Abstract
Background
Published data on the epidemiology of meningococcal disease in Latin America and the Caribbean region is scarce and, when available, it is often published in Spanish and/or in non-peer-reviewed journals, making it difficult for the international scientific community to have access.
Methods
Laboratory data on 4,735 Neisseria meningitidis strains was collected and reported by the National Reference Laboratories in 19 Latin American countries and the Caribbean Epidemiology Centre (CAREC) between 2006 and 2010 as part of the work carried out by the SIREVA II network. Serogroup and MIC to penicillin, rifampin and chloramphenicol were determined.
Results
Isolates were mainly obtained from patients <5 years, but each year around 25% of isolates came from adult patients. Serogroup distribution was highly variable among countries. Serogroup C was the main cause of disease in Brazil; the majority of disease seen in the Southern cone was caused by serogroup B, but serogroup W135 strains have increased in recent years. In the Andean and Mexico, Central America and Caribbean regions, serogroups B and C were equally present, and serogroup Y was frequently isolated. Isolates were generally susceptible to chloramphenicol, penicillin and rifampin, but almost 60% of isolates characterized in Southern cone countries presented intermediate resistance to penicillin. Five rifampin-resistant isolates have been isolated in Uruguay and Brazil.
Conclusions
Serogroup distribution is highly variable among countries, but some geographic structuring can be inferred from these data. Epidemiological and laboratory data are scarce among Andean and Mexico, Central America and Caribbean countries. Evaluation and implementation of corrective measures on disease surveillance and reporting systems and the implementation of molecular diagnostic techniques and molecular characterization on meningococcal isolates are advised.
Introduction
Neisseria meningitidis is a leading cause of invasive disease in the form of meningitis and scepticæmia worldwide. Invasive meningococcal disease (IMD) is associated with a high case-fatality rate and survivors are often left with severe long-term neurological sequelæ [1].
In industrialized countries, IMD is presented in sporadic cases with small localized outbreaks occurring occasionally [2]–[8]. In these countries, incidence rates remain low and rarely surpass 1/100,000 [9]. Large epidemics are restricted to Africa and, specifically to the area known as the “meningitis belt” [10], [11], [12].
Disease causing serogroups vary widely across continents. Serogroup A is associated with epidemic outbreaks in Africa and, occasionally, in other parts of the world, whereas serogroup B is the leading cause of disease in Australia and New Zealand, as well as in Europe [9], [13], especially since the introduction of the meningococcal C conjugate vaccine in the national vaccination schedules of many countries [14]–[17]. In the United States, serogroups B, C and Y account for the majority of disease in the United States, although the implementation of the tetravalent A, C, W135, Y conjugate vaccine for children from the age of eleven has contributed to a substantial reduction on disease incidence [18].
Despite being a disease of compulsory notification and presumably a leading cause of invasive bacterial disease in Latin America, the real burden of meningococcal disease is widely underestimated in the majority of countries in the region. Reported annual incidence rates range from the approximately 2/100,000 cases reported annually from Brazil, a country with a well-established surveillance and reporting system, to figures below 0.1/100,000 in countries such Paraguay, Costa Rica or Mexico, or even countries where no cases of disease have been confirmed for years [19].
The reasons for this are diverse and also vary from country to country, but differences on clinical definition of cases and management of patients, difficulties on the isolation, identification and characterization of the bacterium, and under-notification to the national reporting system are common problems in the region [19], [20].
Since 1993, the Pan-American Health Organization (PAHO) has run a laboratory-based regional surveillance system; SIREVA (Sistema Regional de Vacunas) and later SIREVA II (Sistema de Redes de Vigilancia de Agentes Bacterianos Causantes de Meningitis y Neumonías) aimed at the collection of relevant laboratory and epidemiological data on the invasive disease-causing bacteria, Streptococcus pneumoniae, Haemophilus influenzae (1997) and, since 2000, Neisseria meningitidis [20]–[23].
Meningococcal vaccines are not available through the public sector in Latin American countries, with two exceptions: Cuba introduced in 1991 the Cuban-developed outer-membrane protein based vaccine VA-MENGOC-BC®, which achieved a significant reduction of IMD incidence rates in the country [24], [25], [26]. And Brazil is currently the only country in Latin America that has introduced a meningococcal serogroup C conjugate vaccine in its national immunization scheme for children under the age of two [27], but in contrast to the majority of European countries, no catch-up campaign on teenagers is planned. However, meningococcal vaccination is available through the private sector in many Latin American countries. It is crucial for public health authorities and policy makers that data regarding distribution and characteristics of disease-causing strains in Latin America is made available so a cost-effective vaccination campaign with the right vaccine formulation can be implemented through the National Program of Immunization, targeting at including all individuals on the selected groups to be vaccinated regardless of their socio-economic status. This paper reviews available laboratory-based data on serogroup distribution and antibiotic resistance of Neisseria meningitidis generated by countries from the Latin America and Caribbean region within the SIREVA II network for the period 2006–2010 [28]–[32].
Materials and Methods
SIREVA II Network
In 1993, the Pan-American Health Organization (PAHO) started a regional laboratory-based passive surveillance program, aiming at obtaining quality laboratory data on disease-causing Streptococcus pneumoniae strains. Surveillance was extended to Haemophilus influenzae in 1997 and Neisseria meningitidis in 2000, Currently, the SIREVA II network includes 19 national reference laboratories (NRLs) from an equivalent number of countries from the Latin American and Caribbean region participate in the SIREVA II network: Argentina, Bolivia, Brazil, Chile, Colombia, Costa Rica, Cuba, Ecuador, El Salvador, Guatemala, Honduras, México, Nicaragua, Panama, Paraguay, Peru, Dominican Republic, Uruguay and Venezuela. Additionally, the Caribbean Epidemiology Centre (CAREC), which provides reference laboratory services for 21 countries in the Caribbean, is also part of the network. The Instituto Adolfo Lutz (IAL) in São Paulo, Brazil serves as the regional reference laboratory (RRL) for Neisseria meningitidis, and the Instituto de Salud Carlos III in Madrid, Spain (ISCIII), acts as global reference laboratory for this bacterium [20], [21], [33], [34].
Data have been grouped into four geographic regions: (i) Brazil, (ii) Southern cone (Argentina, Chile, Paraguay and Uruguay), (iii) Andean Region (Bolivia, Colombia, Ecuador, Peru and Venezuela), and (iv) Mexico, Central America and Caribbean (Mexico, CAREC, Costa Rica, Cuba, Dominican Republic, El Salvador, Guatemala, Honduras, Nicaragua, and Panama) (Table 1).
Table 1. Isolates received from each participating country.
| Country and regions | Year | Total | |||||
| 2006 | 2007 | 2008 | 2009 | 2010 | |||
| n | n | % | |||||
| Brazil | 628 | 563 | 622 | 582 | 686 | 3,081 | 65.1 |
| South Cone | 1,126 | 23.8 | |||||
| Argentina | 64 | 119 | 142 | 132 | 134 | 591 | |
| Chile | 71 | 82 | 57 | 60 | 56 | 326 | |
| Paraguay | 7 | 13 | 13 | 9 | 7 | 49 | |
| Uruguay | 40 | 46 | 32 | 22 | 20 | 160 | |
| Andean | 260 | 5.5 | |||||
| Colombia | 25 | 39 | 22 | 21 | 17 | 124 | |
| Venezuela | 25 | 28 | 24 | 16 | 18 | 111 | |
| Ecuador | 6 | 5 | 8 | 0 | 1 | 20 | |
| Bolivia | 0 | 0 | 2 | 0 | 0 | 2 | |
| Peru | 0 | 0 | 1 | 1 | 1 | 3 | |
| Mexico, Central America & Caribbean | 268 | 5.7 | |||||
| Mexico | 10 | 13 | 10 | 2 | 17 | 52 | |
| El Salvador | 5 | 6 | 6 | 6 | 2 | 25 | |
| Nicaragua | 2 | 0 | 0 | 2 | 1 | 5 | |
| Honduras | 1 | 0 | 0 | 2 | 0 | 3 | |
| Costa Rica | 18 | 7 | 7 | 2 | 1 | 35 | |
| Panama | 4 | 9 | 28 | 13 | 12 | 66 | |
| Dominican Republic | 18 | 10 | 4 | 1 | 10 | 43 | |
| Cuba | 8 | 4 | 7 | 6 | 6 | 31 | |
| CAREC | 5 | 3 | 0 | 0 | 0 | 8 | |
| TOTAL | 937 | 947 | 985 | 877 | 989 | 4735 | |
Isolates
Data include a total of 4,735 Neisseria meningitidis strains that were received between 2006 and 2010 at the NRLs from the aforementioned countries [28], [29], [30], [31], [32]. Isolates came from national hospitals whose type and distribution varies across countries, but there is a predominance of pædiatric hospitals belonging to the public health sector, although adult population are also attended in many centers and some countries receive isolates also from the private sector. Isolates were obtained from CSF (71.4%), blood (28.0%), and other sterile body fluids (0.6%), and information on gender, age, clinical presentation of the disease, serogroup and antibiotic resistance pattern was available. A total of 3,081 (65.1%) isolates were reported from Brazil alone. Argentina reported 591 (12.5%) isolates, and 326 (6.9%) came from Chile. Uruguay, Colombia and Venezuela reported 160 (3.4%), 124 (2.6%) and 111 (2.3%) respectively. All other countries reported under 100 isolates each (Table 1).
