Abstract
BACKGROUND:
The objective of this study was to determine the effects of nutritional educational program on glycemic control of elderly patients with type 2 diabetes.
METHODS:
In this parallel randomized controlled educational trial, 100 diabetic elderly patients (≥60 years) were chosen (50 in control and 50 in test group). Nutrition education based on beliefs, attitudes, subjective norms and enabling factors (BASNEF model) was conducted. Dietary intake and glycemic indices as well as the components of the BASNEF model were assessed. The four 70-minute educational sessions were conducted in one month. Three months after training intervention, questionnaire was completed again and blood tests were performed.
RESULTS:
Increased intake in the mean daily servings of fruits (0.91± 0.82 vs. 0.17±0.79; p < 0.001), vegetables (0.87±0.86 vs. 0.03±1; p < 0.001) and dairy (0.35±0.52 vs. and 0.12±0.76; p < 0.001) were reported in the intervention group compared to the control group (p < 0.001). The amount of fruits, vegetables and dairy increased in the intervention group at the end of the study (p < 0.001). However, it was not significantly changed in the control group. HbA1c and fasting blood sugar (FBS) levels decreased significantly in the interventional group compared to the control group (p < 0.001). Comparing the amount of FBS and HbA1c at the end of the study with the baseline measurements showed significant reduction in interventional group (p < 0.001). However, there was no significant change in control group in this regard.
CONCLUSIONS:
BASNEF–based nutritional educational intervention improved dietary intakes as well as glycemic control, 3 months after intervention.
KEYWORDS: Nutrition Education, BASNEF Model, Type 2 Diabetes Mellitus
Diabetes is recently considered to be a major health concern both in developing countries and developed ones. According to the estimates, the prevalence of type 2 diabetes will increase to 366 million in 2030.1 However, by increasing age the prevalence of diabetes increases from 10% to 20%.2,3 Based on the results of the Framingham's heart study, elderly diabetic people live 7.5 to 8.2 year less than healthy ones4 and they also have more problems and special diseases such as nephropathy, cardiovascular diseases, retinopathy and micro and macro-vascular problems.5,6 Lower quality of life is more prevalent among elderly with diabetes compared to healthy older adult.7,8
Different interventional programs can reduce the morbidities and mortalities of diabetic patients. Nutritional interventions are one of the most important ones. Nutritional intervention can have beneficial effects on the markers of glycemic control and other cardiovascular risks.9 Following nutritional intervention, the complications of diabetes mellitus also will be improved.10
Life style modifications including changing the nutritional habits are difficult kinds of interventions. Having knowledge regarding the nutritional recommendation is not enough and even in spite of good knowledge, it is difficult for patients to act according to the knowledge.11 This is more important in elderly patients with type 2 diabetes due to lower knowledge of nutrition.12 Previous studies pointed out the important role of nutrition education in controlling glucose in elderly with diabetes13 and mentioned the key role of education for changing nutritional habits.14 The effectiveness of nutritional educational programs also is important. A change of behavior model that is suitable for nutritional educational programs is Hubly's change of behavior model. This model includes beliefs, attitudes, subjective norms and enabling factors (BASNEF Model).15 Behavioral attitude is a product of one's belief; in fact, it is the positive or negative evaluation of behavior. Subjective norms are one's belief relative to influential persons and this is on social pressures and reflections. Enabling factors are skills and sources that allow person's aim or intention to change the behavior.16 The novelty of the present study is related to the type of study participants. We chose elderly patients with type 2 diabetes. According to our knowledge, there is no study regarding the effects of educational model among elderly patients. Almost all the studies on diabetes have been conducted on newly diagnosed and not elderly patients. It is always a question if the educational model can be effective among elderly patients. Furthermore, BASNEF model has not been administered for the educational intervention yet. Therefore, another innovation of the present study was the application of this kind of educational model.
Based on the cited materials and paucity of interventions performed in nutrition education of elderly, this study was performed to determine the effect of nutrition education on knowledge and dietary behaviors as well as glycemic control status of elderly patients with type 2 diabetes based on BASNEF model.
