Abstract
Objective:
To evaluate the prevalence of parasitic and bacterial infestations among food handlers.
Design:
Retrospective study.
Setting:
Food handlers working in the Military food serving facilities in Jubail (Eastern Province of Saudi Arabia).
Method:
The stool samples of 881 food handlers of different nationalities were examined at the Armed Forces Hospital laboratory using the concentration method.
Results:
A total of 194 (20%) of the workers tested positive for enteric microbial infestation. Helminths were the most prevalent, infecting 93 (10.56%) of the food handlers; followed by protozoa which affected 65 (7.38%) food handlers; and the smallest group was infected with bacteria in 44 (4.9%) of the food handlers. Not only single organism infection was seen (83.94%), but also double (14.51%) and triple (1.55%) infections. Among the Helminths, Ascaris lumbricoides was the most prevalent with 33 (47.14%) cases, Giardia lamblia was the most prevalent Protozoa with 23 (43.40%) cases, and Salmonella was the most prevalent bacteria with 34 (87.18%) cases. Expatriates from South Asia showed a significant rate of infection when compared to expatriates from Arabian countries. The Bangladeshi food handlers were of the greatest prevalence of infection with 151 (17.14%) cases, followed by Indian workers with 17 (1.93%) cases, and Pakistani workers with 11 (1.25%).
Conclusion:
The study stresses the importance of regular check-ups and prompt treatment of infected food handler.
Keywords: Food handler, intestinal parasite, food inspection, bacterial infection
INTRODUCTION
Food handlers, particularly those handling unwrapped food which is to be consumed uncooked, play a significant role in the transmission of food-borne microbial diseases. Symptomatically ill food handlers can easily be detected and excluded from work duties which involve working directly with food products, however, the danger lies in the food handlers who do not show any symptoms.
Therefore, it is extremely important to have regularly scheduled check-ups so that infected employees can be immediately excluded from work involving direct contact with food products and can be appropriately treated.
The Armed Forces Hospital at King Abdulaziz Naval Base in Jubail (Eastern Region of Saudi Arabia) is responsible for providing medical services to all Military personnel who are stationed within a 50 kilometer radius in addition to the personnel stationed at the Naval Base itself. One of the responsibilities of the Preventive Medicine Department at the hospital is to screen all food handlers who are employed at any of the food service facilities within this area. To be sure that the food handlers are medically fit, check-ups are done upon employment and then twice annually thereafter. The subject of investigating intestinal infestations among food handlers had been studied in different parts of the Kingdom previously.1,2 However, in this study, the author is presenting another experience from the eastern region of Saudi Arabia. The objective of this investigation is to assess the enteric microbial (parasitic and bacterial) infestations in food handlers in Jubail.
MATERIALS AND METHODS
Within the 50 kilometer radius of the Naval Base, there are several military installations and within each of these areas there is one, or more, food service facility. Satellite clinics have been set up in each of these areas and it is the responsibility of the doctor at each clinic to screen and examine all the food handlers who work in the respective installation and forward a report on these employees to the Preventive Medicine Department.
One of the main screening tests for the food handlers is a stool examination. During the period of time from December 1993 to November 1994, three fresh specimens of feces were obtained on three consecutive days from each of a total of 881 food handlers. Each of these specimens were stained with Lugol's iodine solution and were then examined under light microscopy within approximately one hour from the time of collection (using the Ridley-Allen modified formol-ether concen-tration method).3 All examinations were done by one microbiology technician. The food handlers who were found to have parasites were then excluded from handling food until they had completed the appropriate treatment and their stool specimens were free from parasites. All the laboratory results were then entered into the Epi Info (the public domain software for Epidemiology and disease surveillance). The statistical test used by Epi Info were Chi Square and Fisher exact.
RESULTS
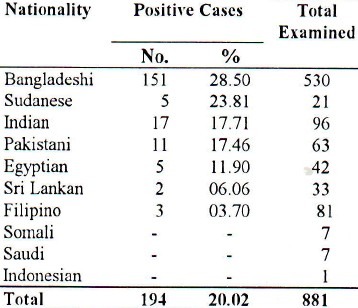
Stool specimens were examined from a total of 881 food handlers. Table 1 shows the distribution of the food handlers in terms of nationality and enteric pathogen infections which were prevalent. The overall prevalence of intestinal parasitic and bacterial infestation among the food handlers was 20% (194 of 881) (some workers were infected with more than one organism). Bangladeshi workers had the highest percentage of infection (28.5%), followed by Sudanese (23.8%), Indians (17.7%) and the Pakistanis (17.4%). The lowest rate of infection was among food handlers from the Philippines (3.7%). Workers from Somalia, Indonesia and Saudi Arabia were free of any enteric infection. Although the number of food handlers from these three nationalities was small (15); there was a statistical significant difference in the rate of infection (Fisher exact: 2-tailed P=0.05).
