Abstract
Objective
To assess the association between correction of myopia, hyperopia and astigmatism with self-reported near and distance visual function.
Design
Population based, cross-sectional study.
Participants
A random sample of 4272 Latinos over 40 years old from Arizona with both ophthalmic exam and questionnaire data, including answers to the NEI VFQ-25.
Methods
Cases of refractive error (RE) were defined as subjects who met at least one of the following criteria in both eyes: myopia, sphere ≤-0.5 diopters (D); hyperopia, sphere ≥1.0D; astigmatism, cylinder≥0.75D. Uncorrected refractive error (URE) was defined as having RE and achieving ≥2 line improvement in visual acuity in both eyes after refraction. The association between RE category and near and distance vision difficulty (as measured by the National Eye Institute Visual Functioning Questionnare-25 near and distance vision subscores) was modeled with ordinal logistic regression, adjusting for age, sex, diabetes, hypertension, income, education and acculturation.
Main Outcome Measures
Association between RE correction and near and distance vision difficulty by type of RE (myopia, hyperopia, and astigmatism).
Results
Of 4272 participants, 54% had RE. 48% of these had myopia, 41% hyperopia, and 11% astigmatism. 14% of myopes, 21% of hyperopes, and 22% of astigmatics had URE. Subjects with myopia, astigmatism, and hyperopia were significantly more likely to report more distance vision difficulty than subjects without RE, whether or not they had correction (Odds Ratios (OR) from 1.7-3.7; p<0.005 for all). Subjects with corrected myopia reported less near vision difficulty than subjects without RE (OR 0.8, Confidence Interval (CI) 0.7-0.9). Subjects with uncorrected hyperopia and uncorrected astigmatism reported more near vision difficulty than those without RE (OR 1.6, CI 1.2-2.2 and OR 1.7, CI 1.0-3.0, respectively). Self reported distance and near visual function scores were sensitive to non-vision variables; namely, age, sex, diabetes, high blood pressure, acculturation score, income, and education.
Conclusions
in our population, correction of any type of RE is not entirely sufficient to restore distance visual function to the level of those without RE. More research is necessary to determine the reasons for this shortcoming.
INTRODUCTION
Uncorrected refractive error (URE) is a leading cause of blindness worldwide as well as the primary cause of visual impairment in the United States (US). 1,2 Studies have reported that among United States Latino populations, URE is associated with older age and socioeconomic factors such as lower levels of income and education.3-5 Functional limitations due to URE compound this relationship by decreasing productivity, as highlighted by research that attempts to identify the magnitude of productivity that is lost globally.6
Recent research has focused on describing the negative effect that URE has on vision specific quality of life.7-10 The National Eye Institute Visual Functioning Questionnaire (NEI VFQ-25) is a tool that quantifies the degree to which an individual’s visual impairment results in functional difficulty.11,12 While previous studies have used this tool, and other questionnaires, to demonstrate that URE has a negative impact on vision-specific quality of life, few studies have examined the effects of different types of refractive error (RE), namely, myopia, hyperopia, and astigmatism, on visual function. The Singapore Malay Eye Study used a visual function questionnaire to assess the association between RE correction and visual function within myopia, hyperopia, and emmetropia.7 However, this study used an overall score for general vision as well as several independent items related to visual function, rather than composite scores for near vision function and distance vision function. The authors found that RE correction was associated with higher function scores among subjects with myopic RE, but not among those with hyperopic RE.
Proyecto Ver is a population based, cross sectional survey of ocular disease and visual function as measured by the NEI VFQ-25 among Latinos in southern Arizona. This study utilizes two previously validated subscores within the NEI VFQ-25, the near vision subscore and the distance vision subscore, to analyze visual function within the Proyecto Ver population.13 We aim to describe the association between uncorrected and corrected RE correction with near and distance vision subscores by type of refractive error (myopia, hyperopia, and astigmatism). We also aim to determine which factors independently affect self-reported visual function.
METHODS
Study Design
Study methods have been previously described in detail.5,8,14 Briefly, Proyecto Ver is a population based, cross sectional survey of ocular disease and visual function in Latinos living in southern Arizona. Based on the 1990 US census, a stratified random sample of block groups in Nogales and Tucson were selected, with probability of selection within the strata proportional to the size of the Latino population over 40 years of age in each block group. Every other household in Nogales block groups, and two thirds of household in Tucson block groups were chosen for determination of eligibility. Self-described Hispanic or Latino household members over 40 years of age were considered eligible. Participation rate was 72%.