Methods
This study was a randomized controlled educational trial. The studied population included elderly patients with type 2 diabetes in Isfahan (Iran) Diabetes Institution during 2010. The age of participants was 60 years or greater and none had cognitive or motor disabilities. The participants in the present study were chosen by stratified random sampling method from among elderly patients with type 2 diabetes. 100 elderly with type 2 diabetes were chosen and were randomly divided to intervention (n=50) and control (n=50) groups (Figure 1). Inclusion criteria were being more than 60 years old, consuming no special diet for a kind of specific disease, having type 2 diabetes for at least one year, and not having moving disability or cognitive impairment. Those patients that did not participate in one educational session were excluded from the study. The sample size was calculated by this formula:
Figure 1.
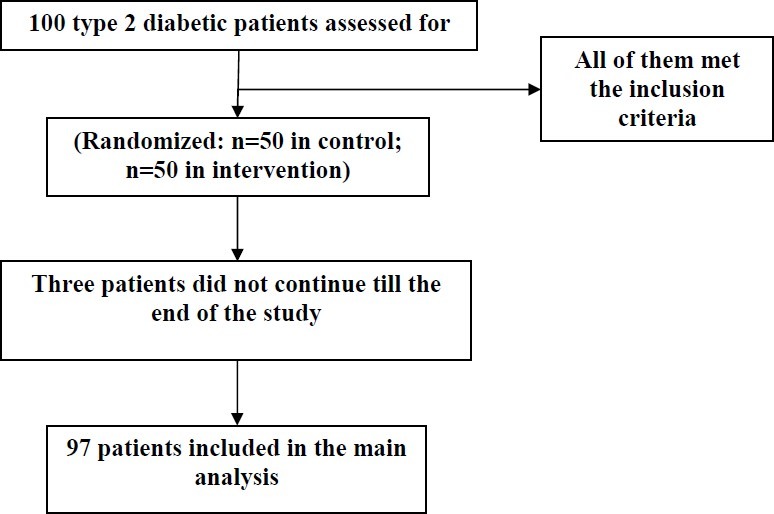
Patients diagram during the present study.
![]()
Therefore, it was needed to have 44 patients in each group. This study was approved by the research council and ethics committee of Isfahan University of Medical Sciences. Written informed consent was completed by all the patients.
This was an educational intervention based on BASNEF model. This model includes beliefs, attitudes, subjective norms and enabling factors.
The data collection tools in this study included: A) questionnaire designed based on BASNEF model and included demographic characteristics (14 items), knowledge questions (15 items), attitude to behavioral beliefs (5 items) and evaluations of behavioral outcomes (5 items), enabling factors (5 items) , and subjective norms (5 item). This questionnaire was completed by structured interview. The scoring method of the questionnaire was such that 1 score was given to the true answer and zero was given to the false answer in knowledge part. In beliefs part, it was designed on 3-point Likert scales and score range of each item varied between 1 to 3 so that 1 score was given to “I disagree” , 2 scores to “I do not have idea”, and 3 scores to “I agree”. About subjective norms and enabling factors, items were designed as 2–options. The scale of scores was considered out of 100 for all parts of questionnaire.
The validity of given questionnaire was measured by content validity and face validity methods. The questionnaire was provided on sources and valid books. Five experts’ views were given for assessing content validity. Some of the suggestions of the reviewers were used to change the wording of the questionnaire. This questionnaire was given to 20 elderly patients with diabetes (similar but non-participants in the study) for confirming face validity and explanations, questions and defects of the questionnaire were considered. The reliability of given questionnaire was confirmed by test–retest for knowledge questions (r=0.76) and by internal validity for attitude questions (α=0.80).
B) Three days food record questionnaire was used for assessing nutrition performance of diabetic elderly. For assessing the amount of each food group consumption the gram of each kind of food was changed to equivalent servings based on the original USDA Food Guide Pyramid.
c) Biochemical tests of blood including fasting plasma glucose (FBS) and HbA1C were performed in a lab. FBS was measured via enzymatic method with a commercially enzymatic kit (Parsazmoon-2010) by using autoanalyzer (BT3000). Hb1AC was measured according to the immunoturbidimetric method using Rondex commercially kit (Rondox-2010) by using autoanalyzer (BT3000). Before educational intervention in intervention and control groups, the given questionnaires were completed and patients were referred to the lab for doing tests with an introducing letter.