Laboratory Procedures
N. meningitidis isolates received at the NRLs were processed for ascertainment of species identification, serogrouping and determination of Minimum Inhibitory Concentration (MIC) to antibiotics [35]. Determinations were performed by agar dilution when possible [36], or using the gradient diffusion method (e.g. Etest, AB Biodisk®) following the manufactureŕs instructions. Results were interpreted according to the MENSURA group [37].
Quality Assurance
Quality and reliability of data are guaranteed through a comprehensive quality control and assurance assessment that is carried out by the IAL. The program was originally developed for S. pneumoniae and later extended to H. influenzae and N. meningitidis. Twice a year, five meningococcal test strains are distributed among the SIREVA II network participating laboratories, which will perform the necessary tests for species identification, phenotypic characterization (serogroup, serotype and serosubtype) and antibiotic susceptibility testing. A report is issued twice a year with the results for all countries, so corrective measures can be implemented if needed. A similar test is carried out on the IAL by ISCIII. External quality assurance is carried out twice a year, when the NRLs send their strains to the IAL for confirmation [34].
Statistical Analyses
Proportions were compared using Chi-Square test or Fisheŕs exact tests as appropriate. All analyses were performed using Stata/SE 11 for Windows.
Results
Clinical Origin of Isolates
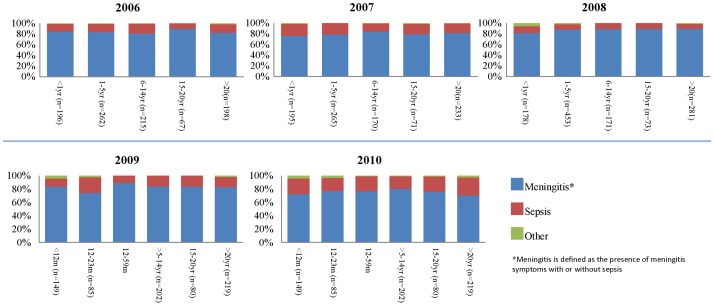
Around 80% of isolates were obtained from patients with meningitis in all study years (Figure 1). Approximately 20% of isolates came from patients presenting sepsis without meningitis, and around 1% of strains were isolated from cases of forms of invasive disease. Data did not specify what type of disease, with the exception of pneumonia cases, of which there were three in 2006, one in Argentina and two in Ecuador, and another three in 2007: in Chile, Ecuador and Paraguay respectively.
Figure 1. Meningococal disease presentation in Latin America and the Caribbean, 2006–2010.
*Meningitis is defined as the presence of meningitis symptoms with or without sepsis.
Isolates Reported by Age Group and Region
Data on age distribution of meningococcal disease isolates is shown in Tables 2 and 3, reflecting changes on the age-distribution data reporting introduced in 2009.
Table 2. Age distribution by region, 2006–2008.
| Region | 2006 | 2007 | 2008 | ||||||||||||
| <1 yr | 1–5 yrs | 6–14 yrs | 15–20 yrs | >20 yrs | <1 yr | 1–5 yrs | 6–14 yrs | 15–20 yrs | >20 yrs | <1 yr | 1–5 yrs | 6–14 yrs | 15–20 yrs | >20 yrs | |
| Brazil | 98 (15.6%) | 194 (30.8%) | 153 (24.3%) | 53 (8.4%) | 132 (21.0%) | 95 (16.9%) | 164 (29.1%) | 121 (21.5%) | 43 (7.7%) | 140 (24.9%) | 79 (12.7%) | 178 (28.6%) | 121(19.4%) | 52 (8.3%) | 193 (31.0%) |
| Southern cone | 62 (32.4%) | 55 (28.8%) | 33 (17.3%) | 4 (2.1%) | 37 (19.4%) | 70 (26.6%) | 85 (32.3%) | 34 (12.9%) | 14 (5.4%) | 60 (22.8%) | 71 (29.5%) | 76 (31.5%) | 29 (12.0%) | 12 (5.0%) | 53 (22.0%) |
| Andean Region | 19 (35.2%) | 6 (11.1%) | 6 (11.7%) | 6 (11.7%) | 17 (31.5%) | 24 (33.3%) | 10 (13.9%) | 11 (15.3%) | 7 (9.7%) | 20 (27.8%) | 13 (22.8%) | 10 (17.5%) | 9 (15.8%) | 2 (3.5%) | 23 (40.4%) |
| Mexico, Central America & Caribbean | 15 (21.1%) | 14 (19.7%) | 24 (33.8%) | 3 (4.2%) | 15 (21.1%) | 10 (19.6%) | 11 (21.6%) | 12 (23.5%) | 5 (9.8%) | 13 (25.5%) | 13 (20.3%) | 12 (18.8%) | 11(17.2%) | 7 (10.9%) | 21 (32.8%) |
| Total | 194 (20.5%) | 269 (28.4%) | 216 (22.8%) | 66 (7.0%) | 201 (21.2%) | 199 (21.0%) | 270 (28.5%) | 178 (18.8%) | 69 (7.3%) | 233 (24.6%) | 176 (17.9%) | 276 (28.0%) | 170 (17.3%) | 73 (7.4%) | 290 (29.4%) |
Table 3. Age distribution by region, 2009–2010.
| Region | 2009 | 2010 | ||||||||||
| <12 months | 12–23 months | 24–59 months | ≥5–14 years | 15–20 years | >20 years | <12 months | 12–23 months | 24–59 months | ≥5–14 years | 15–20 years | >20 years | |
| Brazil | 73 (12.5%) | 50 (8.6%) | 93 (16.0%) | 152 (26.1%) | 59 (10.1%) | 155 (26.6%) | 81 (12.3%) | 40 (6.2%) | 83 (12.9%) | 169 (26.2%) | 82 (12.7%) | 190 (29.5%) |
| Southern cone | 63 (28.3%) | 30 (13.5%) | 27 (12.1%) | 41 (18.4%) | 11 (4.9%) | 51 (22.9%) | 69 (32.4%) | 19 (9.1%) | 27 (12.7%) | 41 (19.2%) | 9 (4.2%) | 48 (22.5%) |
| Andean Region | 12 (31.6) | 2 (5.3%) | 2 (5.3%) | 5 (13.2%) | 5 (13.2%) | 12 (31.6) | 10 (27.0%) | 0 | 8 (21.6%) | 10 (27.0%) | 3 (8.1%) | 6 (16.2%) |
| Mexico, Central America & Caribbean | 7 (20.6%) | 4 (11.8%) | 2 (5.9%) | 6 (17.6%) | 11 (32.4%) | 4 (11.8%) | 8 (16.3%) | 3 (6.1%) | 10 (20.4%) | 12 (24.5%) | 5 (10.2%) | 11 (22.4%) |
| Total | 155 (17.7%) | 86 (9.8%) | 124 (14.1%) | 204 (23.3%) | 86 (9.8%) | 222 (25.3%) | 168 (17.8%) | 62 (6.6%) | 128 (13.6%) | 232 (24.6%) | 99 (10.5%) | 255 (27.0%) |
From 2006 to 2008, isolates obtained from cases on patients aged up to 5 years were consistently the most frequent on the five-year period in Brazil and in the Southern cone region. Brazilian isolates obtained from patients <1 year represented 12.7%, and in the Southern cone isolates from patients <1 year surpassed 30% in most years. A total of 185 (29.4%) isolates were obtained from patients aged 15 and over in Brazil during 2006, and that percentage increased steadily over the following years amidst an outbreak of serogroup C disease in recent years affecting older-age groups in some states in the country. In the Southern cone region, the yearly percentages of isolates obtained from this age-group remained stable.
In the Andean region, the highest percentage of isolates obtained from patients below the age of 5 was seen in 2007, with a total of 34 (47.2%) and 33.3% of them belonging to patients <1 year. Isolates on patients aged 15 and over represented 37.5% of the total in the same year.