Table 1.
Prevalence of food-borne microbial disease anrongfood handlers in Jubail, Eastern Region of Saudi Arabia based on their nationalities
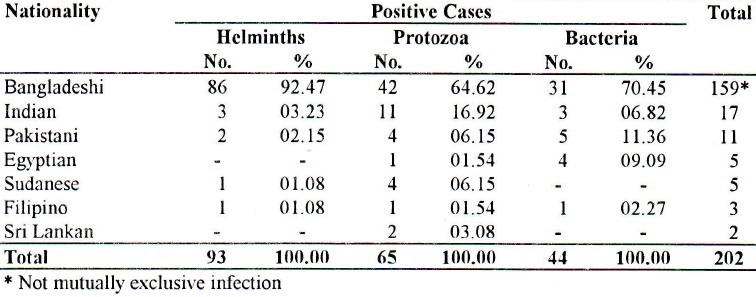
Among the three classes of enteric microbial, Helminths had the highest rate of infection among the food handlers (46.04%), followed by Protozoa (32.18%) and the least were enteric bacteria (21.78%).
Bangladeshi food handlers had the highest infection rate in all three classes (Table 2)- Helminths (92.47%), Protozoa (64.62%), and Enteric Bacteria (70.45%). The Indian workers had the next highest infection rate in Helminths (3.23%) and in protozoa (16.92%). For the enteric bacteria, the Pakistani workers had the second highest rate of infection (11.36%).
Table 2.
Distribution of the infecting organisms among different nationalities of food handlers in Jubail
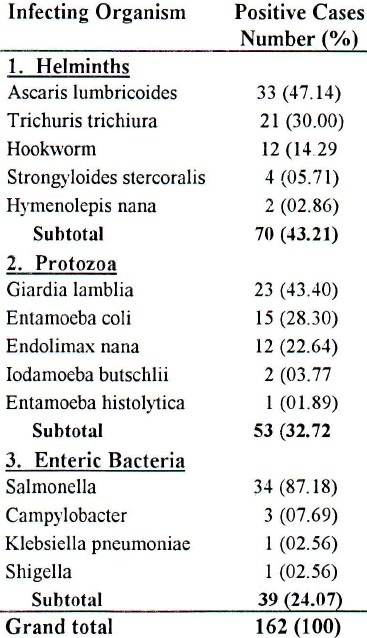
A. Lumbricoid was found to be the most prevalent helminth (47.14%) among the food handlers, followed by T. Trichuria (30%). The most prevalent protozoa among the food handlers was G. lamblia, constituting 43.40%, followed by E. Coli at 28.30%. On the other hand, salmonella was the most prevalent gram-negative enteric bacteria seen in food handlers (87.18%), followed by campylobacter (7.69%) as shown in Table 3. The single organism infection was seen in 162 workers (83.94%) of the total number of infected food handlers which is 194 of all the food handlers examined (881).
Table 3.
Distribution of the single infecting organism in food handlers in Jubail
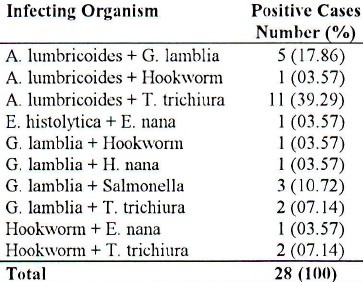
Double infection with A. lumbricoides and T. trichuria was the most prevalent of the double enteric infections (Table 4), followed by A. lumbricoides plus G. lamblia combination (17.86%), and G. lamblia plus salmonella at 10.72%. The double organism infection constituted 14.51%of all the infected workers (28 food handlers).
Table 4.
Distribution of the double infectionion organisms in food handlers in Juhoil
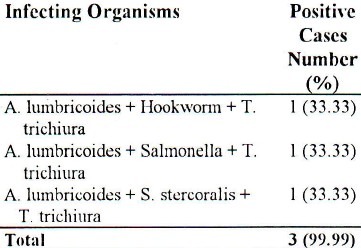
Triple infection (A. lumbricoides and T. trichiura and either hookworm or salmonella or S. stercoralis) was also noted, but in only three of the 881 food handlers who were examined (1.55%). A combination of A. lumbricoides and T. trichiura was common for all the three cases (Table 5).
