Abstract
In 1967, the problem of occupational lead exposure came to public attention in Korea. Since then, regular progress has been made in lowering workplace lead exposures, instituting new workplace controls, and implementing health examinations of exposed workers. Past serious lead poisoning episodes made it possible to introduce biological monitoring programs on a voluntary basis in high-lead-exposure facilities in Korea. Industry-specific occupational health services for lead workers in Korea during the last 22 years can be categorized into three phases. During the first phase (1988-1993), efforts were directed at increasing awareness among workers about the hazards of lead exposure, biological monitoring of blood zinc protoporphyrin began, and a respiratory protection program was introduced. During the second phase (1994-1997), a computerized health management system for lead workers was developed, blood-lead measurement was added to biologic monitoring, and engineering controls were introduced in the workplace to lower air-lead levels to comply with air-lead regulations. Finally, during the third phase (1998-present), a new biomarker, bone-lead measurement by X-ray fluorescence, was introduced. Bone-lead measurement proved to be useful for assessing body burden and to demonstrate past lead exposure in retired workers. Occupational health service practice for lead workers, including the industry-specific group occupational health system, has brought considerable success in the prevention of lead poisoning and in reducing the lead burden in Korean lead workers during the last several decades. The successful achievement of prevention of lead poisoning in Korea was a result of the combined efforts of lead workers, employers, relevant government agencies, and academic institutes.
Keywords: Blood zinc protoporphyrin, Blood lead, Bone lead, Maintenance free respirator, Industry specific group occupational health service
Introduction
Although the history of economic growth for Western developed countries spans some 200 years, Korea's economic development was accomplished in a matter of just 4-5 decades after the end of World War II. In the 1950s, Korea was one of the five poorest countries in the world, and the nation depended heavily on foreign assistance from United Nations member states after the Korean War. Now, the most recent estimates indicate that Korea's gross domestic product (GDP) in 2010 was 890.0 billion USD, making Korea the twelfth-largest economy in the world [1,2]. This rapid economic development has produced unwanted side effects in terms of worker health and safety [3-5]. Among the important raw materials in industrial development, lead and its compounds have been widely used in various industrial processes. The problem of occupational lead exposure in Korea first came to public attention in 1967, when the government completed an investigation of lead-using industries as part of an extensive evaluation of occupational hazards in Korean industrial facilities [6]. Since then, regular progress has been made in lowering workplace lead exposure, instituting new workplace controls, and implementing large-scale health screening [7].
In the early stage of Korean industrialization during the 1960s and 1970s, secondary preventive measures (early diagnosis and prompt treatment to minimize morbidity) were thought to be more feasible, and thus a better intervention strategy, than primary preventive measures, such as biological monitoring, which allows the removal of asymptomatic workers from exposure before the initiation of disease processes [8,9].
Until now, on-going regular biological monitoring of lead workers has not been required by Korean regulation. Special medical examinations for lead workers once or twice per year are the only method for surveillance of lead workers required by law. Serious lead poisoning episodes during the last several decades made it possible to introduce biological monitoring as part of a medical surveillance program provided by Korea's specialized occupational health institute in facilities characterized by high-risk lead exposure [10].
In this article, the history of lead poisoning in Korea and the evolution and formation of an occupational health service system for lead workers in Korea during different historical periods are reviewed.
1950s: Pre-economic Development Period and Baseline Period of Occupational Health
Thirty-six years of Japanese occupation followed by three years of the Korean War devastated every sector of the economy. The extremely damaged economic situation made the nation one of poorest in the world. During this period, per capita income was less than 100 dollars and half of the population was in absolute poverty. At this time, Korea was viewed as a hopeless country compared with other Asian countries, such as the Philippines, Thailand, and Myanmar [1].
In 1953, during the Korean War, the Korean government enacted the Labor Standards Law to regulate industrial accidents and occupational diseases. Chapter VI of the Labor Standards Law described the duty of employers to provide measures for workers' safety and health including the implementation of periodic health examinations of workers employed in workplaces with 16 or more employees. The law also described the protection of young workers and female workers in certain hazardous workplaces. In accordance with the law, the first periodic medical examination was performed in the coal-mining industry in the Kangwon area in 1954. Official government records for periodic medical examinations started to appear in 1957. In 1957, 50,675 workers in 305 workplaces had periodic health examinations. Since then, periodic health examinations have been provided to eligible workers by law [5].
During this period, two storage-battery factories manufactured lead-acid storage batteries for automobiles and industrial use, and one primary smelting factory produced lead ingots by smelting lead ores. Several hundred people worked in these factories, but no records of workers' health examinations are available, particularly with regard to their blood-lead levels and other lead-related laboratory data [11,12].
1960s: Start of Economic Development and Advances in Occupational Health
Beginning in the early 1960s, Korea's economy started to develop, relying heavily on government-led economic development plans and an export-promotion policy, and this rapid growth continued into the 1970s.