The four 70-minute educational sessions were conducted during one month. The goals of the sessions were to increase the frequency of meals, to decrease use of fat and simple sugars and to increase use of fruits and vegetables for intervention group. The final session included patients‘ family that was conducted with the presence of staff and participants. Content of education was transferred to target group by lecture, question and answer, and discussion. Education pamphlets were given to patients’ family in order to involve them in intervention at the end of educational session. Telephone follow-ups in week 4 and 8 after intervention by researchers to patients and their families were done in order to emphasize on educational materials, and to response to possible questions of the patients. Three months after training intervention, questionnaire was completed in both intervention and control groups again and blood tests were performed in order to determine the indices regarding the glycemic control. All the nutritional educations were provided by the nutritionist. Control group received usual care and they did not receive specific nutritional education. SPSS software (version 15) was used for data analysis. χ2 test, and McNemar tests were used for comparing the qualitative variables. Independent-sample t test and paired-sample t test were used in the present study for comparing the quantitative variables.
Results
In the present study, 97 of the original 100 patients completed the study (48 in intervention group and 49 in control group). Two persons in intervention group did not continue the education sessions due to physical problems and one patient in control group did not continue the study due to travel.
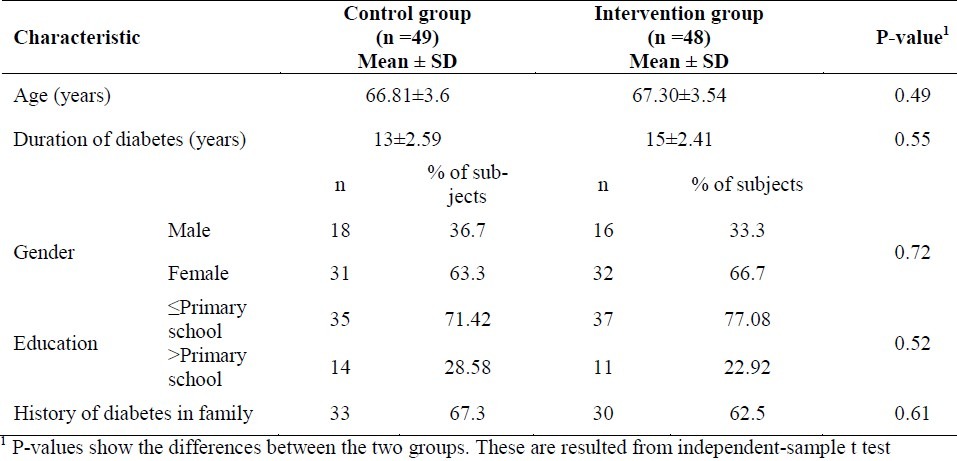
The mean age of the participants was 67.06±3.56 year. Monthly mean income did not show significant difference between the two groups (p=0.42). Moreover, the two groups were similar in other demographic variables (Table 1).
Table 1.
Demographic Characteristics of the Sample.
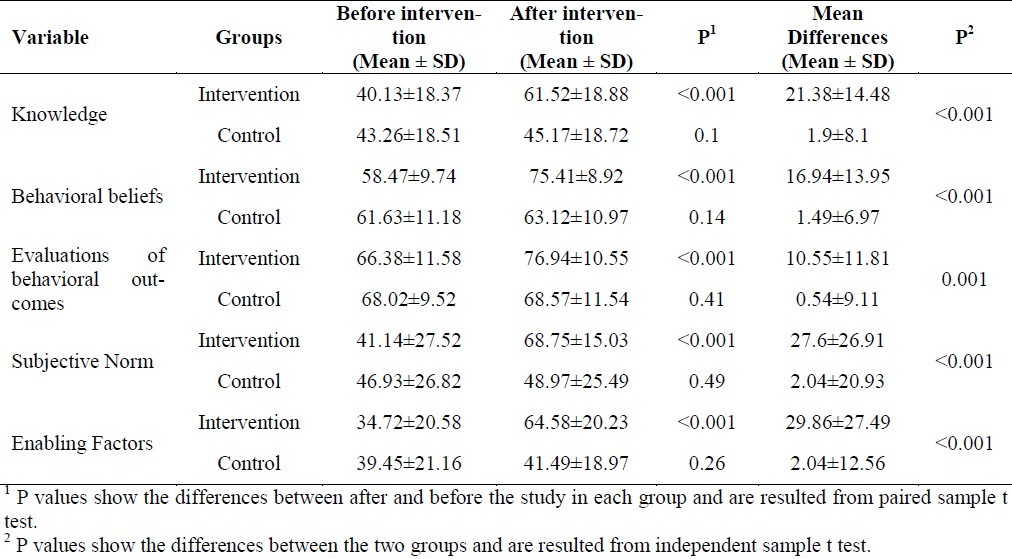
There were no significant differences between the two groups regarding any studied variables prior to the intervention. Mean score of components of BASNEF model showed significant increase in intervention group after intervention, while such increase was not seen in control group. Moreover, independent-sample t test showed a significant difference between the control and intervention groups in mean change of knowledge, behavioral beliefs, evaluations of behavioral outcomes, enabling factors and subjective norms (p<0.001 for all) (Table 2).