Table 5.
Distribution of the triple infection organisms in food handlers in Jubail
Because the number of food handlers of some nationalities was not big enough for statistical analysis; the Arabians were pooled together (N=77) in one group and the South East Asian (N=804) in another group. Ten out of 881 (1.14%) Arabians showed intestinal infestations in comparison to 184 (20.89%) of the latter. This difference was statistically significant (Chi Square = 4.01 with P = 0.045).
DISCUSSION
Since the implementation of routine clinical bi-annual check-ups (July 1993) on all of the food handlers, the Armed Forces Hospital, Jubail, has not received any case of food poisoning. This includes all of the Military's food serving facilities. Despite this fact, the screening for 1994 has shown a significant rate of enteric infestation (20%) among food handlers working in these areas. This is a high prevalence compared to what others1,2 have reported, which is explained by the fact that in this study bacterial and nonpathogenic parasites were included as well. Cruickshank4 stated that apart from Salmonella typhi and S. paratyphi, there have been no reports of food poisoning which incriminated a food handler source.
In this study, most of the food handlers were either Bangladeshi, Indian or Pakistani (78.2%). This ratio of workers is generally found throughout the Kingdom of Saudi Arabia.1 Most of these workers are examined upon their arrival to Saudi Arabia. However, after medical attention is given to them, they may harbor these enteric infections throughout their stay in the Kingdom, depending on their personal hygiene. Therefore personal hygiene plays a major role in the incidence of enteric microbial infection as these arc transmitted via the feco-oral route.1,5,6 Another factor which encourages the growth of these microbes is the climate environment which is extremely hot and humid throughout much of the year.2
There was no intestinal infestation found among the Saudi, Somali and Indonesian workers. Though the number of food handlers from these three nationalities was small in comparison to the other nationalities; the difference in infection rate was statistically significant (Fisher exact P=0.05 two tailed). Khan1 also reported no parasitic infection among Indonesian food handlers. The high prevalence of intestinal infestation among Bangladeshi and Indian food handlers was consistent with other studies.2
Because the number of infected food handlers of some of the nationalities was less than five, the investigator combined some of the nationalities for the sake of statistical analysis only.7 Therefore, for this combination to be logical, the Arabians were combined as one group, and the South East Asians were combined as another group. The result showed a significant difference in the infection rate between the two groups (with P=0.045 Chi square = 4.01). Ali et al2 report similar findings in Al-Medinah.
The helminths infection was more common than those due to protozoa or bacteria. This pattern is different from that reported by Siddiqui et al8 who reported protozoa being more common than helminths and Ghandour et al9 in cases examined in the Western region of Saudi Arabia and by Nasher10 in the Southern region. The helminths infections were the most prevalent of the three microbial classes among Bangladeshi workers. Whereas the protozoa were the most prevalent class of microbial infections among Indian, Sri Lankan and Sudanese workers. The enteric bacterial infections were most prevalent among Egyptian, Filipino and Pakistani workers. This may be explained by the endimicity of the respective microbes in the worker's country of origin.
Not only single organism infection, but also double and triple organism infection was seen in this study. A. lumbricoides and T. trichiura, as a combination, were seen in all three cases of triple infection. These findings are not unique. Abdel-Hafez11 reported double and triple parasitic infestations in expatriates in Riyadh. In addition, Qadri and Khalil12 reported multiple parasites among patients at King Faisal Specialist Hospital.
A. lumbricoides was the most prevalent helminth followed by T. trichiura and hookworm. This is consistent with what Khan and his colleagues1 have reported from Dammam. However, Ali and his colleagues2 reported that in Al-Madinah there was more T. trichiura than A. lumbricoides. Among the protozoa, G. lamblia was the highest followed by E. coli and E. nana in this study. This is consistent with many reports within the Kingdom2,5,11 and outside.13,14
Salmonella was the commonest among the enteric bacterial infections in this study. Salmonella is considered the major cause of food poisoning,15 and therefore, special attention was given to these cases. Telzak16 reported 42% infection with salmonella among the 404 admitted patients when a nosocomial outbreak occurred due to contaminated eggs, resulting in a 3% fatality rate.
RECOMMENDATIONS
Routine check-ups should be conducted on all food handlers at a minimum rate of once yearly, but preferably bi-annually. The appropriate medical treatment should then be administered to hose workers who are found to be infected.