In the Mexico, Central America and Caribbean region the percentage of cases among patients aged 5 or less were 40.8%, 34.7% and 38.7% in 2006, 2007 and 2008 respectively, with 21.1%, 16.3% and 21% of cases occurring among those <1 year.
The same trends were observed in all four regions for the period 2009–2010 (Table 3), with a high percentage of isolates coming from older patients in Brazil, and most isolates being obtained from young children, and particularly those <12 months in the Southern cone, Andean and Mexico, Central America & CAREC regions.
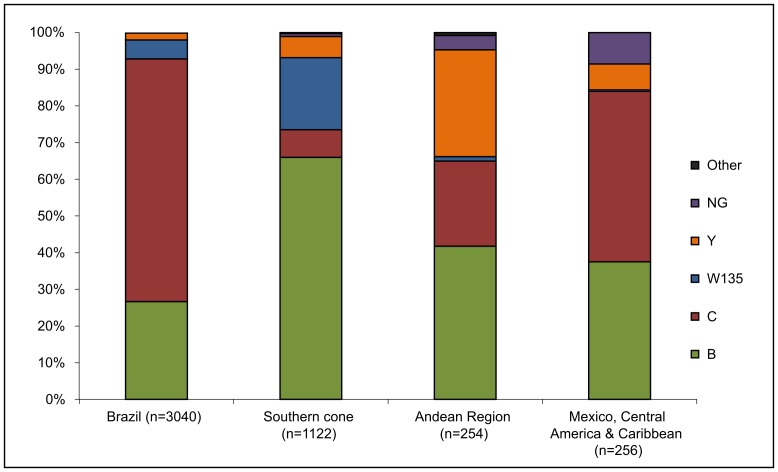
Serogroup Distribution by Regions and Countries
Serogroup distribution (Figure 2) was highly variable among countries for the period 2006–2010, which is consistent with what was seen in previous years since Neisseria meningitidis surveillance began in 2000 [20]. Sixty-six percent of meningococcal isolates characterized at the Brazil NLR for the period 2006–2010 belonged to serogroup C, and 26.7% were serogroup B. Serogroups W135 and Y represented 5.2 and 1.9% of isolates respectively. Conversely, 66% of all isolates characterized at the NRLs in the Southern cone region belonged to serogroup B, and 7.6% were serogroup C. Serogroup W135 was detected in 19.6% of isolates, and serogroup Y represented 5.8%.
Figure 2. Serogroup distribution, by region for the 2006–2010 period.
In the Andean region, serogroups B and Y were the most predominant, representing 41.7% and 29.1% respectively. Serogroup W135 accounted for 1.2% of isolates and 23.3% were serogroup C. Serogroup C was the most predominant serogroup among countries located in the Mexico, Central America & Caribbean region (46.5% of all isolates). Serogroup B was found in 37.5% of the isolates, and serogroups W135 and Y were 0.4% and 7% respectively.
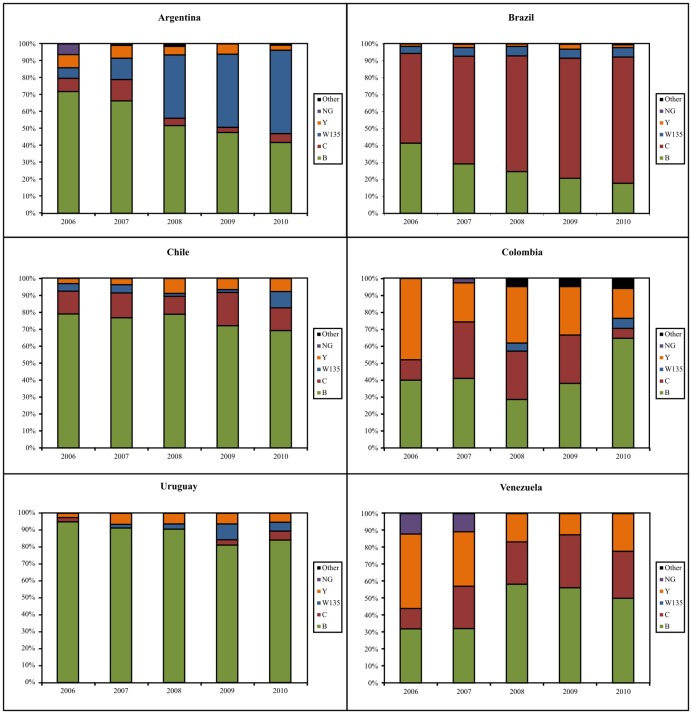
Figure 3 shows serogroup distribution among those countries that have reported at least 100 meningococcal isolates for the study period. In Argentina, serogroup B isolates represented 71.9% of all characterized isolates in 2006, whereas these isolates made up to 41.8% in 2010 (p>0.0001). Similarly, serogroup C halved its prevalence, from 7.8% in 2006 to 3% in 2009, but it was higher again in 2010, when it was found in 5.22% of isolates (p = 0.018). The biggest change was noticed in the proportion of isolates belonging to serogroup W135, which represented 6.3% of isolates in 2006 but accounted for almost half the isolates received by the NRL from 2008 onwards.
Figure 3. Serogroup distribution by year for Argentina Brazil, Chile, Uruguay and Venezuela.
*Selected countries are those for which >100 isolates were available.
In Brazil, serogroup C has experienced an important and progressive increase since the year 2000 [20], [28], [30], [31], [38] and accounted for over 74% of isolates characterized 2010 (p<0.0001). Conversely, serogroup B disease represented over 70% of isolates in 2000, but it was only found in 17.7% of them in 2010 (p<0.0001). Serogroups W135 and Y remained more or less stable since 2006 at around 5% and 2% respectively.
Serogroup B has been consistently the causative serogroup of over 80% of cases in Chile since data reporting to SIREVA II began in 2000. Serogroup C remains the second cause of disease and represents between 10–15% of the total. Serogroup W135 accounted for 9.6% of all isolates received in 2010, and serogroup Y isolates doubled their prevalence during the study period. None of these changes were statistically significant.
Serogroup B was present in over 90% of isolates received at the Uruguayan NRL consistently for the entire study period, and other serogroups were rare. In Colombia, serogroup B isolates were the most frequently received by the NRL. An important increase in serogroup Y has been noticed and reported in recent years but our data show that this trend is not sustained over time [39].
Serogroup W135 disease has not been detected in Venezuela, but serogroup Y isolates have been received occasionally by the NRL since surveillance started in 2000 [20]. The percentage of cases caused by this serogroup peaked in 2006, accounting for 44% of the total isolates characterized. Serogroup B isolates accounted for 32% of all meningococcal isolates processed at the NRL in 2006 and 2007, but it became over 50% on the three following years. Serogroup C isolates, however, remained at around 25% of isolates over the 5 years period.
Serogroup Distribution by Age Group
Serogroup distribution by age for the period 2006–2010 can be seen in Tables 4 and 5. Serogroup B isolates were consistently the most frequently obtained among those that came from patients aged >5 years in the LAC region. Serogroup C isolates, however appeared to be more prevalent among those coming from older patients and, particularly, among teenagers and adults. Similarly, serogroups W135 and Y were also associated with older age, but from 2008 onwards the number of W135 isolates obtained from young children was noticeably higher.
Table 4. Serogroup distribution by age, 2006–2008.
| Age | 2006 | 2007 | 2008 | |||||||||||||||
| B | C | W135 | Y | NG | Other | B | C | W135 | Y | NG | Other* | B | C | W135 | Y | NG | Other | |
| <1 | 91 (48.4%) | 72 (38.3%) | 7 (3.7%) | 11(5.9%) | 7 (3.7%) | 0 | 107 (65.2%) | 27 (16.5%) | 14 (8.5%) | 14 (8.5%) | 2 (1.2%) | 0 | 90 (51.4%) | 56 (32%) | 22 (12.6%) | 6 (3.4%) | 0 | 1(0.6%) |
| 1–5 | 125 (49.8%) | 102 (40.6%) | 12 (4.8%) | 7 (2.8%) | 5 (2.0%) | 0 | 126 (46.7%) | 119 (44.1%) | 13 (4.8%) | 6 (2.2%) | 6 (2.2%) | 0 | 103 (37.8%) | 135 (49.4%) | 24 (8.8%) | 8 (2.9%) | 3 (1.1%) | 0 |
| 6–14 | 101(47.4%) | 95 (44.6%) | 5 (2.3%) | 7 (3.3%) | 5 (2.3%) | 0 | 67 (37.9%) | 92 (51.9%) | 5 (2.8%) | 8 (4.5%) | 5 (2.8%) | 0 | 56 (33.1%) | 92 (54.4%) | 12 (7.1%) | 9 (5.3%) | 0 | 0 |
| 15–20 | 28 (42.4%) | 27 (40.9%) | 4 (6.1%) | 7 (10.6%) | 0 | 0 | 22 (32.8%) | 35 (52.2%) | 3 (4.5) | 7 (10.4%) | 0 | 0 | 23 (29.15) | 42 (53.2%) | 6 (7.6%) | 5 (6.3%) | 3 (3.8%) | 0 |
| >20 | 96 (47.8%) | 80 (39.8%) | 7 (3.5%) | 17 (8.4%) | 1 (0.5%) | 0 | 76 (32.9%) | 119 (51.5%) | 15 (6.5%) | 19 (8.2%) | 1(0.4%) | 1 (0.4%) | 71 (25.4%) | 160 (57.1%) | 29 (10.4%) | 19 (6.8%) | 0 | 1 (0.4%) |
| Total | 540 | 376 | 37 | 45 | 19 | 0 | 398 | 392 | 442 | 54 | 14 | 1 | 343 | 485 | 93 | 39 | 6 | 2 |
Table 5. Serogroup distribution by age, 2009–2010.