Table 2.
Mean ± SD of the of BASNEF constructs at baseline and 3 months after educational intervention in the intervention and control groups
After educational intervention, the prevalence of those patients that consumed more frequent meals was significantly higher in the intervention group compared with before study (P<0.001), however, it was not significantly different in the control group (P=0.51). Mean servings of bread-grain intake decreased in intervention group (Mean differences: -1.01 ±1.93 serving/day) and increased in control groups (Mean differences: 0.13 ±1.28 serving/day). The mean difference between these two group changes was significant (p <0.001). In the intervention group, fruit intake increased more than that in the control group (0.91±0.82 vs. 0.17±0.79 serving/day, respectively; p <0.001). The mean servings of vegetable intake increased by 0.87±0.86 servings/day in the intervention group and decreased by -0.03±1 serving/day in the control group (p<0.001). Dairy intake also increased in the intervention group more than that in the control group (mean differences: 0.35±0.52 vs. 0.12±0.76 serving/day, respectively; p<0.001). Fat intake decreased in the intervention group (mean differences: -1.29±1.36 vs. -0.2±0.86 serving/day, respectively; p<0.001). There were no significant differences regarding the amount of meat intake between the two groups (Table 3).
Table 3.
Mean ± SD of the nutrition behavior and glycemic control indices in diabetic patients at baseline and after intervention in the intervention and control groups and the mean differences.
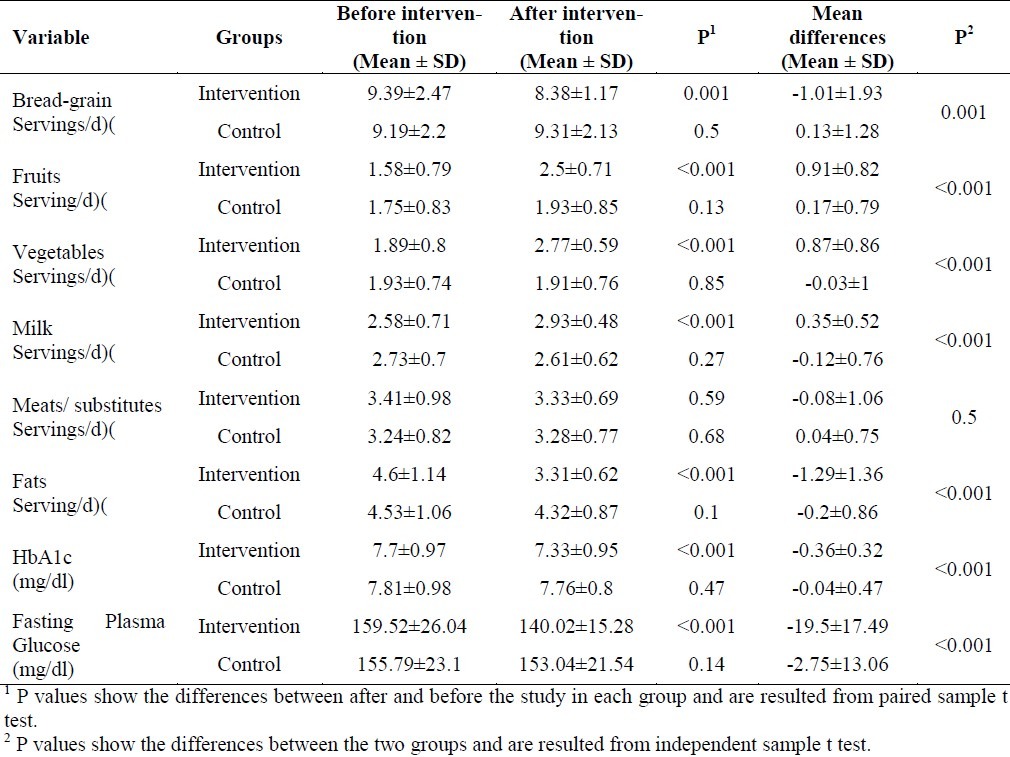
Table 3 shows mean indices of glucose control before and 3 months after educational intervention. A comparison of the mean differences of HbA1C (-0.36±0.32 vs. -0.04±0.47%, respectively; p<0.001) and fasting plasma glucose (-19.5±17.49 vs. -2.75±13.06 mg/dl, respectively; p<0.001) in intervention and control groups showed significant difference 3 months after educational intervention (p<0.001). Comparing the values of FBS at the end of study with the baseline values in the intervention group showed significant change (159.52±26.04 mg/dl at baseline vs. 140.02±15.28 mg/dl at the end of the study; p<0.001). However, it was not changed significantly in the control group. HbA1c decreased significantly at the end of the study in the intervention group (7.7±0.97 vs. 7.33±0.95%, respectively; p<0.001). HbA1c did not change significantly in the control group.
Discussion
The results of the present study revealed that mean change of knowledge, behavioral beliefs, evaluations of behavioral outcomes, enabling factors and subjective norms increased significantly in the intervention group. Furthermore, the number of meals during a day and also the number of fruits, vegetables, and dairy servings increased in the intervention group while the number of bread-grain servings decreased.
Significant change in the mean knowledge score of patients in intervention group is the sign of the effect of educational intervention in improving knowledge of this group. The importance of educational intervention has been also mentioned in other studies.17,18 Some studies cited BASNEF-based educational interventions are more effective than classic nutritional education to increase knowledge level.19 Pressure of social norms and enabling factors used in BASNEF model leads to promote patients’ knowledge. Effects of application of BASNEF model in promoting patients knowledge was stated in other BASNEF-based educational interventions performed on diabetic patients19,20 and even other patients with chronic diseases.21