After obtaining informed consent, participants had an extensive home interview and were scheduled for ophthalmic examination at a central clinic site. All study procedures were approved by the Johns Hopkins University Joint Committee on Clinical Investigations and the University of Arizona Institutional Review Board and complied with the tenets of the Declaration of Helsinki.
Home Interview
The questionnaire was offered in English and Spanish by trained personnel, and 80% of interviews were conducted in Spanish. Participants were asked questions regarding their education, socioeconomic and health status, and history of vision problems. Additionally, participants were asked a series of questions from the Hispanic Health and Nutrition Examination Survey (HHANES) on preferred language, country of birth, and other topics pertaining to level of adaption to U.S. culture. These answers were converted to an acculturation score, which ranges from 1, indicating low acculturation, to 5, indicating high acculturation.
Finally, the questionnaire also included a measure of functional status, the shortened National Eye Institute Visual Function Questionnaire, or NEI VFQ-25. Twelve domains of function are included in the NEI VFQ-25. The near vision and distance vision domains consist of 3 items each.12 For each of these subscales, responses were scored on a scale of 0 to 100. The near and distance vision subscales were chosen for assessment of visual function difficulty in this study because they have been previously validated.13
Clinical Exam
At the central clinic site, three blood pressure readings were taken. The average of the final two readings was used to characterize blood pressure. Blood samples were obtained to determine hemoglobin A1C levels.
Distance visual acuity was tested in each eye with a modified Early-Treatment Diabetic Retinopathy Study (ETDRS) chart at 3m, illuminated at 130cd/mˆ2, using a forced-choice procedure in which persons are asked to guess at letters rather than simply stop. Participants who failed to read the largest letters at 3m were retested at 1.5m, and then at 1m. Presenting visual acuity (PVA) was measured with the participant’s habitual distance correction. Best corrected visual acuity (BCVA), after subjective refraction, was measured in each eye. Results from testing with an autorefractor (Humphrey instruments Inc., San Leandro, CA) were used as a starting point for full subjective refraction. Visual acuity was scored as the total number of letters read correctly, transformed to log minimum angle of resolution (logMAR) units. Failure to read any letters was assigned an acuity of 1.7 logMAR units, which is equivalent to an acuity of 20/1000. An E chart was used for participants who were illiterate.
Definitions
Refractive error (RE) was defined as an eye with sphere correction ≤-0.5 diopters (D) or ≥1.0D or cylinder≥0.75D. An individual was considered to have RE if both eyes met the above criteria. Refraction information was extracted using a lensometer with a standard protocol for placement of the lenses from the glasses for those wearing glasses whose PVA was 20/25 or better. Information on refractive error was obtained from subjective refraction for those who had PVA worse than 20/25.”
Subjects with RE were subdivided into three groups, based on the spherical error of the “better eye,” or the eye whose spherical error was closer to zero. Those whose better eye spherical error was ≤-0.5D were classified as myopic, those with spherical error ≥1.0D as hyperopic. Subjects with spherical error between -0.5D and 1.0D, but with bilateral cylinder error ≥0.75D, were classified as astigmatic. Subjects with bilateral RE of a different type in each eye were categorized based on the better eye’s spherical equivalent in diopters. For example, if one eye was astigmatic and the other eye had spherical error, the better eye was chosen by comparing the diopters of spherical error to the diopters of cylinder error divided by two.
The “no RE group” consisted of: individuals without correction with PVA 20/25 or better, individuals without correction or identifiable eye disease causing visual loss whose PVA was worse than 20/25 and failed to improve with subjective refraction, individuals with RE in only one eye, and those with correction who did not meet the above definition of RE.
URE was defined as having an improvement in visual acuity ≥2 lines in both eyes. Individuals who had corrected RE in one eye and URE in the other were classified as corrected RE.
Hypertension was defined as a positive answer to the question of whether the person has hypertension and is currently under treatment with antihypertensive medication, or had systolic pressure of 160mmHg or higher or diastolic pressure of 90mmHg or higher on the average of the final two blood pressure readings.