In 1962, the Catholic Institute of Industrial Medicine (CIIM) was launched to prevent industrial accidents and occupational diseases and to treat injured workers and those with occupational diseases. CIIM was founded by Professor Kyu-Sang Cho who is the founder/pioneer of occupational health in South Korea. Professor Cho has been a leader of occupational health in South Korea for 50 years since the late 1950s.
In 1963, the Korean Industrial Health Association (KIHA) was established to provide occupational health services to industrial facilities and foster the exchange of occupational health knowledge among occupational health personnel, mainly occupational health physicians. In 1963, the CIIM and KIHA, with the cooperation of the Korea Tuberculosis Association and the support of the Ministry of Health, performed a nationwide health examination for workers who were employed in workplaces with 30 or more workers. A total of 148,358 workers in 1,773 workplaces throughout the country were given health examinations, including chest X-rays, parasite tests, and simple blood and urine tests [13]. Five mobile health examination units were assembled for this mass screening survey. The manpower and equipment for this survey were later used for the establishment of a specialized institution for health examination in Korea. Until this survey, workers were not examined or tested for any occupation-related diseases except for pneumoconiosis and noise-induced hearing loss. The objective of the mass screening survey was to find cases of tuberculosis, which was prevalent at that time [11].
In 1967, the CIIM developed blood- and urine-lead analyses to diagnose lead poisoning for the first time in Korea. The CIIM published two papers regarding the normal values of blood- and urine-lead concentrations in 1967 [14,15]. In 1967, for the first time in occupational health history in Korea, the CIIM identified 58 lead poisoning cases among 235 lead workers in 24 lead-using facilities [6]. The mean blood-lead concentrations of workers in seven storage-battery factories and one smelting facility were 72.4 ± 25.6 µg/dL and 71.9 ± 25.6 µg/dL, respectively.
No follow-up was performed due to the lack of a proper occupational health management system at that time. These lead facilities had no available occupational health institution to take care of the lead workers in their local area. The blood-lead measurement was only available for research purposes at the CIIM. At this time, blood lead levels were measured with the dithizone method, which involved a time-consuming and labor-intensive laboratory analysis with a colorimetric technique [16].
1970s: Period of the Promotion of Heavy and Chemical Industry and a Standstill in Occupational Health
In 1972, an examination to detect occupational diseases, called the Special Medical Examination, was added to the existing periodic medical examination system. The Special Medical Examination was provided by law to selected workers who worked in designated workplaces using harmful agents.
During this period, Korea started its exponential economic development, overcoming its longstanding poverty and raising its GDP through the promotion of heavy industry and the chemical industry and through export-oriented government policy. At the same time, from the late 1960s, many medical doctors immigrated to the United States for better medical training opportunities and better future lives, which created a serious shortage of medical manpower in Korea. Rapid growth of the economy always required social and public services in many sectors, particularly in the public health sector. The high demand for medical services throughout the country, even with the shortage of medical doctors, meant that most medical personnel were involved in treatment-oriented medical service in a private clinic or hospital. Very few medical doctors were involved in occupational health service, except for local clinical doctors who were engaged with nearby industries as part-time occupational health physicians by law. In this situation, mass screening, such as periodic medical examination, was the sole and marginal health benefit for most workers in many industries [11].
Outbreak of lead poisoning in the storage-battery industry (1972)
Early in the 1970s, the Labor Administration realized the significance of occupational diseases arising from the rapid development of various industries and requested that the CIIM and KIHA perform several large nationwide surveys relevant to workers' health [11]. One of these surveys was related to lead poisoning and was titled "The Study on Health Impairment and Diagnostic Criteria of Lead Absorption in Korean Lead Workers" [17]. This survey was performed in 1972 with 324 lead workers in the storage-battery, electricity industry, and printing industries. The survey team only included day-shift workers in the survey, excluding night-shift workers. Of the 324 workers tested, 58 were found to have positive scores on a coproporphyrin semi-quantitative test. Ninety-three percent (54/58) of the positive workers were employed in a single storage-battery factory located in the southern part of Korea. The laboratory tests included blood lead, urine lead, urine coproporphyrin semi-quantitative analysis, urine coproporphyrin (CPU), and urine delta-aminolevulinic acid (ALAU).
The analyses of CPU and ALAU were conducted for the first time in Korea by the CIIM for this survey. Hemoglobin and whole-blood specific gravity as a surrogate for hematocrit were also checked, using the Shali hemoglobin meter and the copper sulfate method that used 1.052 and 1.055 specific gravity values, respectively.
The mean blood-lead level of 54 lead workers was above 80 µg/dL; the blood-lead levels of 30 of the workers were above 150 µg/dL.
The workers from this storage-battery factory that were found to have lead poisoning were treated at the Masan Occupational Health Center. Afterward, the Masan Occupational Health Center provided periodic medical examinations for this battery factory and the examinations included coproporphyrin semi-quantitative tests to detect lead poisoning.
In 1978, an outbreak of lead poisoning cases was reported in a primary smelting factory located in the Janghang area. Several severely lead poisoned workers were admitted to the Catholic Industrial Accident Hospital to chelate their high lead burden.