| Age | 2009 | 2010 | ||||||||||
| B | C | W135 | Y | NG | Other* | B | C | W135 | Y | NG | Other* | |
| <12 months | 70 (45.2%) | 50 (32.3%) | 27 (17.4%) | 7 (4.5%) | 0 | 1(0.6%) | 62 (36.9%) | 61 (36.3%) | 40 (23.9%) | 5 (3.0%) | 0 | 0 |
| 12–23 months | 37(43.0%) | 36 (41.9%) | 9 (10.5%) | 4 (4.7%) | 0 | 0 | 23 (37.1%) | 30 (48.4%) | 5 (8.1%) | 4 (6.5%) | 0 | 0 |
| 24–59 months | 48 (39.0%) | 68 (55.3%) | 5 (4.5%) | 2 (1.6%) | 0 | 0 | 52 (40.6%) | 68 (53.1%) | 4 (3.1%) | 2 (1.6%) | 1 (0.8%) | 1 (0.8%) |
| ≥5–14 years | 57 (27,8%) | 127 (62.0%) | 16 (7.8%) | 5 (2.4%) | 0 | 0 | 64 (27.6%) | 145 (62.5%) | 18 (7.9%) | 4 (1.7%) | 1 (0.4%) | 0 |
| 15–20 years | 19 (24.1%) | 47 (59.5%) | 9 (11.4%) | 4 (5.1%) | 0 | 0 | 15 (15.2%) | 70 (70.7%) | 11 (11.1%) | 3 (3.0%) | 0 | 0 |
| >20 years | 50 (22.0%) | 132 (58.1%) | 27 (11.9%) | 17 (7.5%) | 0 | 1 (0.4%) | 51 (20.0%) | 155 (60.8%) | 32 (12.5%) | 12 (4.7%) | 1 (0.4%) | 4 (1.6%) |
| Total | 281 | 460 | 93 | 39 | 0 | 2 | 267 | 529 | 110 | 30 | 3 | 5 |
Serogroup B isolates lowered from 53.1% of all processed isolates in 2006, to 28.3% in 2010 (p<0.0001). Serogroup C isolates varied over the five-years period, but continued to represent around 50% of all those received by the NRLs. Serogroup W135 was found in 3.6% of all isolates received by the NRLs isolates in 2006, but it represented a much higher proportion in 2007, when it was present in 34% of isolates. In 2010, serogroup W135 was detected in 11.7% of isolates in 2010 (p<0.0001).
Data on serogroup distribution by age and regions is submitted as supplementary data (Tables S1 and S2). A decrease in serogroup B across all age groups was noticed in Brazil during the 2006–2008 period, which was accompanied by an increase in serogroup C that was specially marked among older patients. Serogroup C became less prevalent among isolates obtained in the Southern cone region. This serogroup remained generally very low among patients in the <1 year and 1–5 year groups (4–6%), and was more frequent isolated among older patients, representing around 15% of isolates obtained from those aged 6–14, 15–20 and >20 years.
An increase on the percentage of isolates belonging to serogroup W135 was noticed in the Southern cone region across all age groups. In the Andean region, serogroup B represented 16.7% of isolates obtained from those aged 6–14 years in 2006, but it became 44.4% in 2008. An increase on serogroup Y isolates was seen among all age groups.
For the period 2009–2010, serogroup B remained stable in Brazil in all age-groups with the exception of the 15–20 years, among whom changed from 23.7% to 13.4%. Serogroup C went from 62.0% to 70.0% among those aged 12–23 months, and from 67.8% to 79.3% among the 15–20 years group. In the Southern cone region, the proportion of serogroup B isolates among those aged <12 months was 60.3% in 2009, and 47.8% in 2010. Among those in the 24–59 months group, the percentages in 2009 and 2010 were 81.5% and 66.7% respectively, and, 37.7% and 45.7% among the >20 years. Serogroup W135 was found to increase from 2009 to 2010 among adults >20 years, from 29.4% in 2009 to 41.3% in 2010.
Antibiotic Susceptibility
Minimum inhibitory concentration to penicillin, rifampin and chloramphenicol were determined either at the NRLs of participating countries, or at the RRLs in Brazil. Overall, 70.3% of all isolates were fully susceptible to penicillin, and 29.1% presented an intermediate resistance to this drug. A small decrease in the percentage of isolates with intermediate resistance to penicillin was noticed over the five-year period, as well as in comparison to published data from 2000–2005 [20]. Five fully-resistant isolates were found in 2006: four in Uruguay and one in Mexico. The 14 penicillin-resistant isolates reported in 2010 were found in Mexico, and all but one were isolated from cases of meningococcal disease occurred in penitentiary enclosure.
Isolates remained highly susceptible to rifampin. Intermediately-resistant isolates were rare (0.2%), and only 2 resistant isolates were detected: one in Brazil in 2006 and one in Argentina in 2009. Two rifampin resistant isolates reported in 2010 were isolated in Uruguay. Clinical and epidemiological data has been reported elsewhere [40].
Almost all isolates tested were resistant to chloramphenicol (data not shown) One isolate from Ecuador presented intermediate resistance to this drug, and one fully-resistant isolate was detected in Brazil in 2009.
Tables 6, 7, 8 and 9 show antibiotic resistance data by geographic regions. In Brazil, 14.5% of isolates characterized between 2006–2010 presented intermediate resistance to penicillin, and no fully resistant isolates were found. Over 99% of isolates were susceptible to rifampin, and intermediate and resistant isolates remained rare in Brazil.
Table 6. Susceptibility to penicillin and rifampin by year-Brazil.
| Year | PENICILIN | RIFAMPICIN | ||||
| Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | |
| 2006 | 168 (80.8%) | 40 (19.2%) | 0 | 207 (99.5%) | 0 | 1(0.5%) |
| 2007 | 293 (89.9%) | 33 (10.1%) | 0 | 326 (100%) | 0 | 0 |
| 2008 | 432 (84.4%) | 80 (15.65) | 0 | 511 (100%) | 0 | 0 |
| 2009 | 368 (83.6%) | 72 (16.4%) | 0 | 440 (100%) | 0 | 0 |
| 2010 | 442 (87.4%) | 64 (12.6%) | 0 | 502 (99.2%) | 3 (0.6%) | 1 (0.2%) |
| Total | 1703 (85.5%) | 289 (14.45%) | 0 | 1986 (99.7%) | 3 (0.2%) | 2 (0.1%) |
Brazil tests a random selection of isolates (67% in this study). Calculations take into account the percentage of penicillin intermediate-resistance as on the previous year.