Diabetes was defined as either an affirmative response to the question of whether diabetes had been diagnosed by a physician or having an HbA1c of 7.0% or greater.
Exclusions
Participants with bilateral BCVA worse than 20/200 (n=11) or missing or ambiguous visual testing data (n=20) were excluded, as it was not possible to accurately assess visual acuity. Patients with bilateral cataract surgery (n=244) were also excluded because the absence of natural lenses precluded accurate assessment of previous RE. Finally, patients with other eye disease causing visual loss that was not improved with refraction (including cataract, macular degeneration, glaucoma, keratoconus, and corneal dystrophy) (n=222) were excluded, so as not to obscure the relationship between functional status and RE.
Statistical Methods
The distribution of near vision function scores and distance vision function scores were highly skewed. For the purpose of analysis, the scores were transformed into an ordinal variable. Visual inspection of the score distributions suggested cutoff values of ≤75 and ≤100, creating three difficulty score categories for both near and distance vision function scores.
An ordinal logistic regression model was chosen to analyze the relationship between RE category and level of visual function difficulty. The proportional odds assumption was checked to ensure that the model was appropriate. Associations are reported as odds ratios (OR) with 95% confidence intervals (CI). ORs for associations were considered statistically significant if they maintained a p value less than 0.05.
Regression models were selected using stepwise methods. First, potential covariates were checked for age-adjusted association with the outcome of function score category. Covariates with an age-adjusted association with either outcome at the 0.10 level were selected for the multivariate analysis phase. Covariates that maintained a p-value of <0.05 in the final models were kept. The Akaike Information Criteria (AIC) was utilized to confirm the best fitting model. The final model included the variables for age, sex, education, income, acculturation, hypertension, and diabetes. Data was analyzed using STATA (STATA Statistical Software: Release 10, College Station, TX).
RESULTS
A total of 4272 participants were included in the final analysis, and 54% had RE (Table 1). The average age of the total population was 55 years (S.D. 11 years). 61% of subjects were female, 66% had an income of <$20,000, 20% had diabetes, and 43% had high blood pressure (Table 1). The highest grade completed on average was 9.2 (SD 4.0), and the average acculturation score was 2.0 (SD 1.0) on a scale of 1 to 5 (Table 1). In the whole population, 39% of total subjects reported no near vision difficulty, and 61% of total subjects reported no distance vision difficulty.
Table 1.
Population characteristics by vision score category
| Near vision score categories | Distance vision score categories | Total | |||||
|---|---|---|---|---|---|---|---|
| No Difficulty | Mild Difficulty | More Difficulty | No Difficulty | Mild Difficulty | More Difficulty | ||
| Total, N | 1653 | 1710 | 909 | 2616 | 1220 | 436 | 4272 |
| Age, mean (SD) | 56.1 (11.4) | 55.1 (10.7) | 55.0 (10.5) | 54.7 (10.5) | 56.1 (11.0) | 57.9 (12.1) | 55.4 (10.9) |
| Female, % | 56.9% | 62.3% | 66.8% | 55.5% | 69.0% | 73.4% | 61.2% |
| Highest grade level, mean (SD) | 9.7 (4.0) | 9.0 (3.9) | 8.5 (3.9) | 9.4 (4.0) | 9.0 (3.9) | 8.2 (4.1) | 9.2 (4.0) |
| Acculturation Score, mean (SD) | 2.0 (0.9) | 2.0 (1.0) | 2.0 (1.0) | 2.0 (0.9) | 2.1 (1.0) | 2.1 (1.0) | 2 (1.0) |
| Income < $20,000, % | 59.5% | 67.3% | 76.0% | 62.5% | 68.9% | 80.4% | 66.1% |
| Diabetes, % | 18.0% | 19.4% | 25.6% | 18.0% | 22.4% | 26.9% | 20.2% |
| Hypertension. % | 41.4% | 43.2% | 43.5% | 41.5% | 43.5% | 46.3% | 42.6% |
Acronym key: SD (Standard Deviation)
The distribution of near and distance visual function scores for the study population as a whole was highly skewed (Figures 1A and 1B). Scores were transformed into an ordinal variable by choosing two cutoff values, creating three score levels. Under near vision function, 21% of subjects had “more difficulty” (score under 75), 40% had “mild difficulty” (score 75-99), and 39% had “no difficulty” (score of 100) (Table 1). Under distance vision function, 10% of subjects had “more difficulty” (score under 75), 29% had “mild difficulty” (score 75-99), and 61% had “no difficulty” (score of 100) (Table 1).