If a food handler is symptomatic or is found to be a carrier of salmonella, the worker should not be allowed to do any duty that involves handling of food products until such time as the worker is found to be free from infection.
The health area clinics should be responsible for using the Catchment Centers as a centralized area in which all of the incoming workers can be tested and treated for any infections they may have upon entering the Kingdom.
Statistical data on these food handlers should be gathered and analyzed Kingdom-wide.
ACKNOWLEDGMENT
The author thanks Prof. Ibrahim E., for the editing and Mrs. Jenifer Johnson for typing the manuscript.
REFERENCES
- 1.Khan ZH, Al-lama AA, Madani I. Parasitic Infections Amongst Food Handlers in Dammam and Al-Khobar, Saudi Arabia. Ann Saudi Med. 1987;7:47–50. [Google Scholar]
- 2.AIi SI, Jamal K, Qadri SM. Prevalence of Intestinal Parasites Among Food Handlers in Al-Medinah, Saudi Arabia. Ann Saudi Med. 1993;12(1):63–6. doi: 10.5144/0256-4947.1992.63. [DOI] [PubMed] [Google Scholar]
- 3.Stokes EJ, Ridgway GL, Wren MWD. Clinical Microbiology. 7th Edn. London: Edward Arnold; 1993. p. 209. [Google Scholar]
- 4.Cruickshank JG. Food Handlers and Food Poisoning. Br Med J. 1990;300:207–8. doi: 10.1136/bmj.300.6719.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Madani AA, Omar MS, Abu-Zeid HA, Abdulla SA. Intestinal Parasites in Urban and Rural Communities of Abha, Saudi Arabia. Ann Saudi Med. 1989;9(2):182–5. [Google Scholar]
- 6.Jawetz E, Melnick JL, Adelberg EA. Review of Medical Microbiology. 14th edn. California: Lange Medical Publication; 1980. pp. 556–9. [Google Scholar]
- 7.Daniel WW. Biostatistics: A Foundation for Analysis in the Health Sciences. 2nd Edn. New York: John Wiley & Sons; 1978. p. 359. [Google Scholar]
- 8.Siddiqui MA, Affifi IH, Edeson JF. Survey of Intestinal and Urinary Parasitic Infections at King Abdulaziz University Hospital, Jeddah, Saudi Arabia. King Abdulaziz University Med J. 1982;2(1):35–44. [Google Scholar]
- 9.Ghandour AM, Zahid NZ, Banajee A, Kamal K, Boug A. Zoonotic intestinal parasites of hamadry-as baboons papio hamadry-as in the western and northern regions of Saudi Arabia. Journal of Tropical Medicine and Hygiene. 1995;98:431–439. [PubMed] [Google Scholar]
- 10.Nasher AK. Zoonotic parasitic infections of the Arabian Baboon papio hamadry-as Arabices Thomsas in Asir Province. Annals de Parasitologia Humaine et Comparee. 1988;63:448–454. doi: 10.1051/parasite/1988636448. [DOI] [PubMed] [Google Scholar]
- 11.Abdel-Hafez MA, El-Kady N, Noah MS, Bolbol A. Parasitic Infestation in Expatriates in Riyadh, Saudi Arabia. Ann Saudi Med. 1987;7(3):202–6. [Google Scholar]
- 12.Qadri SH, Khalil S. Intestinal Parasites: Incidence and Etiology in over 1,000 patients in King Faisal Specialist Hospital in Riyadh, Saudi Arabia. Ann Saudi Med. 1987;7(3):207–11. [Google Scholar]
- 13.Faust EC, Beaver PC, Jung RC. Animal Agents & Vectors of Human Disease. 4th Edn. Philadelphia: Lea & Fibiger; 1975. p. 25. [Google Scholar]
- 14.Cevallos AM, McHugh TD, Carnaby S, Farthing JG. Phenotypic and Genotypic Variation in Gardia Lamblia. Saudi Med J. 1991;12(4):285–9. [Google Scholar]
- 15.Mitchel JE, Skelton MM. Diarrheal Infections. Am Fam Physician. 1988;37(5):195–207. [PubMed] [Google Scholar]
- 16.Telzak EE, Budnick LD, Greenberg MSZ, Blum S, Shayegani M, Benson CE, Schultz S. A Nosocomial Outbreak of Salmonella enteritidis Infection Due to the Consumption of Raw Eggs. N Engl J Med. 1990;323(6):394–397. doi: 10.1056/NEJM199008093230607. [DOI] [PubMed] [Google Scholar]