Table 7. Susceptibility to penicillin and rifampin by year-Southern cone.
| Year | PENICILIN | RIFAMPICIN | ||||
| Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | |
| 2006 | 49 (27.8%) | 123 (69.9%) | 4 (2.3%) | 176 (100%) | 0 | 0 |
| 2007 | 71 (28.9%) | 175 (71.1%) | 0 | 237 (99.6%) | 1 (0.4%) | 0 |
| 2008 | 100 (42.0%) | 137 (57.6%) | 1 (0.4%) | 238 (100%) | 0 | 0 |
| 2009 | 110 (51.6%) | 103 (48.4%) | 0 | 204 (99.5%) | 0 | 1 (0.5%) |
| 2010 | 108 (50.7%) | 105 (49.3%) | 0 | 204 (99.0%) | 0 | 2 (1.0%) |
| Total | 438 (40.3%) | 643 (59.2%) | 5 (0.5%) | 1059 (99.6%) | 1 (0.1%) | 3 (0.3%) |
Table 8. Susceptibility to penicillin and rifampin by year-Andean region.
| Year | PENICILIN | RIFAMPICIN | ||||
| Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | |
| 2006 | 52 (92.9%) | 4 (7.1%) | 0 | 55 (98.2%) | 1 (1.8%) | 0 |
| 2007 | 36 (92.3%) | 3 (7.7%) | 0 | 39 (100%) | 0 | 0 |
| 2008 | 26 (81.3%) | 5 (15.6%) | 1 (3.1%) | 31 (100%) | 0 | 0 |
| 2009 | 27 (75.0%) | 9 (25.0%) | 0 | 35 (100%) | 0 | 0 |
| 2010 | 19 (63.3%) | 10 (33.3%) | 1 (3.4%) | 30 (100%) | 0 | 0 |
| Total | 160 (82.9%) | 31(16.1%) | 2 (1.0%) | 190 (99.5%) | 1 (0.5%) | |
Table 9. Susceptibility to penicillin and rifampin by year-Mexico, Central America & Caribbean.
| Year | PENICILIN | RIFAMPICIN | ||||
| Susceptible | Intermediate | Resistant | Susceptible | Intermediate | Resistant | |
| 2006 | 32 (68.1%) | 14 (29.8%) | 1 (2.1%) | 22 (100%) | 0 | 0 |
| 2007 | 22 (68.8%) | 10 (31.2%) | 0 | 17 (100%) | 0 | 0 |
| 2008 | 40 (87.0%) | 6 (13.0%) | 0 | 36 (100%) | 0 | 0 |
| 2009 | 13 (76.5%) | 4 (23.5%) | 0 | 11 (84.6%) | 2 (15.4%) | 0 |
| 2010 | 16 (43.2%) | 6 (16.2%) | 15 (40.6%) | 27 (100%) | 0 | 0 |
| Total | 123 (68.7%) | 40 (22.3%) | 16 (8.9%) | 113 (98.3%) | 2 (1.7%) | |
A total of 643 (59.2%) of isolates characterized in the Southern cone region presented intermediate resistance to penicillin, and fully-resistant isolates were also present (four in Uruguay in 2006 and one in Paraguay in 2008) although their overall prevalence was below 1%. Isolates from this region remained susceptible to rifampin, with intermediate and fully resistant isolates being representing 0.1 and 0.3% of isolates respectively.
The Andean Region presented similar percentages of susceptibility to those seen in Brazil. However, the percentage of isolates presenting intermediate resistance to penicillin increased noticeably from 2008 onwards.
In the Mexico, Central America and CAREC, an overall of 68.7% of isolates were fully susceptible to penicillin, and 22.3% presented intermediate resistance to this antibiotic. In 2010, 14 fully penicillin resistant isolates were found in Mexico, all associated to an outbreak of disease in a prison. With the exception of these isolates, penicillin resistance also remained rare in this region.
Discussion
Neisseria meningitidis is presumed to be a leading cause of invasive bacterial disease in Latin America, as the implementation of the Hib-conjugate vaccine has substantially reduced the burden of disease caused by this bacterium [19], [41]–[44]. But to date, very few countries in the region have a well-established surveillance for IMD so no data on the true burden of disease is available. All available laboratory data has been generated through the SIREVA II network, which is coordinated by PAHO [20], [28], [30], [31], [38]. Despite many improvements over the years, quality of both epidemiological and laboratory information is not equal among all participating countries. Specifically, the recovery of Neisseria meningitidis is particularly challenging for a number of reasons; empiric antibiotic therapy is often administered prior to sample collection, which prevents the isolation of the bacterium in culture. Delays in sample processing sometimes result in the bacterium being detected by indirect methods such as Gram-stain or latex-agglutination, but not recovered in culture. In many low-income countries, peripheral laboratories lack the infrastructure and resources to allow them to process samples correctly, which results in bacteria being neither detected nor isolated from biological samples. Data presented here was obtained solely from information on the number of strains processed by NRLs and reported to the SIREVA II network, so with a few exceptions, they are not representative of the epidemiology and strain characteristics of IMD in individual countries, but show trends of what has taken place in the region over the past five years. It is worth pointing out that countries such as Argentina, Brazil or Chile, with well-established surveillance system, report to receive isolates from approximately 50 to 60% of all reported cases any given year, whereas Uruguay, which also has a good performing surveillance receives nearly all isolates obtained in the country. But countries such as those located in the Mexico, Central America and Caribbean region and in the Andean region are unlikely to receive any percentage of isolates that could suffice to draw any conclusions regarding the epidemiology or circulating strains in these countries.
Based on the data collected by the NRL in Latin America, IMD in appears to occur mainly in children under the age of 5. However, a substantial number of isolates processed by the NRLs participating in the SIREVA II network were obtained from patients over 20 years of age. Although this could indicate that the number of disease cases among adult patients is unusually high, especially as this trend appears to be sustained over time and also evidenced in countries where clinical management guidelines are well established, such as Brazil or Argentina, further investigations are needed to determine whether and which operational factors could account for this phenomenon in each of the countries. Additionally, the implementation of an active surveillance in a well-defined population including both pædiatric and adults hospitals is needed to confirm this trend. Carriage studies in the region could be of use in providing indirect evidence. In high and medium-income countries, asymptomatic carriage of Neisseria meningitidis peaks among adolescents and decreases progressively in adulthood, making disease less likely [45], [46], [47]. Data on the distribution of IMD from Latin America and Caribbean countries could suggests distribution of carriage rates across age groups might differ from those reported from Europe and the US, at least in those where environmental and socio-economic factors make living conditions not comparable to those in other continents. A study performed in Uruguay in 1998 found carriage rates of 41.5% among adults aged 21–30 years, and 19.5% on the 31–40 years age range, which differ from findings elsewhere [48]. However, studies from Cuba [49] and Brazil have shown trends and carriage rates similar to those reported elsewhere [47], [50], [51]. It would therefore be advised that asymptomatic carriage studies are carried out in the region before any vaccination strategy is considered, as the adult group might need to be taken into consideration in some countries if transmission of invasive strains is to be stopped by, for instance, the implementation of a catch-up campaign similar to that carried out in the United Kingdom in addition to the introduction of the vaccine in the national immunization scheme [52].
Serogroup distribution varied widely among the four regions in which countries were divided. Serogroup C was the major cause of disease in Brazil, where a sustained epidemic of serogroup C disease in some states prompted the health authorities to introduce the serogroup C conjugate vaccine in the infant vaccination schedule in October 2010, while changes induced by this public health intervention are being monitored closely [19]. As serogroup C accounted for over 90% of all vaccine-preventable isolates, it is expected that the implementation of the vaccine will substantially reduce the overall burden of disease in the country. In the Southern cone region serogroup C isolates represented less than 10% of those processed by the NRLs, with serogroup B being the major cause of MD. A substantial increase of serogroup W135 was noticed among countries in this region in recent years, especially in Argentina. Brazil reported also an increase on the number of cases of W135 disease in two states: Rio de Janeiro and Rio Grande do Sul. In both cases, the causing strain was found to be that linked to the 2000 Hajj global outbreak [53], [54]. Data presented in this article appear to indicate that serogroup W135 is more often seen among isolates obtained from older patients. It is widely accepted that an age-shift towards older patients occurs in hyper-endemic and epidemic situations [55], [56], which can occur when a new strain is introduced into the population as no immunity has been generated against it [57], [58].
Data on serogroup distribution from the Andean Region and from the Mexico, Central America and CAREC is not representative of the regions, as virtually all data comes from Colombia and Venezuela in the first case and from Mexico, Dominican Republic and Panama on the second case. This was expected as some of the lowest income countries in Latin America are grouped within these two regions.
Analysis of data from Argentina, Brazil, Chile, Colombia, Uruguay and Venezuela highlight variations in the epidemiology of the disease among individual countries. Although all four of the major disease-causing serogroups, B, C, W135 and Y are present across the region, data suggest that recommendations regarding public health interventions to control IMD will need to be carefully evaluated in each country. However, countries grouped in the Southern cone region (Argentina, Chile and Uruguay) all present a similar pattern of serogroup distribution, with high prevalence of serogroup B disease, low number of serogroups C and a recent increase in W135 isolates. Similarly, Colombia and Venezuela, which are both grouped in the Andean region, also share the pattern, with serogroups B and C being both a major cause of disease, and high percentages of serogroup Y compared to other countries in the region. This serogroup was reported to have increased significantly in Colombia since 2003 onwards [39] but our data suggest that this trend might be reverting. A previously published study on the molecular characteristics of serogroup Y isolates found in Latin America showed that the strains circulating in Colombia are not different from those found in Argentina, Brazil, Chile or Costa Rica and hence this apparently unusual situation could not be attributed to the presence of a particularly virulent strain in Colombia [59]. Our data does not suggest that serogroup Y is replacing any of the previously circulating serogroups but rather that there is a higher circulation of this serogroup among the Colombian and Venezuelan populations. Serogroup Y strains are also present in Ecuador, also grouped in the Andean region, and its presence in other surrounding countries could not be ruled out. Close monitoring of disease-causing strains, and particularly of serogroup Y in all countries in the Andean region should be maintained.