1980s: Period of Rationalization and Liberalization and Period of Refurbishing Occupational Health
Since the 1970s, despite impressive economic and industrial developments, the development of industrial safety and health in Korea had been lagging. The problems related to industrial accidents and occupational diseases accumulated to a point where they became a deterrent to corporate development as well as a social issue.
In 1981, the Labor Agency was promoted to the Ministry of Labor to cope with the issues of industrial safety and health in addition to labor-related social issues [18]. In the same year, the Ministry enacted the Industrial Safety and Health Law, which was separate from the Labor Standards Law.
In 1982, the Ordinance on Industrial Safety and Health specifically outlined the measures with which employers must comply regarding industrial safety and health. The ordinance classified harmful workplaces according to 50 categories of hazardous factors and also detailed the first and second special examinations for each category. In May 1982, the Council of Special Medical Examination Associations was formed to promote effective special medical examinations. This council prevented manipulation of examination fees and fee competition by allocating one institution for each regional examination site and regulating examination fees. As recommended by this council, in February, 1983, the Ministry of Labor designated 24 medical institutions throughout the country for special medical examinations. This new special medical examination system partially succeeded in preventing manipulation of examination fees and heavy competition among institutions, but failed to improve the ability of the examinations to detect occupational diseases compared with the former examination system in certain hazardous workplaces [5]. Unfortunately, many of the medical institutes designated for special medical examinations did not have qualified laboratory personnel and equipment for the measurement of selected heavy metals in blood or urine, which were necessary tools for diagnosing some occupational diseases. Unlike other heavy metals, lead was used in various manufacturing processes, particularly in the storage-battery, smelting, and electronic industries, as well as in other industries, as the Korean economy had continued to expand [12]. Consequently, high lead exposure or lead poisoning cases were anticipated, but very few lead-poisoning cases were reported to the government in the early 1980s.
Banwol lead-poisoning outbreak (1983)
In October 1983, an outbreak of lead poisoning occurred in the Banwol industrial complex. Thirteen high school students were employed as trainee workers at a litharge-making factory for two months during the summer vacation of their third year in preparation for taking jobs at the factory after graduation. One of 13 students suffered from abdominal pain, headache, indigestion, and general malaise and was admitted to a private clinic for a week, but no improvement was observed. The student was transported to one of the university hospitals in Seoul.
The student was diagnosed with acute lead poisoning using lead-specific laboratory data from the CIIM. Soon, the rest of students who worked together at the litharge-making factory were called to the CIIM by their teacher to check their lead absorption levels. Most of them also suffered from abdominal pain, and two students had already had appendectomies because of the pain.
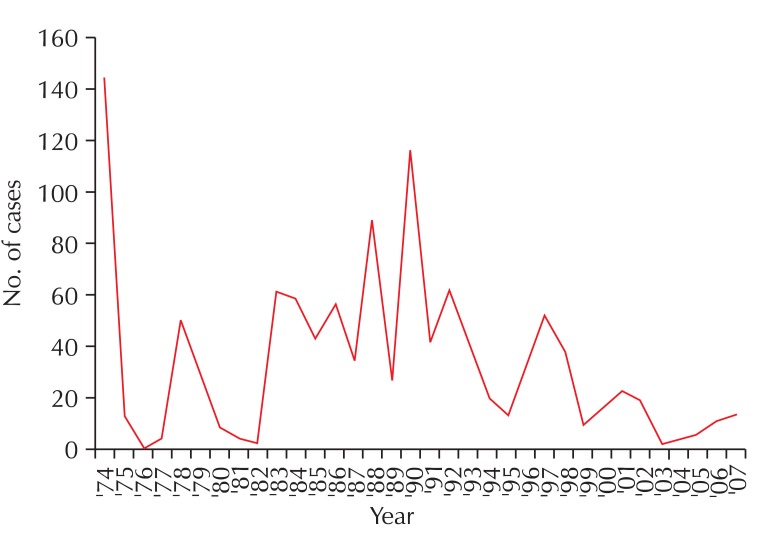
The other students were also diagnosed with acute lead poisoning and began treatment. This episode was reported to the Ministry of Labor. Afterward, the Ministry of Labor performed a field survey with the cooperation of the CIIM and KIHA. The 4-day field survey of the Banwol Industrial Complex area investigated 101 lead workers in seven factories that used lead (six litharge-making factories and one storage-battery factory). The working conditions were deplorable, and the health survey results were striking, with 33 cases of lead poisoning (blood lead > 80 µg/dL) and 36 cases of high lead absorption (blood lead > 60 µg/dL) diagnosed. Among the seven surveyed lead-industry factories, only one (in the storage-battery industry) had conducted the mandated special medical examinations. From that factory, four lead-poisoning cases had been reported to the regional office of the Ministry of Labor, but in this survey, 18 lead-poisoned cases were found among day-shift workers alone. The six other surveyed factories did not provide special medical examinations to detect possible lead poisoning cases. After the 4-day survey, the field survey team recommended a more thorough nationwide survey of facilities using lead, but no further investigation was conducted until one of the largest daily newspapers reported on this survey on its front page and in two related follow-up articles. Immediately after the newspaper reports of the episode of lead poisoning, the Ministry of Labor performed a nationwide survey to check the working conditions of factories and to identify lead-poisoning cases. After the Banwol episode, the number of reported lead poisoning cases increased from single to double digits (Fig. 1).
