Abstract
This study aimed to elucidate the efficacy of contrast-enhanced ultrasonography (CEUS) with perfluorobutane (Sonazoid®) in the diagnosis of hepatocellular carcinomas (HCCs), particularly small HCCs, by comparing the results with dynamic computed tomography (Dy-CT). Seventy-nine nodules in 69 patients with chronic liver disease, suspected as HCCs were studied. The nodules were selected based on the results of B-mode ultrasonography and/or Dy-CT conducted between January and August 2007. The nodules were divided into two groups: the S-group with tumors ≤2 cm (49 nodules), and the L-group with tumors >2 cm (30 nodules). Typical HCCs were defined, and the nodules were enhanced and shown as defects in the arterial and late phase of Dy-CT, respectively. Target lesions were scanned using CEUS, and the results were compared with those of Dy-CT. The L-group nodules diagnosed as HCCs using Dy-CT were also diagnosed as HCCs using CEUS. In the S-group, the diagnostic sensitivity of CEUS was 94.7% and the specificity was 81.8%. We diagnosed two liver tumors that were detected by CEUS but not by Dy-CT; biopsies revealed one tumor to be a well-differentiated HCC and the other to be an atypical adenomatous hyperplasia. The sensitivity and specificity of CEUS against HCC were high even in the small-size HCCs. Thus, Sonazoid is useful in the screening for small HCCs.
Keywords: Sonazoid®, perfluorobutane, hepatocellular carcinoma, contrast-enhanced ultrasonography, dynamic computed tomography
Introduction
Dynamic computed tomography (Dy-CT) and conventional B-mode ultrasonography (US) are used for the screening of hepatocellular carcinomas (HCCs). Although Dy-CT is useful for assessing the vascularity of hepatic tumors, negative aspects include exposure to X-rays and the high cost. On the other hand, B-mode US is economical and easy to perform repeatedly. However, some nodules are difficult to identify or diagnose, particularly small-size tumors, due to the sensitivity as well as the irregularity in the case of chronic injured liver.
Recently, the development of US and contrast-enhanced ultrasonographic agents for hepatic tumors have enabled the diagnosis of HCC in the early stage. Perfluorobutane (Sonazoid®) (1) was approved as a new contrast-enhanced ultrasonographic agent in Japan in January 2007. The tumors are phagocyted by Kupffer cells after injection. The primary characteristic of this agent is the ability to maintain observations continuously as the tumors are being phagocyted by Kupffer cells. The present study evaluated the diagnostic efficacy of contrast-enhanced (CE) US with Sonazoid for HCCs, particularly small-size HCCs.
Materials and methods
Seventy-nine nodules detected by US and/or Dy-CT between January and August 2007 in 70 patients examined at Ehime Prefectural Central Hospital, Japan, were studied. Nodules showing the typical findings of liver hemangioma were excluded from this study. Informed consent was obtained from all of the studied patients and the study protocol was approved by the Ethics Committee of Ehime Prefectural Central Hospital.
CEUS was performed within 1 month from the Dy-CT examination in all of the patients. We divided the nodules into two groups. Forty-nine nodules (41 patients) ≤2 cm in diameter were defined as the S-group, and 30 nodules (28 patients) >2 cm in diameter were defined as the L-group. Sonazoid was used as the contrast-enhanced ultrasonographic agent (4 μl/kg of body weight) in all examinations, and the target lesions were scanned after injection in the arterial and Kupffer phases using a ProSound Alpha-10 (Aloka Co. Ltd., Tokyo, Japan). The arterial phase of CEUS imaging was identified 10–60 sec after Sonazoid injection, and the Kupffer phase 10 min after the injection (2). ProSound Alpha-10 was set up in the extended pure harmonic detection mode and was used with a convex type probe (Table I). The results were compared retrospectively between CEUS and Dy-CT. Nodules were diagnosed as typical HCCs by Dy-CT when they were enhanced in the arterial phase and were revealed as a defect in the portal phase of Dy-CT (Fig. 1) (3). Moreover, a nodule was diagnosed as typical HCC, when it was shown as hypervascular in the arterial phase and revealed as a defect lesion in the Kupffer phase (Fig. 2) by CEUS (4,5).
Table I.
Technical background using the extended pure harmonic detection method and ProSound Alpha-10.
| Image | Frequency (MHz) | MI index | Range | Gain | Contrast |
|---|---|---|---|---|---|
| Fundamental | 5.00 | 0.30 | 17 | 60 | 15 |
| Contrast | 1.88 | 0.24 | 17 | 45 | 18 |
MI, mechanical index.