Although the number of isolates analyzed from countries grouped in the Mexico, Central America and Caribbean region is not enough to discern a common pattern of major disease-causing serogroups, based on results from the other two major regions, data suggest that some geographic structuring is present among the four regions in which the data has been grouped. This finding could have implications to those countries experiencing difficulties to isolate meningococcus in their laboratories, as they could infer the epidemiology of meningococcal disease based on findings from neighboring countries, notwithstanding the necessity of taking steps to improve their surveillance systems and laboratory capacities to generate their own data.
The number of isolates reported from many of the countries has experienced an important decline, especially when all data collected on the 2000–2005 period are taken into consideration [20]. Evidence points at this decline being caused by the cyclical nature of meningococcal disease outbreaks, which is characterized by waves of progressive increased incidence rates followed by an equally progressive decrease that can last for decades [18], [60], [61].
In many Latin American countries a decline on disease incidence rates that is consistent with this observation has also been noticed [62]–[65]. One explanation for this could be the widespread practice of administering antibiotics prior to LP, which is very common in the region and results in IMD cases being reported as unknown ætiology when reported at all. However, the cyclical nature of meningococcal disease could also provide an explanation for this and if so, increases in the number of isolates reported through the SIREVA II network as well as in disease incidence are to be expected in the future.
All Neisseria meningitidis strains for which antibiotic susceptibility was tested remained highly sensitive to rifampin and chloramphenicol. However, the presence of sporadic cases caused by rifampin-resistant strains evidences the need to maintain systematic monitoring of resistance to this drug, as it is still the first choice as prophylaxis for case contacts in many countries in the region.
Decreased sensitivity to penicillin was found in around 30% of isolates. Special attention should be paid in the Southern cone region, where isolates presenting intermediate resistance to penicillin represented almost 60% of all characterized isolates. A number of studies have shown that the infection with a such strains is not associated with a fatal outcome [66], [67], [68], as the drug remains effective for the treatment of IMD. But as the opposite has also been documented, it would be advisable that attention is paid by NRL and epidemiologist to the outcome of IMD cases from whom a strain with decreased susceptibility to penicillin is isolated in order to establish the clinical significance of such strains in the region. These results also highlight the necessity to maintain systematic surveillance of MICs to this drug, as well as the importance of standardizing protocols and unifying susceptibility reporting criteria so ensure data are comparable among countries in the region.
Fourteen penicillin-resistant isolates reported in 2010 belong to an outbreak occurred in a Mexican prison. The outbreak affected mainly inmates and some of their relatives, but at least one unrelated case of penicillin-resistant meningococcal disease was reported (Monica Viveros-Terrazas, personal communication). These results need to be considered with caution as confirmation from the RRL is still pending, but attention must be paid should they be confirmed, as the spread of fully-resistant strains in a region where penicillin is the first line of action when a case of acute bacterial meningitis is suspected could have fatal consequences for the patients.
In conclusion, laboratory data on meningococcal disease across the Latin American region evidences that disease surveillance needs to be improved, especially among countries located in the Mexico, Central America and Caribbean, and those in the Andean region. Information is urgently needed, as the use of either the already available meningococcal vaccines against serogroups A, C, W135 and Y or those that are to come covering serogroup B are likely to have a great impact in the epidemiology of IMD in the region.
The establishment of standardized case definitions and clear guidelines on when lumbar puncture or blood culture should be performed would ensure that cases of meningococcal disease are diagnosed, especially since new molecular diagnostic techniques are being incorporated into routine surveillance and making it possible to identify the causative pathogen even when very little quantities of bacterial DNA are present in the sample [69]. Epidemiological surveillance and report systems need to be carefully evaluated to ensure weaknesses at all levels are identified and addressed. It is of great importance that national health authorities adopt these guidelines into their national ones, and accept the need to obtain data of IMD in their countries if improvements are to be made. An active sentinel-site surveillance covering all age-groups and allowing the incorporation of population-based data would be strongly recommended, especially for those countries where IMD is rarely reported.
Harmonization of laboratory procedures is essential not only to ensure data are comparable among countries, but also to facilitate the identification and solution of any methodological problems that might arise. Peripheral laboratories need to be well equipped and supplied with all necessary reagents and quality controlled-culture media to ensure isolation of bacteria. Personnel in these laboratories should be enrolled in periodic trainings carried out at central level by the NRLs to ensure they can perform all laboratory procedures correctly. Additionally, NRLs need to ensure their staff are properly trained and encouraged to implement new emerging technologies. Implementation of molecular characterization techniques such as Multilocus Sequence Typing (MLST) as a routine in NRLs and RRLs would make data from Latin America comparable to that generated and published worldwide.
With the predicted arrival of new meningococcal vaccines and their potential introduction in Latin American countries, the implementation of measures to allow the generation of reliable data on disease burden and circulating strains in those countries where no information is available will be a major challenge in the upcoming years.
Supporting Information
Serogroup distribution by age and regions 2006–2008.
(XLSX)
Serogroup distribution by age and regions 2009–2010.
(XLSX)
Acknowledgments
The authors are grateful to the Canadian International Development Agency (CIDA) to their support to the SIREVA II network. They also want to extend their gratitude to all personnel working at sentinel and peripheral laboratories in participating countries, in national reference laboratories and, especially to the Instituto Adolfo Lutz in São Paulo, Brazil, Instituto Nacional de Salud, Colombia, and the Instituto de Salud Carlos III in Madrid, Spain for their contribution as regional and international reference laboratories.
Since 2010, meningococcal disease surveillance is supported by the Pan-American Health and Education Foundation (PAHEF). Finally, the authors wish to thank the Immunizations Project in the Family and Community Health Area (FCH/IM) in PAHO headquarters and country offices.
Contributors
Members of the SIREVA II study group are: Alejandra Corso, Paula Gagetti, Adriana Efron, Cecilia Sorohuet, Marilina Moscoloni (Instituto Nacional de Enfermedades Infecciosas Dr. Carlos G. Malbrán, Argentina); Patricia Rosales Rojas (Instituto Nacional de Laboratorios de Salud-Brasil, Bolivia); Maria Cristina de Cunto Brandileone (Instituto Adolfo Lutz, Bolivia); Aurora Maldonado, Soledad Prat, Mabel Seoane, Pamela Araya (Instituto de Salud Pública, Chile); Maria Elena Realpe, Olga Marina Sanabria, Carolina Duarte (Instituto Nacional de Salud, Colombia); Grettel Chanto Chacon (Centro Nacional de Referencia en Bacteriología, Costa Rica); Rafael Llanes, Gilda Toraño, Onelkis Feliciano, Oderay Gutiérrez (Instituto de Medicina Tropical Pedro Kourí, Cuba); Carmen Pesantes Almeida, Yolanda Narváez San Martín, Javier Sánchez Chóez (Instituto Nacional de Higiene y Medicina Tropical Leopoldo Izquieta-Perez, Ecuador); Zandra Jiménez de Fuentes (Ministerio de Salud Pública y Asistencia Social, El Salvador); Roxana Elizabeth Castillo (Laboratorio Nacional de Vigilancia, Dr. Alejandro Lara, Honduras); Mónica Viveros Terrazas (Instituto de Diagnóstico y Referencia Epidemiológicos, México); Gabriela Echániz-Avilés (Instituto Nacional de Salud Pública, México); María Javiera Mejía Sandino, Armengol Ortiz Gómez (Centro Nacional de Diagnóstico y Referencia, Nicaragua); Markela de Quinzada, Raquel de Bolaños, Marlenys Fernandez (Laboratorio Central de Referencia en Salud Pública. Instituto Conmemorativo Gorgas de Estudios de la Salud, Panamá); Gustavo Adolfo Chamorro Cortesi, Maria Eugenia León Ayala, Aníbal Kawabata (Laboratorio Central de Salud Pública, Paraguay); Sara Morales (Instituto Nacional de Salud, Perú); Jacqueline Sánchez, Milagro Peña (Hospital Infantil Dr. Roberto Reid Cabral, Dominican Republic); Michelle Nurse-Lucas, Lorraine Francis (Caribbean Epidemiology Centre, Trinidad & Tobago (CAREC)); Teresa Camou, Gabriel Pérez-Giffoni (Servicio Nacional de Laboratorios, Ministerio de Salud, Uruguay); Enza Spadola, Daisy Payares (Instituto Nacional de Higiene Rafael Rangel, Venezuela); Clara-Inés Agudelo, Elizabeth Castañeda (SIREVA II advisors).