Figure 1.
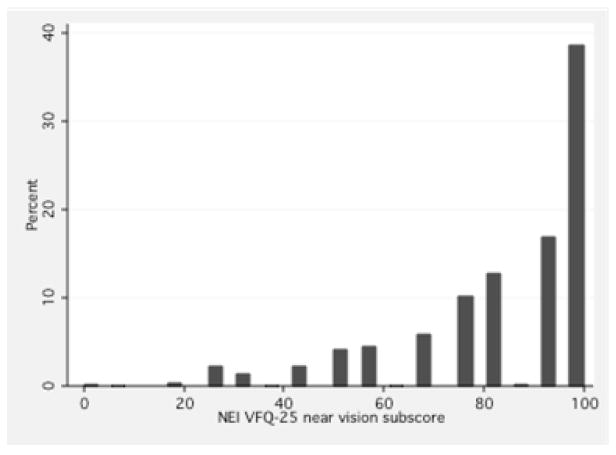
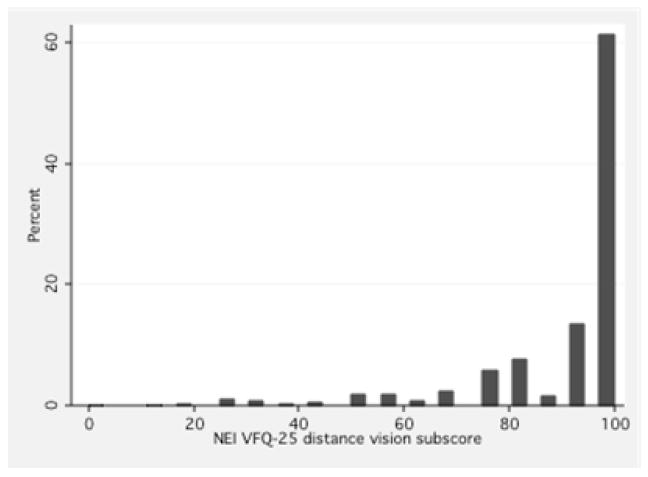
A: Histogram of NEI VFQ-25 near vision function subscore distribution
B: Histogram of NEI-VFQ 25 distance vision function subscore distribution
Two cutoff values were chosen to create three score levels. Scores under 75 were categorized as “more difficulty.” Scores from 75-99 were “mild difficulty,” and scores of 100 were “no difficulty.”
Acronym and abbreviation key: NEI VFQ 25 (National Eye Institute Visual Functioning Questionnaire-25).
Of those with refractive error, 48% (944/1982) subjects were myopic, 41% (812/1982) were hyperopic, and 11% (226/1986) were astigmatic. Of those with myopia, 14% (135/944) had uncorrected myopia. A greater proportion, 21%, of those with hyperopia had uncorrected refractive error, and 22% of those with astigmatism were uncorrected (Table 2).
Table 2.
Distribution of refractive error type into score categories
| Refractive error category | Number per RE group | Near vision score categories | Distance vision score categories | |||||
|---|---|---|---|---|---|---|---|---|
| No Difficulty | Mild Difficulty | More Difficulty | No Difficulty | Mild Difficulty | More Difficulty | |||
| No RE | 2290 | 36.3% | 42.2% | 21.4% | 69.2% | 24.5% | 6.3% | |
| Myopia | Corrected | 809 | 45.1% | 37.0% | 17.9% | 53.9% | 32.6% | 13.5% |
| Uncorrected | 135 | 34.0% | 43.0% | 23.0% | 35.6% | 41.5% | 23.0% | |
| Astigmatism | Corrected | 176 | 41.5% | 35.8% | 22.7% | 54.6% | 34.7% | 10.8% |
| Uncorrected | 50 | 28.0% | 38.0% | 34.0% | 50.0% | 34.0% | 16.0% | |
| Hyperopia | Corrected | 639 | 42.6% | 37.7% | 19.7% | 52.9% | 32.1% | 15.0% |
| Uncorrected | 173 | 29.5% | 36.4% | 34.1% | 51.4% | 32.4% | 16.2% | |
Acronym and abbreviation key: RE (Refractive Error).