Figure 1.
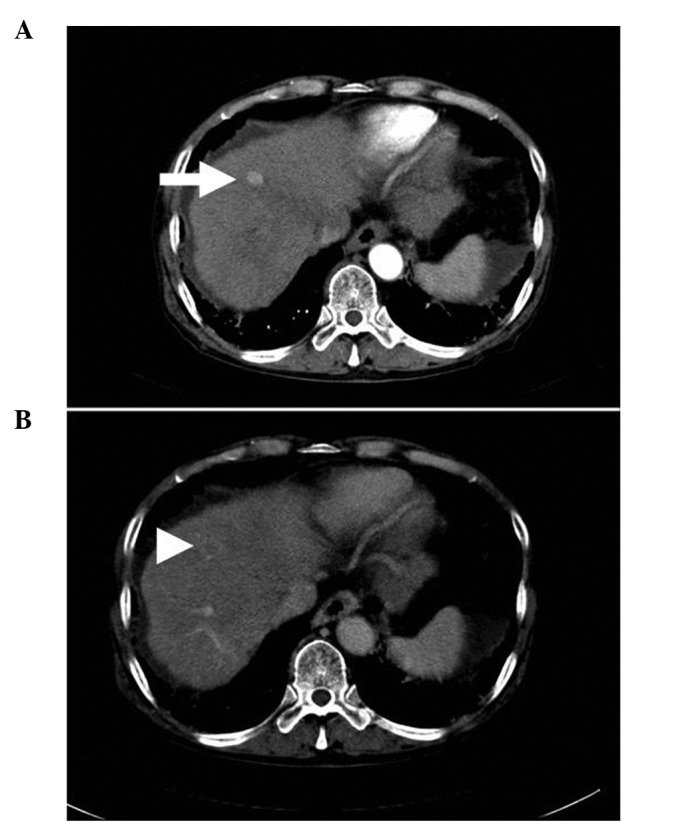
A nodule diagnosed as a typical hepatocellular carcinoma by dynamic computed tomography. (A) The nodule was enhanced in the arterial phase (arrow) and (B) revealed as a defect in the late phase (arrowhead).
Figure 2.
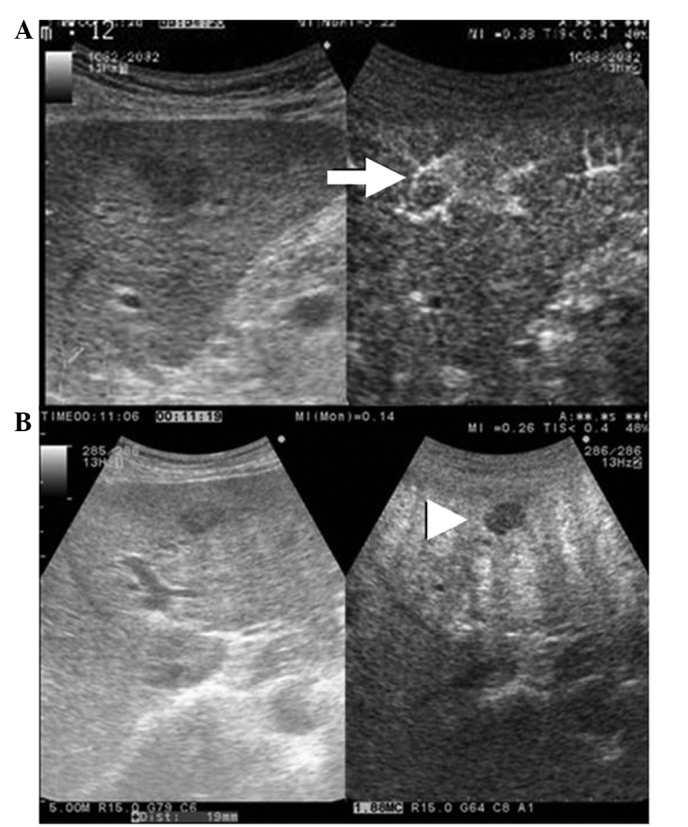
A nodule diagnosed as a typical hepatocellular carcinoma by contrast-enhanced ultrasonography. (A) The nodule was enhanced in the arterial phase (arrow) and (B) revealed as a defect in the Kupffer phase (arrowhead).