Funding Statement
Funding to the SIREVA II network was provided by the Canadian International Development Agency (CIDA). Since 2010, funding for meningococcal disease surveillance in 2010 is provided by Sanofi-Pasteur through the Pan-American Health and Education Foundation (PAHEF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM (2001) Meningococcal disease. N Engl J Med 344: 1378–1388. [DOI] [PubMed] [Google Scholar]
- 2. Aguilar-Garcia J, Olalla-Sierra J, Perea-Milla E, Rivas-Ruiz F, Martos F, et al. (2009) Analysis of the epidemiological characteristics and prognostic factors in probable or confirmed invasive meningococcal disease in a cohort of adolescents and adults during an epidemic outbreak. Rev Clin Esp 209: 221–226. [PubMed] [Google Scholar]
- 3. Deghmane AE, Parent du Chatelet I, Szatanik M, Hong E, Ruckly C, et al. (2010) Emergence of new virulent Neisseria meningitidis serogroup C sequence type 11 isolates in France. J Infect Dis 202: 247–250. [DOI] [PubMed] [Google Scholar]
- 4. Doyle TJ, Mejia-Echeverry A, Fiorella P, Leguen F, Livengood J, et al. (2009) Cluster of serogroup W135 meningococci, southeastern Florida, 2008–2009. Emerg Infect Dis 16: 113–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jardine A, Truman G, Sheppeard V, Gibbons D, Thomas J, et al. (2009) A community outbreak of meningococcal serogroup B disease in western Sydney: the challenges of identification and significance. Commun Dis Intell 33: 221–224. [PubMed] [Google Scholar]
- 6.Skoczynska A, Wasko I, Kuch A, Golebiewska A, Forys M, et al.. (2010) Outbreak of invasive meningococcal disease in Goleniow County, northwest Poland, March 2009. Euro Surveill 15. [PubMed]
- 7. Taylor-Robinson D, Elders K, Milton B, Thurston H (2010) Students' attitudes to the communications employed during an outbreak of meningococcal disease in a UK school: a qualitative study. J Public Health (Oxf) 32: 32–37. [DOI] [PubMed] [Google Scholar]
- 8. Weiss D, Stern EJ, Zimmerman C, Bregman B, Yeung A, et al. (2009) Epidemiologic investigation and targeted vaccination initiative in response to an outbreak of meningococcal disease among illicit drug users in Brooklyn, New York. Clin Infect Dis 48: 894–901. [DOI] [PubMed] [Google Scholar]
- 9. Harrison LH, Trotter CL, Ramsay ME (2009) Global epidemiology of meningococcal disease. Vaccine 27 Suppl 2B51–63. [DOI] [PubMed] [Google Scholar]
- 10.Lapeyssonnie L (1963) La méningite cérébrospinale en Afrique. Bull World Health Organ: 1–100. [PMC free article] [PubMed]
- 11. Greenwood B (1999) Manson Lecture. Meningococcal meningitis in Africa. Trans R Soc Trop Med Hyg 93: 341–353. [DOI] [PubMed] [Google Scholar]
- 12. Stephens DS, Greenwood B, Brandtzaeg P (2007) Epidemic meningitis, meningococcaemia, and Neisseria meningitidis. Lancet 369: 2196–2210. [DOI] [PubMed] [Google Scholar]
- 13.Lopez L, Sexton K, Carter P (2011) The epidemiology of meningococcal disease in New Zealand in 2010
- 14. Cano R, Larrauri A, Mateo S, Alcala B, Salcedo C, et al. (2004) Impact of the meningococcal C conjugate vaccine in Spain: an epidemiological and microbiological decision. Euro Surveill 9: 11–15. [PubMed] [Google Scholar]
- 15. Kafetzis DA, Stamboulidis KN, Tzanakaki G, Kourea Kremastinou J, Skevaki CL, et al. (2007) Meningococcal group C disease in Greece during 1993–2006: the impact of an unofficial single-dose vaccination scheme adopted by most paediatricians. Clin Microbiol Infect 13: 550–552. [DOI] [PubMed] [Google Scholar]
- 16.Salisbury D (2001) Introduction of a conjugate meningococcal type C vaccine programme in the UK. J Paediatr Child Health 37: S34–36; discussion 37. [DOI] [PubMed]
- 17. Stefanelli P, Fazio C, Sofia T, Neri A, Mastrantonio P (2009) Serogroup C meningococci in Italy in the era of conjugate menC vaccination. BMC Infect Dis 9: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harrison LH (2010) Epidemiological profile of meningococcal disease in the United States. Clin Infect Dis 50 Suppl 2S37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Safadi MA, Cintra OA (2010) Epidemiology of meningococcal disease in Latin America: current situation and opportunities for prevention. Neurol Res 32: 263–271. [DOI] [PubMed] [Google Scholar]
- 20. Gabastou JM, Agudelo CI, Brandileone MC, Castaneda E, de Lemos AP, et al. (2008) Characterization of invasive isolates of S. pneumoniae, H. influenzae, and N. meningitidis in Latin America and the Caribbean: SIREVA II, 2000–2005. Rev Panam Salud Publica 24: 1–15. [DOI] [PubMed] [Google Scholar]
- 21. Castaneda E, Agudelo CI, Regueira M, Corso A, Brandileone MC, et al. (2009) Laboratory-based surveillance of Streptococcus pneumoniae invasive disease in children in 10 Latin American countries: a SIREVA II project, 2000–2005. Pediatr Infect Dis J 28: e265–270. [DOI] [PubMed] [Google Scholar]
- 22. Di Fabio JL, Castaneda E, Agudelo CI, De La Hoz F, Hortal M, et al. (2001) Evolution of Streptococcus pneumoniae serotypes and penicillin susceptibility in Latin America, Sireva-Vigia Group, 1993 to 1999. PAHO Sireva-Vigia Study Group. Pan American Health Organization. Pediatr Infect Dis J 20: 959–967. [DOI] [PubMed] [Google Scholar]
- 23. Hortal M, Ruvinsky R, Rossi A, Agudelo CI, Castaneda E, et al. (2000) Impact of Streptococcus pneumoniae on pneumonia in Latin American children. SIREVA-Vigia Group. Rev Panam Salud Publica 8: 185–195. [DOI] [PubMed] [Google Scholar]
- 24. Perez Rodriguez A, Meneses FO (1999) VA-MENGOC-BC vaccine: its impact on meningococcal disease in children 1–4 years old. Rev Cubana Med Trop 51: 189–193. [PubMed] [Google Scholar]
- 25. Rodriguez AP, Dickinson F, Baly A, Martinez R (1999) The epidemiological impact of antimeningococcal B vaccination in Cuba. Mem Inst Oswaldo Cruz 94: 433–440. [DOI] [PubMed] [Google Scholar]
- 26. Sotolongo F, Campa C, Casanueva V, Fajardo EM, Cuevas IE, et al. (2008) Cuban Meningococcal BC Vaccine: Experiences & Contributions from 20 Years of Application. MEDICC Rev 9: 16–22. [DOI] [PubMed] [Google Scholar]
- 27.Ministerio da Saúde do Brasil website. Available: http://portal.saude.gov.br/portal/saude/profissional/area.cfm?id_area=1563. Accessed 2012 Aug 3.
- 28.OPS (2008) Informe regional de SIREVA II, 2007: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos. Washington D.C.: OPS. 273 p.
- 29.OPS (2008) Informe regional de SIREVA II, 2006: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos. Washington D.C.: OPS. 273 p.
- 30.OPS (2009) Informe regional de SIREVA II, 2008: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos. Washington D.C.: OPS. 273 p.
- 31.OPS (2010) Informe regional de SIREVA II, 2009: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos. Washington D.C.: OPS. 273 p.
- 32.OPS (2010) Informe regional de SIREVA II, 2010: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos. Washington D.C.: OPS. 273 p.
- 33. Di Fabio JL, Homma A, de Quadros C (1997) Pan American Health Organization epidemiological surveillance network for Streptococcus pneumoniae. Microb Drug Resist 3: 131–133. [DOI] [PubMed] [Google Scholar]
- 34. Lovgren M, Talbot JA, Brandileone MC, Casagrande ST, Agudelo CI, et al. (2007) Evolution of an international external quality assurance model to support laboratory investigation of Streptococcus pneumoniae, developed for the SIREVA project in Latin America, from 1993 to 2005. J Clin Microbiol 45: 3184–3190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popovic T, Ajello G, Facklam R (1998) Laboratory methods for the diagnosis of meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae and Haemophilus influenzae. Centers for Disease Control and Prevention and World Health Organization. 381 p.