Using subjects with no RE as a reference group, we examined the relationship of refractive error to near vision difficulty (Table 3). Subjects with corrected myopia were significantly less likely to report near vision difficulty (OR 0.78, 95% CI 0.68-0.93). In the same model, subjects with uncorrected hyperopia (OR 1.65, 95% CI 1.21-2.23) and uncorrected astigmatism (OR 1.75, 95% CI 1.01-3.03) were significantly more likely to report near vision difficulty. Uncorrected myopia, corrected hyperopia, and corrected astigmatism were not significantly associated with reporting near vision difficulty. Odds ratios were adjusted for age, sex, income, education level, acculturation score, diabetes, and high blood pressure.
Table 3.
Results of ordinal logistic regression: odds of impairment (falling into a worse score category) by refractive error group, compared to subjects without refractive error
| Near vision impairment | Distance vision impairment | ||||
|---|---|---|---|---|---|
| Refractive error category | Odds Ratio* | 95% CI | Odds Ratio* | 95% CI | |
| No refractive error | Ref | Ref | Ref | Ref | |
| Myopia | Corrected | 0.8 | 0.7-0.9 | 2.00 | 1.7-2.4 |
| Uncorrected | 1.1 | 0.8-1.5 | 3.7 | 2.7-5.2 | |
| Astigmatism | Corrected | 1.0 | 0.7-1.4 | 1.7 | 1.2-2.3 |
| Uncorrected | 1.7 | 1.0-3.0 | 2.4 | 1.4-4.2 | |
| Hyperopia | Corrected | 0.9 | 0.7-1.0 | 1.8 | 1.5-2.2 |
| Uncorrected | 1.6 | 1.2-2.2 | 2.0 | 1.5-2.8 | |
Bolded ORs are significant at p<0.05 after adjustment for age, sex, income, education, diabetes, hypertension, and acculturation.
Acronym and abbreviation key: RE (Refractive Error), OR (Odds Ratio), CI (Confidence Interval), Ref (Reference Category).
In a corresponding model for distance vision function, all subjects with any type of RE, and regardless of correction, were significantly more likely to report distance vision difficulty than subjects without RE (Table 3). This model was adjusted for age, sex, income, education level, acculturation score, diabetes, and high blood pressure.
We conducted sensitivity analyses on our models by altering the choice of cut-offs. The alternative models defined “more difficulty” as a score worse than 60, “mild difficulty” as a score between 60 and 90, and “no difficulty” as a score of 90 or better. Although the alternative cutoffs included more severe impairment in the “no difficulty” and “mild difficulty” groups, the results were consistent in significance and direction with the original results detailed in Table 3 (data not shown).
A similar set of ordinal logistic regression models were created to examine the odds of vision function difficulty in corrected myopia compared to uncorrected myopia, corrected to uncorrected astigmatism, and corrected to uncorrected hyperopia (data not shown). After adjusting for confounders, corrected myopia was associated with significantly less distance vision difficulty than uncorrected myopia (OR 0.53, 95%CI 0.37-0.76), although as found above, even corrected myopia was associated with distance vision difficulty. In another model adjusting for the same covariates, corrected hyperopia was associated with significantly less near vision difficulty then uncorrected hyperopia (OR 0.56, 95%CI 0.40-0.77).
DISCUSSION
URE is known to be associated with decreased quality of life and visual function difficulty. This association has been demonstrated in a variety of populations, using a variety of function assessment tools, including the NEI VFQ-25.7-10 However, to our knowledge, this is the first study to assess the association between correction of myopia, hyperopia, and astigmatism and difficulty with specific subgroups of visual function (near vision and distance vision, as measured by the NEI VFQ-25). As expected, we found that persons with corrected myopia reported better distance vision than uncorrected myopia, and persons with corrected hyperopia reported better near vision than uncorrected hyperopia. Unexpectedly, we also found that any type of RE, either corrected or uncorrected, was associated with significantly worse distance vision function compared to those without RE.