Statistical analysis
Statistical analyses were carried out using the Chi-square test with StatView version 5.0 (SAS Institute, Inc., Berkeley, CA, USA). P<0.05 was considered statistically significant.
Results
The average diameter of the S-group nodules was 1.42±0.39 cm (range 0.8–2 cm), while that of the L-group was 3.03±1.10 cm (range 2.1–8 cm). The background of each patient is described in Table II. When typical HCCs using Dy-CT were defined as the gold standard of diagnosing HCCs, the sensitivity and specificity of CEUS with Sonazoid were 97.1% (66/68) and 81.8% (9/11), respectively (Table III). The sensitivity and specificity in the S-group were 94.7% (36/38) and 81.8% (9/11), respectively, while the positive and negative predictive values were 94.7% (36/38) and 81.8% (9/11), respectively. In the L-group, the nodules were diagnosed as HCCs by CEUS, which was identical with the results of Dy-CT.
Table II.
Background of the patients.
| S-groupa | L-groupb | |
|---|---|---|
| Male | 25 | 20 |
| Female | 16 | 8 |
| Mean age (years) | 71.1±7.4 | 71.0±9.0 |
| Positive for anti-HCV | 38 | 21 |
| Positive for HBsAg | 0 | 5 |
| Positive for both anti-HCVAb and HBsAg | 3 | 0 |
| Negative for both anti-HCVAb and HBsAg | 0 | 2 |
| Past history of HCC | ||
| Positive | 16 | 11 |
| Negative | 25 | 17 |
| No. of tumors | 49 | 30 |
| Tumor size (cm) | 1.42±0.39 | 3.03±1.10 |
| AST (IU/l) | 73.6±100.9 | 66.8±42.5 |
| ALT (IU/l) | 52.3±55.9 | 51.4±31.3 |
| T-bil (mg/dl) | 0.92±0.47 | 1.07±0.80 |
| TP (g/dl) | 7.3±0.8 | 7.1±0.7 |
| ALB (g/dl) | 3.7±0.6 | 3.7±0.6 |
| PLT (*104/μl) | 11.8±6.10 | 13.3±8.9 |
| PT (%) | 72.1±10.4 | 74.5±14.4 |
| AFP | 89.4±300.0 | 142.1±360.8 |
HCC diameter ≤2 cm.
HCC diameter >2 cm.
anti-HCV Ab, anti-hepatitis C virus antibody; HBsAg, hepatitis B virus surface antigen; HCC, hepatocellular carcinoma; AST, aspartate aminotransferase; ALT, alanine aminotransferase; T-bil, total bilirubin; TP, total protein; ALB, albumin; PLT, platelets; PT, prothrombin time and AFP, α fetoprotein.
Table III.
Comparison between contrast enhanced ultrasonography and dynamic computed tomography.
| A, All cases. | |||
|---|---|---|---|
|
| |||
| Dy-CT | |||
|
|
|||
| Typical HCC | Not typical HCC | Total | |
| CEUS | |||
| Typical HCC | 66 | 2a | 68 |
| Not typical HCC | 2b | 9 | 11 |
| Total | 68 | 11 | 79 |
|
| |||
| B, S-group. | |||
|
| |||
| Dy-CT | |||
|
|
|||
| Typical HCC | Not typical HCC | Total | |
|
| |||
| CEUS | |||
| Typical HCC | 36 | 2a | 38 |
| Not typical HCC | 2b | 9 | 11 |
| Total | 38 | 11 | 49 |
|
| |||
| C, L-group. | |||
|
| |||
| Dy-CT | |||
|
|
|||
| Typical HCC | Not typical | HCC Total | |
|
| |||
| CEUS | |||
| Typical HCC | 30 | 0 | 30 |
| Not typical HCC | 0 | 0 | 0 |
| Total | 30 | 0 | 30 |
One case was diagnosed as a well-differentiated hepatocellular carcinoma, and the other was diagnosed as an atypical adenomatous hyperplasia by biopsy.
The nodule was located in a deep position.
HCC, hepatocellular carcinoma; CEUS, contrast-enhanced ultrasonography and Dy-CT, dynamic computed tomography.