Fig. 1.
Number of lead poisoning cases reported in special medical examination during the period of 1974-2007.
Nationwide survey of storage-battery factories (1986-1987)
In September 1986, of 258 lead workers in a storage-battery factory, 66 were screened for possible lead poisoning with the semi-quantitative test for CPU and referred for confirmatory laboratory tests, such as blood lead, blood zinc protoporphyrin (ZPP), ALAU, CPU, and hemoglobin. Among the 66 workers that were screened, 29 were diagnosed with lead poisoning by the CIIM. Twelve workers with severe lead poisoning were admitted to two university hospitals to chelate their lead burden. This episode originated from one lead worker's claim of lead poisoning submitted to the government authority. Until this outbreak of lead poisoning, special medical examinations were provided to 10-40% of all lead workers, as the company was located in a local industrial complex area.
The worker's claim brought special medical examinations for lead workers to this factory for the first time. Because the medical institute designated for special medical examinations in the area of this factory did not have laboratory facilities to perform lead-specific analyses, the local medical institute sent blood and urine samples to the CIIM, which was one of the few service laboratories able to conduct measurements of heavy metals in blood and urine in Korea.
This outbreak of lead poisoning, just two years after the Banwol episode, was reported to the Ministry of Labor by the CIIM. The CIIM realized that the outbreak of lead poisoning at this storage-battery factory was the tip of the iceberg with respect to lead poisoning in Korea at that time. Based on the experiences of industrialized countries, relatively high lead absorption in lead workers could be anticipated given the type of operation and work process used, which were old and had not been replaced with the more advanced technology available in industrialized countries. This storage-battery factory moved into the local industrial complex to establish a new type of storage battery with technical support from a well-known US storage-battery company and established a new factory in the late 1970s. Unfortunately, the factory installed machinery for the production of storage batteries without a proper exhaust-ventilation system.
To understand the real status of lead-using industries in Korea at that time and to prevent additional outbreaks of lead poisoning, a comprehensive field survey of the lead industry was needed. The CIIM asked the Ministry of Labor to perform a nationwide survey of the lead industry to investigate the working conditions and lead exposure levels of workers. The Ministry of Labor organized a field survey team of labor inspectors, with occupational health specialists from the CIIM and KIHA. The survey team contacted the Cooperative Storage-battery Association of Korea, an association to which all storage-battery companies belonged, to design the field survey. The association agreed with the survey team that the storage-battery industry would provide full support to perform the survey. The purpose of this preliminary field survey would be to obtain basic data on working conditions and the general health status of lead workers in terms of lead absorption using a portable hematofluorometer to check ZPP levels as a screening tool. The survey team also promised waivers of any kind of prosecution for violations of the Safety and Health Law discovered during the field-survey inspections. The storage-battery industry agreed to develop a comprehensive occupational health program, including improvements in working conditions to meet the government standard.
The survey team selected all 10 storage-battery factories and one lead smelting factory for the survey. The survey comprised four activities: environmental measurement of the workplace; inspection of implementation of special health examinations, including evaluation of individual health examination reports and the proper execution of special health examinations by the local medical institution; measurement of ZPP levels in lead workers to detect high lead absorption and lead-poisoning cases; and assessment of compliance with safety- and health-related regulations.
The survey was performed from November 24, 1986, to January 22, 1987. It revealed that the concentration of lead in the air in some workplaces exceeded the lead standard at that time (0.15 mg/m3), except in one storage-battery factory (factory A), which had experienced a lead-poisoning episode in 1972 and afterward continued to improve its working conditions. ZPP measurements were obtained from 1135 lead workers in 11 lead-using facilities. Twenty-three percent of the workers had ZPP levels of 100 µg/dL or greater, which is the screening criterion for lead poisoning. The distribution of high ZPP levels among the factories varied widely. The lowest percentage of high ZPP levels was observed in factory A (3.2%), but more than 20% of workers were found to have high ZPP levels in most other factories. The survey also confirmed that most regional medical institutions qualified by the Ministry of Labor for the special medical examination were poorly prepared to perform lead-related special medical examinations.
The survey resulted in a recommendation to the Ministry of Labor that it needed to work diligently to solve the problem of lead poisoning in Korea, a prevalent condition, within a few years. The main points of this recommendation were: 1) the necessity of agent-specific (industry-type specific) occupational health services by a specialized institute to take care of lead workers; 2) the necessity of loosening the environmental standards in the workplace (0.15 mg/m3) for a short, specified period of time as an interim measure to stimulate employers to comply with air-lead standards; 3) the necessity for a central laboratory facility to provide laboratory services to local occupational health centers that were not able to conduct certain specific analyses, such as tests for heavy metals in blood and urine.