A previous study examining the association of correction, myopia, and hyperopia with quality of life found that only uncorrected myopia was independently associated with a decrease in overall visual function score as well as several independent visually dependent activities.7 In this study, using a different questionnaire that allowed us to score the subgroups of near visual function and distance visual function, we, too, found that subjects with uncorrected myopia have significantly more distance vision difficulty than subjects with corrected myopia or subjects with no refractive error. In contrast to the previous study, we also found that subjects with uncorrected hyperopia had significantly more near vision difficulty compared to those with corrected hyperopia, and that subjects with uncorrected astigmatism or uncorrected hyperopia had more near vision difficulty than subjects with no RE.
Quality of life improvement with correction of refractive error has previously been demonstrated.9,10 However, we found that both corrected and uncorrected RE of any type was associated with distance vision difficulty compared to subjects without RE, although URE was associated with stronger odds of distance vision difficulty than corrected RE of the same type. However, corrected RE remained significantly associated with distance vision difficulty compared to subjects without RE. This finding indicates that correction, at least as found in this study, may not be sufficient to restore distance vision function to the level of those without RE. It is not likely that this effect was due to under correction of RE, since, by definition, everyone with corrected RE had a visual acuity of 20/25 or better. It is possible that there is some aspect of distance visual function that is not completely characterized through visual acuity testing. If this is the case, the distance vision subscore of the NEI VFQ-25 may be able to capture some functional decrement that is not restored with correction, and that might otherwise be missed.
We found that subjects with corrected myopia report less near vision difficulty compared to those without RE (OR 0.78, 95%CI 0.68-0.93). We suspect this phenomenon may be caused by unmeasured near vision impairment in those without RE due to the development of presbyopia with age. People with no RE, and people with myopic RE, would likely both develop presbyopia as they grow older. However, people in this population of Latinos without RE may be less likely to seek eye care for deteriorating near vision alone. They may not be aware of the possibility of presbyopia correction with the purchase and use of reading glasses. On the other hand, when older persons with corrected myopia receive correction of their distance vision impairment, they are likely routinely evaluated for and prescribed additional correction for their developing presbyopia. This hypothesized disparity in the correction of presbyopia may explain the finding of significantly less near vision difficulty in corrected myopia compared to those without RE. Another possible explanation is that those with myopia may have good near vision with simply removing their spectacles, and may consider this as having no or little difficulty with near vision, compared to emmetropes who must still correct their presbyopia and consider the need for correction as indicating more difficulty with near vision. Although the association is not significant, this protective effect is also observed for corrected hyperopia.
We have previously shown that NEI VFQ-25 scores are influenced by demographic factors, including age, gender, level of acculturation, income, education level, as well as comorbidities such as diabetes and hypertension.13 In our analysis, we continue to confirm that these factors are independently associated with near and distance vision function regardless of RE type. Although the NEI VFQ was designed to be vision specific, it is clearly sensitive to other variables, including cultural factors. Thus, it is important to adjust for these, and likely, additional factors when predicting vision difficulty.
We acknowledge some limitations of this study, including the possibility of residual confounding. For example, there is a known association between depression and self-reported functional status, but information on depression status was not collected in our study.15 The absence of near visual acuity testing may be another limitation of our study. The no RE group likely included some subjects with presbyopia, which is consistent with the finding that those with corrected RE tended to have less near vision difficulty than subjects with no RE. If presbyopia had been taken into account, the protective effect of corrected myopia on near vision function may have been nullified. This study was carried out in a population that has limited access to eye care services, and may not be aware of the value even of reading glasses. This issue deserves further follow up.
Another limitation, not unique to our study, concerns the use of NEI VFQ in population-based studies. The distribution of vision function scores was highly skewed with a large ceiling effect. For this reason, we were unable to treat function score as a continuous variable, and decided to create three ordinal score categories by choosing two cutoff values a priori. As a result, people with subtly different levels of vision difficulty may be grouped in the same score category. Additionally, the near and distance vision subscores were based on just three questions, but the validity of these three item domains within our population has previously been examined.
We chose to use spherical error rather than spherical equivalent in this study, although the use of spherical equivalent is more common in studies of RE. In fact, the use of spherical error confers a unique strength to the classification of refractive error in our study. For example, an individual with myopia, but a large positive cylinder, might be classified as emmetropic by spherical equivalent. However, this individual’s myopia would be captured by the use of spherical error, leading to a more appropriate classification in this case. We also recognize that by not using cycloplegic refraction in those under age 50 years we may have underestimated hyperopia. This misclassification would have attenuated our finding of differences between those with hyperopia and those who were classified as emmetropia, thus suggesting that if anything, the differences we did find were even stronger.