In the present study, the use of the BASNEF model could improve the attitude of dietary behaviors in the intervention group compared to the control group. There are some reports of positive effects of education on improving diabetic patients’ attitude.15,20,22 In another study on type 2 diabetes, significant difference was not reported between the control and the intervention groups about attitude regarding diet.23 It seems that educational methods have an important role in changing patients attitude in different studies.
In the present study, elderly attitude improved by using BASNEF model in planning and performing intervention and also by using educational methods such as discussion and question and answer in educational sessions. In a study conducted by Rakhshanderou et al.24, the use of education theories have been emphasized for changing the attitudes24 and in other studies, the role of educational methods of discussion and question and answers has been mentioned as an effective method in improving nutritional attitude.19,25
The findings of the present study showed that enabling factors were increased significantly in the intervention group as main constructs of BASNEF model. These factors for intervention group included information, dietary skills, opportunity of nutrition education and consultation. They had a nutrition consult with a dietitian or other qualified nutrition professional on a one-on-one basis. While non-existence of such factors in the control group led to no change of their mean score of enabling factors. Many BASNEF–based studies pointed out the unique role of enabling factors in changing behavioral intention to health behaviors.19,25
Following the intervention, the mean score of subjective norms showed significant increase in intervention group. In this study, social norms were divided into four factors (family, peer group, staff and researchers). Educational intervention led to improved mean scale of social norms by involving four factors in the study. Various studies reported family and peers as key factors in dietary behaviors26–28 and specifically family is important for elderly patients with diabetes.12 Some studies also pointed out the importance of staff's’ role in curing diabetic patients.29
The present study was performed with the purpose of changing dietary behavior among elderly patients with diabetes, including an increase in frequency of meals, decrease in use of fat and simple sugar and increased intake of fruits and vegetables. Frequency of meals showed 35% increase in intervention group, while the mean intake of fat and bread-grain group showed significant decrease. In addition, the number of servings of fruits and vegetables group showed significant increase in the intervention group after nutritional educational intervention. Previous studies showed that high fiber diets help to improve risk factors of cardiovascular diseases in diabetic patients.30–32 In the present study, the number of servings of dairies increased in the intervention group. Calcium is an important factor in the diet of diabetic patients.13 In addition, calcium improves sodium–potassium balance and decreases the weight and increases the sensitivity of insulin.33,34 A recent study on type 2 diabetes revealed that even consuming diet with high amount of low fat or fat free dairy products as part of the Dietary Approaches to Stop Hypertension (DASH) diet, had beneficial effects on the glycemic control and cardiovascular risks.35,36