Respiratory protection program with biological monitoring of ZPP levels (1987)
One storage-battery factory in the CIIM's special medical examination area had a serious problem with production space because of an increase in production lines, and the factory management had decided to move to a larger facility in a new location. In the meantime, because of serious problems with working conditions and the high prevalence of high lead burden among the workers, this factory requested that the CIIM recommend swift and feasible measures to prevent lead poisoning and to reduce the workers' lead burden. Because this factory would soon move to a new location and could not renovate its existing facility or improve working conditions through engineering controls, the CIIM recommended a respiratory protection program with a maintenance-free respirator which was cup-shaped, disposable, and was a highly efficient dust-trapping respirator in addition to regular biological monitoring with the measurement of ZPP levels. Until then, the factory had provided lead workers with gauze-type facemasks as respirators, which could not protect against respirable lead dust or fumes. The CIIM proposed to the company and 3M Korea that they initiate a 6-month field study of a 3M maintenance-free respirator (MFR). 3M Korea agreed to provide enough MFRs to perform the respiratory protection study for 60 lead workers over a 6-month period. The study produced dramatic results: the workers who used MFRs had a rapid decrease in ZPP levels within 3 months compared with a control group who used a regular gauze-type mask. At the end of the study period, the blood ZPP level in the MFR group had dropped by more than half (from 140 to 63 µg/dL). The company decided to provide 3M respirators to its lead workers. Although 3M Korea thought that it was premature to introduce these respirators into the Korean industry because of their high cost and the lack of legal certification for MFR-type respirators in Korea, the company wanted this type of respirator because of its ease of use compared with half-face respirators. This was the beginning of the use of MFR respirators by lead workers, and later by other workers in general industries. In 1992, the Ministry of Labor made the MFR-type respirator a certified respirator by regulation.
New regulation on group occupational health services (1987)
In accordance with the recommendation of the survey team discussed above, the Ministry of Labor revised existing regulations on group occupational health services to create two new occupational health services, termed the area-specific group occupational health service and the industry-specific occupational health service [19].
The group occupational health service was introduced to provide legal occupational health services to small and medium-size factories that had no qualified occupational health personnel. This system required regular monthly visits to the contracted factory by qualified personnel (medical doctor, occupational health nurse, and industrial hygienist), which made ongoing occupational health monitoring possible. However, this service had a limitation. Qualified group occupational health centers can only provide their services in permitted areas to avoid heavy competition among occupational health institutes throughout the country. Usually, one institute in any area was designated as a qualified service center. Therefore, to facilitate specialized occupational health services in certain hazardous industries, such as lead- and mercury-using industries, the Ministry of Labor decided to create an occupational health service for these industries. This new service provided service throughout the country and was certified by the Ministry of Labor instead of by the local regional office of the Ministry of Labor, which certified the area group occupational health service.
Designation of soonchunhyang institute of environmental & occupational medicine for industry (lead)-specific group occupational health service (June, 1988)
In June 1988, the Ministry of Labor designated the Soonchunhyang Institute of Environmental & Occupational Medicine (SIEOM) as an authorized industry (lead)-specific group occupational health service center to protect lead workers from lead poisoning and to provide ongoing medical surveillance service throughout the country. During the period from June to December 1988, 27 lead-using facilities (with 4,967 workers) were contracted to receive occupational health services from the SIEOM. The contracted lead facilities were high-risk facilities including those in the storage-battery industry, primary and secondary smelting industries, litharge-making industries, and several others. The institute started to provide legally required occupational health services (special medical examinations, environmental measurement of the workplace, health management) and biological monitoring using ZPP measurements, along with a proper respiratory protection program.
1990s-2000s: New Era of Democracy, Globalization, and Growth of Occupational Health
As democratization progressed and occupational diseases, such as mercury poisoning and carbon disulfide poisoning, began to surface, the government began to respond. In January 1990, in response to society's and workers' requests for reforms in the Industrial Health and Safety Law, the government publicly announced that the general provisions for Industrial Safety and Health were amended.
In June 1991, the government set up and enforced a master plan for occupational disease prevention, which focused on preventing occupational diseases and strengthening employers' responsibilities.
During the 1990s, sudden outbreaks of occupational diseases were reported. These included carbon disulfide poisoning, metal-related poisoning (mercury, chrome, and manganese), occupational asthma, coke-oven emission-related poisoning, cadmium poisoning (which proved controversial), malignant methothelioma due to asbestos, hepatic necrosis due to dimethylformamide (DMF), reproductive disorders due to 2-bromopropane poisoning, occupational diseases among ship-building industry workers, and visual display terminal (VDT)-related health problems [2,4,5].
Industry (lead)-specific group occupational health service (1988-present)
The occupational health services provided by the SIEOM for lead workers in Korea during the last 22 years can be categorized into three phases.