Finally, the lack of a standardized definition for myopia, hyperopia, and astigmatism presented a challenge in the classification of subjects in this study. We chose cutoff values based on prior studies as well as expert advice. Certainly, different cutoff values may have produced different results. However, because we chose relatively conservative definitions for inclusion into a refractive error category, any bias in our results would likely be towards the null.
In conclusion, we found that all three types of RE in this study were associated with distance vision difficulty, but only uncorrected astigmatism and uncorrected hyperopia were associated with near vision difficulty. Importantly, we found that, in our population, correction of any type of refractive error is not entirely sufficient to restore distance vision function to the level of those without refractive error. This finding argues for more research investigating the underlying cause for ongoing dissatisfaction in distance visual function after correction of RE.
Uncorrected refractive error is a significant contributor to visual impairment in the United States. The burden of URE within the Latino populations, currently estimated at more than 48 million people, deserves particular attention.16 This study underscores the need for, and the potential positive impact of, programs aiming to reduce the prevalence of uncorrected refractive error in underserved populations such as in the Latino community.
Acknowledgments
Financial support: Research to Prevent Blindness and Core grant NEI 105357. The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Meeting Presentation: The Association for Research in Vision and Ophthalmology Annual Meeting, May, 2011.
Conflict of Interest: No conflicting relationship exists for any author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295:2158–63. doi: 10.1001/jama.295.18.2158. [DOI] [PubMed] [Google Scholar]
- 3.Schneider J, Leeder SR, Gopinath B, et al. Frequency, course, and impact of correctable visual impairment. Surv Ophthalmol. 2010;55:539–60. doi: 10.1016/j.survophthal.2010.02.004. uncorrected refractive error. [DOI] [PubMed] [Google Scholar]
- 4.Uribe JA, Swenor BK, Muñoz BE, West SK. Uncorrected refractive error in a latino population: Proyecto VER. Ophthalmology. 2011;118:805–11. doi: 10.1016/j.ophtha.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muñoz B, West SK, Rodriguez J, et al. Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:608–14. [PubMed] [Google Scholar]
- 6.Smith TS, Frick KD, Holden BA, et al. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ. 2009;87:431–7. doi: 10.2471/BLT.08.055673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamoureux EL, Saw SM, Thumboo J, et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009;50:2614–20. doi: 10.1167/iovs.08-2164. [DOI] [PubMed] [Google Scholar]
- 8.Broman AT, Munoz B, Rodriguez J, et al. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:3393–8. [PubMed] [Google Scholar]
- 9.Coleman AL, Yu F, Keeler E, Mangione CM. Treatment of uncorrected refractive error improves vision-specific quality of life. J Am Geriatr Soc. 2006;54:883–90. doi: 10.1111/j.1532-5415.2006.00817.x. [DOI] [PubMed] [Google Scholar]
- 10.Owsley C, McGwin G, Jr, Scilley K, et al. Effect of refractive error correction on health-related quality of life and depression in older nursing home residents. Arch Ophthalmol. 2007;125:1471–7. doi: 10.1001/archopht.125.11.1471. [DOI] [PubMed] [Google Scholar]
- 11.Mangione CM, Lee PP, Pitts J, et al. NEI-VFQ Field Test Investigators. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ) Arch Ophthalmol. 1998;116:1496–504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 12.Mangione CM, Lee PP, Gutierrez PR, et al. National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–8. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 13.Broman AT, Munoz B, West SK, et al. Psychometric properties of the 25-item NEI-VFQ in a Hispanic population: Proyecto VER. Invest Ophthalmol Vis Sci. 2001;42:606–13. [PubMed] [Google Scholar]
- 14.West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care. 2001;24:1204–9. doi: 10.2337/diacare.24.7.1204. [DOI] [PubMed] [Google Scholar]
- 15.Sinclair PA, Lyness JM, King DA, et al. Depression and self-reported functional status in older primary care patients. Am J Psychiatry. 2001;158:416–9. doi: 10.1176/appi.ajp.158.3.416. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Census Bureau. [October 24, 2011];American FactFinder. Available at: http://factfinder2.census.gov/main.html.