In this study, biochemical indices of glucose control were measured. After 3 months nutritional educational intervention, HbA1C was decreased significantly in intervention group, while changes were not significant in the control group. Elevated HbA1C was associated with increased risk of mortality from cardiovascular diseases.37 Therefore, the effect of interventions on the level of HbA1C is important. In addition, significant change in fasting plasma glucose (FPG) was observed, so that intervention could decrease FPG to 140 mg/dl in intervention group. It seems that improvement of indices of glucose control can be resulted from decreasing the amount of simple sugars and refined carbohydrates and increasing the amount of fruits and vegetables intake in intervention group. A recent meta–analysis in 2008 showed that lower intake of refined carbohydrates led to improvement in the indices of glucose control.38
Decreasing the rate of tendency for follow up during the study was one of the limitations of the current study. Although, application of the educational model and involving family of patients in intervention might increase the hopefulness for continuing the results during longer time.39,40 Moreover, due to study on elderly population, researchers had a limited number of educational sessions. We compared the effects of BASNEF educational model in the present study with a control group because we had no reports regarding the beneficial effects of this model among elderly with diabetes. However, it was better that BASNEF model had been compared with another educational model. It is suggested that future studies compare the effects of this model with other educational models.
The results of the current study could extrapolate to other population groups with diabetes. As this model was effective in elderly group, it might be also appropriate for other groups with diabetes.
Finally, BASNEF-based nutritional educational intervention led to improved dietary behaviors in addition to improved knowledge and attitudes of older adults with diabetes, which were associated with improved indices of blood glucose control following a three-month intervention.
Authors’ Contributions
GRSH, AN, AH, and LA participated in the design and conducting the study and preparing the manuscript. All authors read and approved the final manuscript.
Acknowledgement
This study was granted by Isfahan University of Medical Sciences, Isfahan, Iran. This was a MS degree thesis approved in the school of Public Health, Isfahan University of Medical Sciences (thesis no: 388419).
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Caughey GE, Roughead EE, Vitry AI, McDermott RA, Shakib S, Gilbert AL. Comorbidity in the elderly with diabetes: Identification of areas of potential treatment conflicts. Diabetes Res Clin Pract. 2010;87(3):385–93. doi: 10.1016/j.diabres.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Vischer UM, Bauduceau B, Bourdel-Marchasson I, Blickle JF, Constans T, Fagot-Campagna A, et al. A call to incorporate the prevention and treatment of geriatric disorders in the management of diabetes in the elderly. Diabetes Metab. 2009;35(3):168–77. doi: 10.1016/j.diabet.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167(11):1145–51. doi: 10.1001/archinte.167.11.1145. [DOI] [PubMed] [Google Scholar]
- 5.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884–90. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 6.Lustman PJ, Gavard JA. Psychosocial aspects of diabetes in adult populations. In: Aubert RE, Ballard DJ, Barrett-Connor E, Boyko EJ, Buchanon TA, Chang YF, editors. Diabetes in America. 2nd ed. Mary Land: National Institutes of Health; 1995. [Google Scholar]
- 7.Schlater A. Diabetes in the elderly: The geriatrician's perspective. Can J Diabetes. 2003;27:172–5. [Google Scholar]
