar SN, Kasare M, Tilekar N, Bhatti B, et al. Behaviour profile of tuberculosis patients in private clinics. Indian J Tuberc. 1998;45:95–100. [Google Scholar]
- 25.Rajeswari R, Muniyandi M, Balsubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: a field report from South India. Soc Sci Med. 2005;60:1845–53. doi: 10.1016/j.socscimed.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 26.Johansson E, Long NH, Diwan VK, Winkvist A. Gender and tuberculosis control: perspectives on health seeking behaviour among men and women in Vietnam. Health Policy. 2000;52:33–51. doi: 10.1016/s0168-8510(00)00062-2. [DOI] [PubMed] [Google Scholar]
- 27.Yamasaki NM, Ozasa K, Yamada N. Gender differences in delays to diagnosis and health care seeking behavior in a rural area of Nepal. Int J Tuberc Lung Dis. 2001;5:24–31. [PubMed] [Google Scholar]
- 28.Uplekar MW, Rangan S. Private doctors and tuberculosis control in India. Tuberc Lung Dis. 1993;74:332–337. doi: 10.1016/0962-8479(93)90108-A. [DOI] [PubMed] [Google Scholar]
- 29.Juvekar SK, Morankar SN, Dalal DB, Rangan SG, Khanvilkar SS, Vadair AS, et al. Social and operational determinants of patient's behaviour in lung tuberculosis. Indian J Tuberc. 1995;42:87–94. [Google Scholar]
- 30.Uplekar MW, Rangan S, Tackling TB. the search for solutions. The Foundation for Research in Community Health, Mumbai, India. 1996 [Google Scholar]
- 31.Nair DM, George A, Chacko KT. Tuberculosis in Bombay: new insights from poor urban patients. Health Policy Plan. 1997;12:77–85. doi: 10.1093/heapol/12.1.77. [DOI] [PubMed] [Google Scholar]
- 32.Singla N, Sharma P, Singla R, Jain RC. Survey of knowledge, attitudes and practices for tuberculosis among general practitioners in Delhi, India. Int J Tuberc Lung Dis. 1998;2:384–9. [PubMed] [Google Scholar]
- 33.Morankar S, Weiss MG. Impact of gender on illness experience and behaviour: Implications for tuberculosis control in rural Maharashtra. Health Adm. 2003;15:149–55. [Google Scholar]
- 34.Long NH, Johanson E, Lonnroth K, Eriksson B, Winkvist A, Diwan VK. Longer delays in tuberculosis diagnosis among women in Vietnam. Int J Tuberc Lung Dis. 1999;3:388–93. [PubMed] [Google Scholar]
- 35.Cambanis A, Yassin MA, Ramsay A, Squire SB, Arbide I, Cuevas LE. Rural poverty and delayed presentation to tuberculosis services in Ethiopia. Trop Med Int Health. 2005;10:330–5. doi: 10.1111/j.1365-3156.2005.01393.x. [DOI] [PubMed] [Google Scholar]
- 36.Chakraborty AK. Missed opportunities for diagnosis of pulmonary tuberculosis: a study among rural patients seeking relief on their own under the tuberculosis program in India. Indian J Tuberc. 2001;48:181–92. [Google Scholar]
- 37.Needham DM, Foster SD, Tomlinson G, Godfrey- Faussett P. Socio-economic, gender and health services factors affecting diagnostic delay for tuberculosis patients in urban Zambia. Trop Med Int Health. 2001;6:256–9. doi: 10.1046/j.1365-3156.2001.00709.x. [DOI] [PubMed] [Google Scholar]
- 38.Huong NT, Vree M, Duong BD, Khanh VT, Loan VT, Co NV, et al. Delays in the diagnosis and treatment of tuberculosis patients in Vietnam: A cross-sectional study. BMC Public Health. 2007;7:110. doi: 10.1186/1471-2458-7-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karim F, Islam MA, Chowdhury AM, Johansson E, Diwan VK. Gender differences in delays in diagnosis and treatment of tuberculosis. Health Policy Plan. 2007;22:329–34. doi: 10.1093/heapol/czm026. [DOI] [PubMed] [Google Scholar]
- 40.Gender and tuberculosis. Geneva: World Health Organization; 2002. [Last accessed on 2007 Jun 28]. World Health Organization. Available from: http://www.who.int/gender/other health/en/gender/TB.pdf . [Google Scholar]
- 41.Uplekar M, Rangan S, Ogden J. Gender and tuberculosis control: Towards a strategy for research and action. 1999 WHO/CDS/TB/2000.280. [Google Scholar]