In the S-group, 2 nodules were detected by CEUS, but were not detected by Dy-CT. On the other hand, 2 nodules were detected by Dy-CT, but not by CEUS. We performed US-guided biopsies in the 2 nodules which were undetected by Dy-CT. One was detected as a mixed echoic nodule with a diameter of 0.8 cm in segment 5 of the liver by B-mode US (male, 63 years of age, positive for anti-HCVAb). This nodule was revealed as a hypervascular lesion in the arterial phase and as a defect in the Kupffer phase. Based on the CEUS findings, the tumor was suspected to be HCC (typical HCC by CEUS). The result of the biopsy identified it as a well-differentiated HCC. The other nodule was revealed to be hypoechoic with a diameter of 1 cm in segment 8 of the liver by B-mode US (female, 81 years of age, positive for anti-HCVAb). The tumor was slightly enhanced peripherally in the arterial phase and was revealed as a partial defect in the Kupffer phase by CEUS. The CEUS findings were not conclusive, and this tumor was unable to be diagnosed as a typical HCC. The result of the biopsy identified it as an atypical adenomatous hyperplasia (AAH). Among the 38 nodules detected by CEUS, the diameter of 8 nodules including the above-mentioned 2 nodules were <1 cm. The other 6 nodules larger by <1 cm were diagnosed as typical HCCs by both Dy-CT and CEUS. One nodule detected by Dy-CT but not by CEUS was located in a deep position from the body surface.
Discussion
Sonazoid is a new agent for CEUS which reveals the arterial flow in tumors. Moreover, malignant hepatic tumors can be observed continuously and repeatedly throughout the examination as a defective area in the Kupffer phase due to the lack of Kupffer cells in tumors (6).
Classic HCC cases have a blood flow from the feeding artery and a decrease in or lack of a portal vein in the tumor, whereas those in the early stage have a portal vein and increased arterial flow. When the diameter of the tumor expands, the portal flow and Kupffer cells decrease in the tumor (7,8). The present study validated the usefulness of CEUS using Sonazoid. We diagnosed all nodules as typical HCCs in cases with tumors >2 cm in diameter (L-group) using CEUS, identical to the results obtained using Dy-CT. Therefore, it was confirmed that the diagnostic ability for detecting HCCs with a diameter >2 cm using CEUS with Sonazoid was identical to Dy-CT.
A small HCC can be difficult to diagnose. We performed CEUS with Sonazoid to evaluate small HCC nodules ≤2 cm in diameter (S-group) and found the sensitivity and specificity to be 94.7 and 81.8%, respectively, while the positive and negative predictive values were 94.7 and 81.8%, respectively. Although the study population was small and the study design was retrospective, the results were encouraging.
The high rates for sensitivity and specificity of CEUS with Sonazoid are thought to depend on the continuous view provided in the Kupffer phase. CEUS with other agents (e.g., Levovist® and SonoVue®) does not reveal the Kupffer phase image continuously for >10 min, as the imaging of the Kupffer phase is performed by bursting microbubbles that accumulate in Kupffer cells by sound waves (9). Continuous viewing in the Kupffer phase image with Sonazoid can be obtained since the images are obtained with vibration, rather than bursting by sound waves, which makes it easy to observe abnormal findings (10).
Wang et al (9) reported on CEUS imaging with Levovist. A combination of the characteristics of arterial phase enhancement and the absence of the Kupffer phase enhancement as determined by CEUS was highly specific for small HCCs in cirrhosis patients. However, the use of CEUS with Levovist is difficult for many operators since the enhancement of the Kupffer phase vanishes immediately, and the scan cannot be conducted continuously. Sonazoid is considered to be superior for the evaluation of hepatic tumors compared with other agents, since nodules that are invisible in B-mode but visible in Dy-CT are not detected in the Kupffer phase with a continuous view due to the character of Sonazoid. the detection of the target lesion, we observed the arterial flow by re-injection into the defect area (11). Hohmann et al reported that SonoVue markedly improved the characterization of focal hepatic lesions in comparison with unenhanced sonography (12). Giorgio et al reported that the enhancement pattern related to tumor hypervascularity as well as sensitivity and specificity with SonoVue were high for nodules 1–3 cm in diameter, whereas these were very low (sensitivity, 27.3%; specificity, 100%) for nodules <1 cm (13).
In the present study, 8 nodules were <1 cm and detectable by CEUS with Sonazoid. Two nodules, which were invisible by Dy-CT but visible in the Kupffer phase of CEUS, were diagnosed as a well-differentiated HCC and an AAH. This indicates that certain HCC nodules which are not detectable by Dy-CT may be detectable by CEUS. The characteristics of these nodules should be investigated. Although these 2 nodules were diagnosed by biopsy, another 6, which were <1 cm, were diagnosed as typical HCCs by CEUS with Sonazoid.