- 36.Wikler ML, Low DE, Cockerill FR, Sheehan DJ, Craig WA, et al. (2006) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard-seventh edition. Available: http://www.clsi.org/source/orders/free/m11a7.pdf
- 37. Baquero F, Martinez-Beltran J, Canton R (1998) Criteria of the MENSURA group for the definition of the critical points of sensitivity to antibiotics. Enferm Infecc Microbiol Clin 16: 85–92. [PubMed] [Google Scholar]
- 38.OPS (2007) Informe regional de SIREVA II: datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus neumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasivos, 2000–2005. Washington D.C.: OPS. 387 p.
- 39. Ines Agudelo C, Sanabria OM, Ovalle MV (2008) Serogroup Y meningococcal disease, Colombia. Emerg Infect Dis 14: 990–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Perez Giffoni G, Garcia Gabarrot G, Alfonso A, Pujadas M, Camou T (2012) Detection of rifampicin-resistant strains of Neisseria meningitidis in Uruguay. Rev Panam Salud Publica 30: 540–544. [DOI] [PubMed] [Google Scholar]
- 41. Pan American Health Organization (1996) Impact of Uruguay's introduction of the Haemophilus influenzae type b (Hib) vaccine. EPI Newsl 18: 6. [PubMed] [Google Scholar]
- 42. Agudelo CI, Munoz N, De la Hoz F (2000) Rapid assessment of the impact of Haemophilus influenzae vaccine serotype b in Colombia. Public Health Laboratories. Rev Panam Salud Publica 8: 181–184. [DOI] [PubMed] [Google Scholar]
- 43. Diaz JM, Catalan L, Urrutia MT, Prado V, Ledermann W, et al. (2001) Trends of etiology of acute bacterial meningitis in Chilean children from 1989 to 1998. Impact of the anti-H influenzae type b vaccine. Rev Med Chil 129: 719–726. [PubMed] [Google Scholar]
- 44. Lagos R, Horwitz I, Toro J, San Martin O, Abrego P, et al. (1996) Large scale, postlicensure, selective vaccination of Chilean infants with PRP-T conjugate vaccine: practicality and effectiveness in preventing invasive Haemophilus influenzae type b infections. Pediatr Infect Dis J 15: 216–222. [DOI] [PubMed] [Google Scholar]
- 45.Broome CV (1986) The carrier state: Neisseria meningitidis. J Antimicrob Chemother 18 Suppl A: 25–34. [DOI] [PubMed]
- 46. Cartwright KA, Stuart JM, Jones DM, Noah ND (1987) The Stonehouse survey: nasopharyngeal carriage of meningococci and Neisseria lactamica. Epidemiol Infect 99: 591–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Claus H, Maiden MC, Wilson DJ, McCarthy ND, Jolley KA, et al. (2005) Genetic analysis of meningococci carried by children and young adults. J Infect Dis 191: 1263–1271. [DOI] [PubMed] [Google Scholar]
- 48.Parodi V, Allende F, Torres E, Mucedo M, Maglione R, et al.. (1998) Portadores de Neisseria meningitidis en una población de Montevideo. Revista medica uruguaya: 4.
- 49.Núñez N, Martinez I, Izquierdo L, Álvarez N, López O (2007) Portadores de Neisseria meningitidis y Neisseria lactamica en tres grupos de edades diferentes. VacciMonitor 16.
- 50. Jolley KA, Kalmusova J, Feil EJ, Gupta S, Musilek M, et al. (2000) Carried meningococci in the Czech Republic: a diverse recombining population. J Clin Microbiol 38: 4492–4498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ibarz-Pavon AB, Maclennan J, Andrews NJ, Gray SJ, Urwin R, et al. (2011) Changes in serogroup and genotype prevalence among carried meningococci in the United Kingdom during vaccine implementation. J Infect Dis 204: 1046–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Miller E, Salisbury D, Ramsay M (2001) Planning, registration, and implementation of an immunisation campaign against meningococcal serogroup C disease in the UK: a success story. Vaccine 20 Suppl 1S58–67. [DOI] [PubMed] [Google Scholar]
- 53. Weidlich L, Baethgen LF, Mayer LW, Moraes C, Klein CC, et al. (2008) High prevalence of Neisseria meningitidis hypervirulent lineages and emergence of W135:P1.5,2:ST-11 clone in Southern Brazil. J Infect 57: 324–331. [DOI] [PubMed] [Google Scholar]
- 54. Barroso DE, Rebelo MC (2007) Recognition of the epidemiological significance of Neisseria meningitidis capsular serogroup W135 in the Rio de Janeiro region, Brazil. Mem Inst Oswaldo Cruz 102: 773–775. [DOI] [PubMed] [Google Scholar]
- 55. Peltola H, Kataja JM, Makela PH (1982) Shift in the age-distribution of meningococcal disease as predictor of an epidemic? Lancet 2: 595–597. [DOI] [PubMed] [Google Scholar]
- 56. Kuzemenska P, Kriz B, Svandova E (1984) Meningococcal meningitis in CSR: a preepidemic situation? Zentralbl Bakteriol Mikrobiol Hyg A 257: 195–203. [PubMed] [Google Scholar]
- 57. McEllistrem MC, Kolano JA, Pass MA, Caugant DA, Mendelsohn AB, et al. (2004) Correlating epidemiologic trends with the genotypes causing meningococcal disease, Maryland. Emerg Infect Dis 10: 451–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Russell JE, Urwin R, Gray SJ, Fox AJ, Feavers IM, et al. (2008) Molecular epidemiology of meningococcal disease in England and Wales 1975–1995, before the introduction of serogroup C conjugate vaccines. Microbiology 154: 1170–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Abad R, Agudelo CI, Brandileone MC, Chanto G, Gabastou JM, et al. (2009) Molecular characterization of invasive serogroup Y Neisseria meningitidis strains isolated in the Latin America region. J Infect 59: 104–114. [DOI] [PubMed] [Google Scholar]
- 60.Cartwright K (1995) Meningococcal carriage and disease. In: Cartwright K, editor. Meningococcal disease. Chichester: John Wiley & Sons Ltd. 115–146.
- 61. Caugant DA, Maiden MC (2009) Meningococcal carriage and disease–population biology and evolution. Vaccine 27 Suppl 2B64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sorhouet Pereira C, Regueira M, Mollerach M (2008) PorA types in Neisseria meningitidis serogroup B isolated in Argentina from 2001 to 2003: implications for the design of an outer membrane protein-based vaccine. J Med Microbiol 57: 338–342. [DOI] [PubMed] [Google Scholar]
- 63.Ministerio de Salud de Chile website. Available: http://epi.minsal.cl/evigant/evganter.htm. Accessed 2012 Aug 3.
- 64.PAHO/WHO Colombia regional office website-Epidemiological bulletins. Available: http://www.col.ops-oms.org/sivigila/IndiceBoletines2003.asp. Accessed 2012 Aug 3.
- 65.Ministerio de Salud de Paraguay-Boletín epidemiológico. Available: http://www.vigisalud.gov.py/index.php?option=com_phocadownload&view=section&id=8&Itemid=128. Accessed 2012 Aug 3.
- 66. Brown EM, Fisman DN, Drews SJ, Dolman S, Rawte P, et al. (2010) Epidemiology of invasive meningococcal disease with decreased susceptibility to penicillin in Ontario, Canada, 2000 to 2006. Antimicrob Agents Chemother 54: 1016–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. du Plessis M, von Gottberg A, Cohen C, de Gouveia L, Klugman KP (2008) Neisseria meningitidis intermediately resistant to penicillin and causing invasive disease in South Africa in 2001 to 2005. J Clin Microbiol 46: 3208–3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Trotter CL, Fox AJ, Ramsay ME, Sadler F, Gray SJ, et al. (2002) Fatal outcome from meningococcal disease–an association with meningococcal phenotype but not with reduced susceptibility to benzylpenicillin. J Med Microbiol 51: 855–860. [DOI] [PubMed] [Google Scholar]
- 69. Sacchi CT, Fukasawa LO, Goncalves MG, Salgado MM, Shutt KA, et al. (2011) Incorporation of real-time PCR into routine public health surveillance of culture negative bacterial meningitis in Sao Paulo, Brazil. PLoS One 6: e20675. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Serogroup distribution by age and regions 2006–2008.
(XLSX)
Serogroup distribution by age and regions 2009–2010.
(XLSX)