First phase (1988-1993)
The 1986 government field survey found that most lead-using facilities in Korea did not provide special health examinations to all their lead workers, and only a few lead workers took advantage of the examinations. Except for one storage-battery factory, no lead-using facilities provided proper respiratory protection programs for their workers. Before the introduction of new occupational health services, no formal or informal health education about the hazards of lead was provided to lead workers. So an effort was directed at increasing awareness among workers about the hazards of lead exposure, with regular health education on an individual or group basis. Biological monitoring using ZPP measurement with a portable hematofluorometer was started to evaluate the health status of lead workers. At the same time, a respiratory protection program was introduced to reduce the exposure level of lead workers whose working conditions were not acceptable. The success of the field intervention study in 1987 with MFR to reduce the ZPP levels of lead workers made a strong impression on other lead-using facilities. Thus, respiratory protection with MFR and biological monitoring using ZPP measurements became the main tools used to protect lead workers from high lead absorption [8].
In 1990, the Korean government lowered the occupational exposure limit (OEL) for lead in air from 0.15 to 0.05 mg/m3 [20]. Except in one storage-battery factory with a modern facility, no other lead-using factories under contract could comply with this OEL. At this time, Korea had experienced a period of social reform in various aspects of society and there was a shortage of labor in the so-called "3D" industries (Dirty, Dangerous, and Difficult). Because many lead-using facilities belonged to this 3D category, they had a difficult time recruiting and hiring new workers, resulting in severe labor shortages. The shortage of workers created a greater risk of high lead exposure to current lead workers. Thus, it was impossible to lower the lead exposure of current workers and very difficult to just maintain the current status and to avoid any worsening of conditions. This situation had an interesting result: within 3 years, all lead-using facilities under contract started respiratory protection programs with MFR devices.
The worst cases of high lead exposure were discovered in small and medium-sized lead-using facilities, such as secondary smelting and litharge-making factories. At the end of this phase, the beneficial effect of respiratory protection with biological monitoring was beginning to slowly emerge, particularly in storage-battery factories, in terms of reductions in mean ZPP levels and blood-lead levels.
Second phase (1994-1997)
To evaluate lead exposure data of workers in a more efficient way, a new health-management computer program that utilized a personal computer was developed in 1993 was put into practice beginning in 1994. Computerized data for lead workers were extensively used during ongoing biological monitoring at the site.
The reduction in the mean blood-lead levels during the first phase in some lead-using facilities made blood-lead measurement necessary for basic biological monitoring. During the early stages of this second phase, lead-using facilities monitored blood-lead levels twice or four times a year in addition to ZPP measurements. The necessity of blood-lead measurements for basic biomarkers was well accepted in most lead-using industries, so blood-lead measurements were added for basic biological monitoring once or twice a year beginning in 1994.
A new monitoring program using blood lead and ZPP levels together as biomarkers of lead exposure resulted in further reductions in lead absorption in most lead-using facilities that were under contract.
Measurement of ZPP levels was still used as the primary screening tool under the regulatory scheme for special health examinations. Only lead workers whose blood ZPP level was 100 or more µg/dL were regarded as screening positive under the official reporting system. Blood-lead levels of 40-50 µg/dL were also used as a screening criterion for further evaluation of lead workers during the regular monitoring period.
At the same time, engineering controls were introduced to lower air-lead levels to comply with air-lead regulations (OEL: 0.05 mg/m3) that were effective in 1990. Some storage-battery factories introduced new types of operations, such as expanded-type casting to reduce lead exposure from classical casting processes and automatic stackers to replace manual stacking processes that produced high air-lead levels from dust. Quite a lot of engineering controls were introduced during this period. But still, it was very difficult to comply with the strict OEL for air lead, a level that was half of that in Japan and one-third of that in many industrialized countries. The strict OEL eventually would induce the improvement of working condition with effective enforcement, but would also endanger the existence of certain industries which could not comply the regulation due to the inherent problem of work process, like the old style operation of the storage battery industry.
Third phase (1998-present)
The new biological monitoring approach using blood lead and ZPP levels in conjunction with an appropriate respiratory protection program resulted in a considerable decrease in lead absorption among lead workers, as reflected in blood-lead and ZPP levels, in most lead-using facilities except a few small factories. In 1997, the prevalence rate of ZPP screening resulted in positive results (ZPP ≥ 100 µg/dL) was less than 5-7% in storage-battery factories. The reduction in lead-exposure levels in terms of ZPP and blood lead levels brought new attention to non-occupational health problems, such as cardiovascular disease, liver disease, and other non-occupational conditions. The prevalence of non-occupational disease in lead workers was well above 5%. Korean government regulations required that every employer should provide a general health examination (chest X-ray, blood pressure measurement, SGOT, SGPT, γGTP, blood sugar) for lead workers annually. The SIEOM began to provide more comprehensive biochemical tests (18 items) in addition to the routine components of the general health examination.