- 8.Miller DK, Lui LY, Perry HM, III, Kaiser FE, Morley JE. Reported and measured physical functioning in older inner-city diabetic African Americans. J Gerontol A Biol Sci Med Sci. 1999;54(5):M230–M236. doi: 10.1093/gerona/54.5.m230. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez LM, Castellanos VM. Use of low-fat foods by people with diabetes decreases fat, saturated fat, and cholesterol intakes. J Am Diet Assoc. 2000;100(5):531–6. doi: 10.1016/s0002-8223(00)00165-6. [DOI] [PubMed] [Google Scholar]
- 10.Harding AH, Day NE, Khaw KT, Bingham S, Luben R, Welsh A, et al. Dietary fat and the risk of clinical type 2 diabetes: the European prospective investigation of Cancer-Norfolk study. Am J Epidemiol. 2004;159(1):73–82. doi: 10.1093/aje/kwh004. [DOI] [PubMed] [Google Scholar]
- 11.Campbell LV, Barth R, Gosper J. Unsatisfactory nutritional parameters in non-insulin-dependent diabetes mellitus. Med J Aust. 1989;151(3):146–50. doi: 10.5694/j.1326-5377.1989.tb139599.x. [DOI] [PubMed] [Google Scholar]
- 12.Meneilly GS, Tessier D. Diabetes in elderly adults. J Gerontol A Biol Sci Med Sci. 2001;56(1):M5–13. doi: 10.1093/gerona/56.1.m5. [DOI] [PubMed] [Google Scholar]
- 13.Rizvi AA. Nutritional challenges in the elderly with diabetes. Int J Diabetes Mellit. 2009;1(1):26–31. [Google Scholar]
- 14.Sahyoun NR, Pratt CA, Anderson A. Evaluation of nutrition education interventions for older adults: a proposed framework. J Am Diet Assoc. 2004;104(1):58–69. doi: 10.1016/j.jada.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Salehi M, Kimiagar SM, Shahbazi M, Mehrabi Y, Kolahi AA. Assessing the impact of nutrition education on growth indices of Iranian nomadic children: an application of a modified beliefs, attitudes, subjective-norms and enabling-factors model. Br J Nutr. 2004;91(5):779–87. doi: 10.1079/BJN20041099. [DOI] [PubMed] [Google Scholar]
- 16.Glanz K, Rimer B, Viswanath K. 4th ed. San Francisco: Jossey -Bass; 2008. Health Behavior and Health Education: Theory, Research, and Practice. [Google Scholar]
- 17.Tankova T, Dakovska G, Koev D. Education of diabetic patients--a one year experience. Patient Educ Couns. 2001;43(2):139–45. doi: 10.1016/s0738-3991(00)00159-2. [DOI] [PubMed] [Google Scholar]
- 18.Rezaei N, Tahbaz F, Kimiagar M, Alavi Majd H. The effect of nutrition education on knowledge, attitude and practice of type 1 diabetic patients from Aligoodarz. J Shahrekord Univ Med Sci. 2006;8(2):52–9. [Google Scholar]
- 19.Hazavehei SMM, Sharifirad GhR, Kargar M. The Comparison of Educational Intervention Effect Using BASNEF and Classic Models on Improving Assertion Skill Level. J Res Health Sci. 2008;8(1):1–11. [PubMed] [Google Scholar]
- 20.Baghyani-Moghadam MH, Shafiei F, Haydarneia AR, Afkhami M. Efficacy of BASNEF Model in Controlling of Diabetic Patients in the City of Yazd, Iran. Indian J Community Med. 2005;30(4):10–2. [Google Scholar]
- 21.Baghianimoghadam MH, Rahaee Z, Morowatisharifabad MA, Sharifirad G, Andishmand A, Azadbakht L. Effects of education on self-monitoring of blood pressure based on BASNEF model in hypertensive patients. J Res Med Sci. 2010;15(2):70–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Shabbidar S, Fathi B. Effect of nutrition education on knowledge, attitude, and practice of type 2 diabetic patients. J Birjand Univ Med Sci. 2007;14(1(30)):31–7. [Google Scholar]
- 24.Rakhshanderou S, Gaffari M, Heydarnia A, Rajab A. Effectiveness of educational interventions on metabolic control in diabetic patients referred to the Diabetes Center of Iran. Iranian J Diabetes Lipid. 2010;9(Special Issue: risk factors for diabetes and cardiovascular disease):57–64. [Google Scholar]
- 25.Hazavehei MM, Khani Jyhouni A, Hasanzade A, Rashidi M. The effect of educational program based on BASNEF model on diabetic (Type II) eyes care in Kazemi's clinic, (Shiraz) Iranian J Endocrinology Metab. 2008;10(2):145–54. [Google Scholar]