There are several negative aspects associated with CEUS, such as the difficulty in discerning lesions deeply positioned, liver surface lesions confirmed by US, and lesions located in the blind spot. In addition, the internal echo is very irregular in the case of chronic liver injury. While all nodules of the L-group were detected by CEUS, 2 nodules in the S-group were not as they were located in a deep position. The diagnostic efficacy for small HCCs is evident when understanding the characteristics and disadvantages of CEUS particularly in the Kupffer phase.
In conclusion, the low cost and non-invasive characteristics of CEUS with Sonazoid are useful in screening examinations and for diagnosing small HCCs.
References
- 1.Sontum PC. Physiochemical characteristics of Sonazoid, a new contrast agent for ultrasound imaging. Ultrasound Med Biol. 2008;34:824–833. doi: 10.1016/j.ultrasmedbio.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Watanabe R, Matsumura M, Chen CJ, et al. Characterization of tumor imaging with microbubble-based ultrasound contrast agent, sonazoid, in rabbit liver. Biol Pharm Bull. 2005;28:972–977. doi: 10.1248/bpb.28.972. [DOI] [PubMed] [Google Scholar]
- 3.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe R, Matsumura M, Munrmasa T, et al. Mechanism of hepatic parenchyma-specific contrast of microbubble-based contrast agent for ultrasonography: microscopic studies in rat liver. Invest Radiol. 2007;42:643–651. doi: 10.1097/RLI.0b013e31805f2682. [DOI] [PubMed] [Google Scholar]
- 5.Kindberg GM, Tolleshaug H, Roos N, et al. Hepatic clearance of Sonazoid perfluorobutane microbubbles by Kupffer cells does not reduce the ability of liver to phagocytose or degrade albumin microspheres. Cell Tissue Res. 2003;312:49–54. doi: 10.1007/s00441-003-0698-0. [DOI] [PubMed] [Google Scholar]
- 6.Kudo M. New sonographic techniques for the diagnosis and treatment of hepatocellular carcinoma. Hepatol Res. 2007;37(Suppl 2):193–199. doi: 10.1111/j.1872-034X.2007.00184.x. [DOI] [PubMed] [Google Scholar]
- 7.Nakashima O, Sugihara S, Kage M, et al. Pathomorphologic characteristics of small hepatocellular carcinoma: a special reference to small hepatocellular carcinoma with indistinct margins. Hepatology. 1995;22:101–105. [PubMed] [Google Scholar]
- 8.Matsui O, Kadoya M, Kameyama T, et al. Benign and malignant nodules in cirrhotic livers: distinction based on blood supply. Radiology. 1991;178:493–497. doi: 10.1148/radiology.178.2.1846240. [DOI] [PubMed] [Google Scholar]
- 9.Wang JH, Lu SN, Hung CH, et al. Small hepatic nodules (< or =2 cm) in cirrhosis patients: characterization with contrast-enhanced ultrasonography. Liver Int. 2006;26:928–934. doi: 10.1111/j.1478-3231.2006.01318.x. [DOI] [PubMed] [Google Scholar]
- 10.Numata K, Morimoto M, Ogura M, et al. Ablation therapy guided by contrast-enhanced sonography with Sonazoid for hepatocellular carcinoma lesions not detected by conventional sonography. Ultrasound Med. 2008;27:395–406. doi: 10.7863/jum.2008.27.3.395. [DOI] [PubMed] [Google Scholar]
- 11.Minami Y, Chung H, Kudo M, et al. Radiofrequency ablation of hepatocellular carcinoma: value of virtual CT sonography with magnetic navigation. Am J Roentgenol. 2008;190:W335–W341. doi: 10.2214/AJR.07.3092. [DOI] [PubMed] [Google Scholar]
- 12.Hohmann J, Skrok J, Puls R, et al. Characterization of focal liver lesions with contrast-enhanced low MI real time ultrasound and SonoVue. Rofo. 2003;175:835–843. doi: 10.1055/s-2003-39923. [DOI] [PubMed] [Google Scholar]
- 13.Giorgio A, De Stefano G, Coppola C, et al. Contrast-enhanced sonography in the characterization of small hepatocellular carcinomas in cirrhotic patients: comparison with contrast-enhanced ultrafast magnetic resonance imaging. Anticancer Res. 2007;27:4263–4269. [PubMed] [Google Scholar]