The SIEOM also began to provide various lead-related examinations as a part of ongoing research activities in collaboration with the Johns Hopkins University School of Hygiene and Public Health, with support from the United States National Institute of Environmental Health Sciences (NIEHS). Such new biomarkers, such as bone-lead levels by X-ray fluorescence, DMSA-chelatable lead levels, genetic markers of susceptibility, and renal early biologic effect measures, are currently being used, and the SIEOM will evaluate their utility as tools for prevention. The SIEOM has been focusing on such health measures as neurobehavioral function, peripheral nervous system function, blood pressure, hematopoietic system function, and renal function. Two large-scale research projects funded by the NIEHS in collaboration with Johns Hopkins University were possible with full support of employers and employees in lead-using facilities that were contracted with the SIEOM. These large research projects not only produced much valuable scientific knowledge with respect to lead poisoning, resulting in publication of more than 40 research papers in international journals [21,22], but also contributed to the improvement of lead workers' health.
Bone-lead results obtained from the research play a major role in finding retired lead-poisoned workers who have high blood- and bone-lead levels. Five retired lead workers who were diagnosed with chronic lead poisoning obtained government benefits from the Industrial Accident Compensation Insurance Act.
Bone-lead measurement by X-ray fluorescence has great promise as a biomarker for evaluating the cumulative effect of lead. In the future, it may be desirable to include bone-lead measurements for the protection of the long-term health of lead workers.
Current Status and Future Needs Regarding the Occupational Health of Lead Workers
The number of lead-poisoning cases reported to the government by law in the late 2000s was fewer than six per year (Fig. 1). The mean blood-lead levels of lead workers in 2008 who worked in facilities with special occupational health service contracts with the SIEOM were 20 µg/dL or lower in primary smelting and medium and large storage-battery factories. Those in secondary smelting, litharge-making, and small storage-battery factories were 30 µg/dL or lower. Compared with data from the 1980s, the decreases in blood-lead levels were significant. No cases of lead poisoning were reported. In 2009, the Korean blood-lead criterion for the diagnosis of lead poisoning in special medical examinations was strengthened further from 60 µg/dL to 40 µg/dL, which is the strictest level in the world. Even with the new criterion, none of the lead workers at companies that were contracted with the SIEOM was classified as having lead poisoning.
The current blood-lead levels of Korean lead workers have been lowered considerably, but they are still high compared with environmentally safe levels. The SIEOM and contracted lead factories together are trying to reduce workers' lead burden to as low a level as possible through engineering controls and active occupational health services. The lead-using industries already are aware that the current blood-lead levels of their workers are not acceptable, and in the near future, new regulations regarding blood-lead levels will be promulgated. Under these circumstances, some Korean lead factories are in a better position to take care of their lead workers using bone-lead data as part of their health management systems. Once the bones store relatively high amounts of lead from any source, it is very difficult to reduce these pools in a short time; a few decades are needed for levels to return to normal. So it is wise to use bone-lead data to predict the future body burden and to supervise lead workers to ensure that lead burdens are kept as low as possible.
The ideal blood-lead level is somewhere near the value of the general population, which is now far below 5 µg/dL. To achieve this goal, the role of bone lead will be very important. The limitations of bone lead measurements, such as the time required for measurement and the poor performance of tests at low levels, needs to be overcome [23].
The successful prevention of lead poisoning in Korea is a shared accomplishment of lead workers, employers, relevant government agencies, and academic institutes. Lead workers followed occupational health regulations by wearing respirators properly for a quite a long time until their working conditions could be improved. Some lead workers still wear their respirators, even in workplaces with safe levels of lead exposure, for double protection against possible lead absorption. Employers have invested their limited budgets in the protection of their workers from high lead exposure by providing good respirators during the early stage, developing engineering controls in the workplace, and installing new operational systems to improve productivity and to prevent high lead absorption by workers. Success would have been impossible without flexible and comprehensive government support through the government field survey of the lead industry and the stipulation of new regulations for the specific group occupational health service. Finally, the continuous concern and passion of academic institutes with their scientific consideration of lead-related health matters played an important role keeping the system running as it developed.
Conclusion
After several outbreaks of lead poisoning since the beginnings of Korean industrialization in the 1970s, a specialized occupational health service for lead-using facilities was developed by relevant parties, including the government, the lead industry, and academic institutes.
The SIEOM was designated as the industry-specific group occupational health service institute in 1988. Since 1988, an active occupational health program for lead facilities in Korea and a respiratory protection program combined with biological monitoring of ZPP and blood lead levels made great contributions to protecting the health of lead workers, even under unfavorable working conditions.
It was learned that in a rapidly developing country such as Korea, which could not introduce engineering controls quickly enough to protect lead workers, biological monitoring of ZPP levels was very useful in identifying and lowering excess lead absorption. The utility of a respiratory protection program was also demonstrated. The data revealed that during the ZPP-monitoring phase, blood-lead levels declined in Korea. Once the mean blood-lead level declined to less than 40 µg/dL, ZPP levels could no longer be used as the primary biomonitoring tool; at this point, blood lead was routinely measured. The occupational health service practice for lead workers, including the industry specific group occupational health system, has brought about considerable success in prevention of lead poisoning and in reducing the lead burden in Korean lead workers during the last several decades.
In the future, as the average exposure duration continues to increase, bone-lead measurements may be highly recommended to adequately protect the long-term health of workers and to enable lead workers to maintain their lead burden as low as possible.