- 26.Perez-Escamilla R, Hromi-Fiedler A, Vega-Lopez S, Bermudez-Millan A, Segura-Perez S. Impact of peer nutrition education on dietary behaviors and health outcomes among Latinos: a systematic literature review. J Nutr Educ Behav. 2008;40(4):208–25. doi: 10.1016/j.jneb.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klomegah RY. The influence of social support on the dietary regimen of people with diabetes. Sociation Today. 2006;4(2):104–8. [Google Scholar]
- 28.Wilson W, Pratt C. The impact of diabetes education and peer support upon weight and glycemic control of elderly persons with noninsulin dependent diabetes mellitus (NIDDM) Am J Public Health. 1987;77(5):634–5. doi: 10.2105/ajph.77.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ciechanowski P, Russo J, Katon W, Von KM, Ludman E, Lin E, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med. 2004;66(5):720–8. doi: 10.1097/01.psy.0000138125.59122.23. [DOI] [PubMed] [Google Scholar]
- 30.Weickert MO, Mohlig M, Schofl C, Arafat AM, Otto B, Viehoff H, et al. Cereal fiber improves whole-body insulin sensitivity in overweight and obese women. Diabetes Care. 2006;29(4):775–80. doi: 10.2337/diacare.29.04.06.dc05-2374. [DOI] [PubMed] [Google Scholar]
- 31.Qi L, van Dam RM, Liu S, Franz M, Mantzoros C, Hu FB. Whole-grain, bran, and cereal fiber intakes and markers of systemic inflammation in diabetic women. Diabetes Care. 2006;29(2):207–11. doi: 10.2337/diacare.29.02.06.dc05-1903. [DOI] [PubMed] [Google Scholar]
- 32.American Diabetes Association. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25(1):202–12. doi: 10.2337/diacare.25.1.202. [DOI] [PubMed] [Google Scholar]
- 33.Pimentel GD, Arimura ST, de Moura BM, Silva ME, de Sousa MV. Short-term nutritional counseling reduces body mass index, waist circumference, triceps skinfold and triglycerides in women with metabolic syndrome. Diabetol Metab Syndr. 2010;2:13. doi: 10.1186/1758-5996-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang L, Manson JE, Buring JE, Lee IM, Sesso HD. Dietary intake of dairy products, calcium, and vitamin D and the risk of hypertension in middle-aged and older women. Hypertension. 2008;51(4):1073–9. doi: 10.1161/HYPERTENSIONAHA.107.107821. [DOI] [PubMed] [Google Scholar]
- 35.Azadbakht L, Fard NR, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, et al. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care. 2011;34(1):55–7. doi: 10.2337/dc10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. 2011;141(6):1083–8. doi: 10.3945/jn.110.136739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pimentel GD, Portero-McLellan KC, Oliveira EP, Spada AP, Oshiiwa M, Zemdegs JC, et al. Long-term nutrition education reduces several risk factors for type 2 diabetes mellitus in Brazilians with impaired glucose tolerance. Nutr Res. 2010;30(3):186–90. doi: 10.1016/j.nutres.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Livesey G, Taylor R, Hulshof T, Howlett J. Glycemic response and health--a systematic review and meta-analysis: relations between dietary glycemic properties and health outcomes. Am J Clin Nutr. 2008;87(1):258S–68S. doi: 10.1093/ajcn/87.1.258S. [DOI] [PubMed] [Google Scholar]
- 39.Miller CK, Edwards L, Kissling G, Sanville L. Evaluation of a theory-based nutrition intervention for older adults with diabetes mellitus. J Am Diet Assoc. 2002;102(8):1069–81. doi: 10.1016/s0002-8223(02)90242-7. [DOI] [PubMed] [Google Scholar]
- 40.Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving self-care among older patients with type II diabetes: the “Sixty Something…” Study. Patient Educ Couns. 1992;19(1):61–74. doi: 10.1016/0738-3991(92)90102-o. [DOI] [PubMed] [Google Scholar]