The Korean experience with its occupational health service system for the prevention of occupational lead poisoning can be transferred to other countries, particularly to newly developing countries that are following similar paths of industrial development.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Cho DS. Design, economic development, and national policy: lessons from Korea. Des Manag Rev. 2004;15:10–20. [Google Scholar]
- 2.Paek D, Hisanaga N. Occupational health in South Korea. Occup Med. 2002;17:391–408. [PubMed] [Google Scholar]
- 3.Lee SH. Occupational medicine in Korea. Int Arch Occup Environ Health. 1999;72:1–6. doi: 10.1007/s004200050326. [DOI] [PubMed] [Google Scholar]
- 4.Kang SK, Kim EA. Occupational diseases in Korea. J Korean Med Sci. 2010;25(Suppl):S4–S12. doi: 10.3346/jkms.2010.25.S.S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park J, Kim Y. The history of occupational health service in Korea. Ind Health. 1998;36:393–401. doi: 10.2486/indhealth.36.393. [DOI] [PubMed] [Google Scholar]
- 6.Korean Industrial Health Association. Survey report on safety and health management in Korean industrial establishments. Seoul (Korea): Korean Industrial Health Association; 1967. p. 122. [Google Scholar]
- 7.Lee BK. Lead poisoning in Korea. Korean J Occup Health. 1991;30:1–9. [Google Scholar]
- 8.Ahn KD, Lee BK, Nam TS. The effect of maintenance free respirator on the prevention of lead absorption in lead using workers of Korea. Korean J Occup Environ Med. 1989;1:180–185. [Google Scholar]
- 9.Lee BK, Lee CW, Ahn KD. The effect of respiratory protection with biological monitoring on the health management of lead workers in a storage battery industry. Int Arch Occup Environ Health. 1993;65(1 Suppl):S181–S184. doi: 10.1007/BF00381336. [DOI] [PubMed] [Google Scholar]
- 10.Lee BK. The role of biological monitoring in the health management of lead-exposed workers. Toxicol Lett. 1999;108:149–160. doi: 10.1016/s0378-4274(99)00083-1. [DOI] [PubMed] [Google Scholar]
- 11.Korean Industrial Health Association. Thirty years history of Korean Industrial Health Association. Seoul (Korea): Korean Industrial Health Association; 1993. p. 419. [Google Scholar]
- 12.Park YP. A study on the promoting plans for Korea Secondary Lead Smelting Industry [dissertation] Seoul (Korea): Hanyang Univ; 2003. [Google Scholar]
- 13.The report of the physical examination on laborers and their working conditions in Korea, 1963. Seoul (Korea): The Catholic University of Korea Catholic Institute of Industrial Medicine; 1964. pp. 5–43. [Google Scholar]
- 14.Yoo JS. A study on normal lead level in blood of Korean male adults. Korean J Public Health. 1968;5:129–134. [Google Scholar]
- 15.Oh SM. A study on normal urinary lead level of Korean male adults. Korean J Public Health. 1968;5:135–138. [Google Scholar]
- 16.Chung KC. Criteria for the assessment of lead absorption in Korea. New Med J. 1969;12:45–58. [Google Scholar]
- 17.Korean Industrial Health Association. The study on health impairment and diagnostic criteria of lead absorption in Korean lead workers. Seoul (Korea): Korean Industrial Health Association; 1972. p. 20. [Google Scholar]
- 18.Park J, Kim Y, Kim KS. Remodeling of the occupational medical examination program in South Korea. Int Arch Occup Environ Health. 1999;72:411–417. doi: 10.1007/s004200050394. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Labor. Regulation on group occupational health service. Ministry regulation 142. Gwacheon (Korea): Ministry of Labor; 1987. Korean. [Google Scholar]
- 20.Ministry of Labor. Regulation on permissible exposure level. Gwacheon (Korea): Ministry of Labor; 1990. Korean. [Google Scholar]
- 21.Schwartz BS, Lee BK, Lee GS, Stewart WF, Lee SS, Hwang KY, Ahn KD, Kim YB, Bolla KI, Simon D, Parsons PJ, Todd AC. Associations of blood lead, dimercaptosuccinic acid-chelatable lead, and tibia lead with neurobehavioral test scores in South Korean lead workers. Am J Epidemiol. 2001;153:453–464. doi: 10.1093/aje/153.5.453. [DOI] [PubMed] [Google Scholar]
- 22.Lee BK, Lee GS, Stewart WF, Ahn KD, Simon D, Kelsey KT, Todd AC, Schwartz BS. Associations of blood pressure and hypertension with lead dose measures and polymorphisms in the vitamin D receptor and delta-aminolevulinic acid dehydratase genes. Environ Health Perspect. 2001;109:383–389. doi: 10.1289/ehp.01109383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Todd AC, Chettle DR. Calculating the uncertainty in lead concentration for in vivo bone lead x-ray fluorescence. Phys Med Biol. 2003;48:2033–2039. doi: 10.1088/0031-9155/48/13/314. [DOI] [PubMed] [Google Scholar]