Abstract
Objective:
To evaluate factors that may contribute to the increased stroke case fatality rates observed in individuals from low-income areas.
Methods:
We conducted a cohort study on a population-based sample of all patients with stroke or TIA seen at 153 acute care hospitals in the province of Ontario, Canada, between April 1, 2002, and March 31, 2003, and April 1, 2004, and March 31, 2005. Socioeconomic status measured as income quintiles was imputed from median neighborhood income. In the study sample of 7,816 patients we determined 1-year mortality by grouped income quintile and used multivariable analyses to assess whether differences in survival were explained by cardiovascular risk factors, stroke severity, stroke management, or other prognostic factors.
Results:
There was no significant gradient across income groups for stroke severity or stroke management. However, 1-year mortality rates were higher in those from the lowest income group compared to those from the highest income group, even after adjustment for age, sex, stroke type and severity, comorbid conditions, hospital and physician characteristics, and processes of care (adjusted hazard ratio for low- vs high-income groups, 1.18; 95 confidence interval 1.03 to 1.29).
Conclusions:
In Ontario, 1-year survival rates after an index stroke are higher for those from the richest compared to the least wealthy areas, and this is only partly explained by age, sex, comorbid conditions, and other baseline risk factors.
Many studies have demonstrated that socioeconomic status is an important predictor of overall health, disease-specific mortality, and health care utilization.1–4 These findings have been observed in multiple jurisdictions, and in countries with and without publicly funded universal health care. Differences in health outcomes, including stroke incidence, mortality, and case-fatality rates, appear to be driven not only by individual-level socioeconomic status, but also by community and neighborhood socioeconomic profiles.4–22
Theoretical explanations for the association between socioeconomic status and disease-specific case fatality rates include differences in disease severity, differential access to or use of effective treatments, differences in response to therapy, differences in baseline risk, differences in health behaviors such as exercise and diet, or differences in community resources.23–25 However, the existing literature provides little information on which, if any, of these factors are most responsible for the observed effect of socioeconomic status on mortality after stroke. Identification of the relevant factors is a necessary first step for the development of interventions to address socioeconomic-related disparities in stroke outcomes.
In this study we use data from a clinical database, the Registry of the Canadian Stroke Network, to determine whether socioeconomic status, defined as neighborhood income group, is associated with differences in baseline risk factors, stroke type, stroke severity, or hospital-based processes of stroke care; and to what extent these differences in baseline factors and processes of care contribute to differences in survival across socioeconomic groups.
METHODS
Data sources and patient sample.
The Registry of the Canadian Stroke Network (RCSN) performs a periodic audit of stroke care delivery on a random sample of all patients with stroke or TIA seen in the emergency department or admitted to any acute care institution in the province of Ontario, Canada.26 Stroke/TIA separations are identified from the discharge abstract database (DAD) and the National Ambulatory Care Reporting System (NACRS) databases maintained by the Canadian Institute for Health Information (CIHI), using International Classification of Diseases (ICD)–10 codes I60, I61, I63, I64, and G45 (excluding G45.4) in the primary diagnosis position. By law in Ontario, all hospitals and emergency department separations are included in the CIHI database, so the sampling frame is population-based. From all eligible cases, a simple random sample of approximately 15% is audited, through retrospective chart abstraction by centrally trained neurology research nurses. Data are collected on all aspects of acute stroke management, including patient demographics, the use of prehospital emergency medical services, stroke type and presentation, in-hospital stroke care (investigations, consultations, medications, other interventions), discharge disposition, length of stay, and in-hospital mortality. The aggregate anonymized database is managed at the coordinating center for the RCSN at the Institute for Clinical Evaluative Sciences (ICES) in Ontario, Canada. Chart validation by duplicate chart abstraction has shown excellent agreement (κ score or intraclass correlation coefficient of greater than 0.9) for key variables including age, sex, and use of thrombolysis.26 The data collection software forces chart abstraction personnel to perform complete data entry before the case record can be submitted for inclusion in the database, ensuring that there are no missing data.
We used data from patients seen between April 1, 2002, and March 31, 2003, and between April 1, 2004, and March 31, 2005. The audits captured both incident and recurrent stroke but, for patients with more than 1 stroke event during the study period, only the first event was included in the present analyses. Patients with a final diagnosis of nonstroke or subarachnoid hemorrhage were excluded, as were those with strokes that occurred as an in-hospital complication, those with invalid postal codes, and those where income quintile could not be determined. Using unique encrypted patient identifiers, we linked the RCSN database to the Ontario Registered Persons Database to obtain information on 30-day and 1-year mortality after stroke, regardless of place of death.
Assessment of socioeconomic status.
We aimed to explore the relationship between community rather than individual-level socioeconomic status on stroke mortality. Therefore, we used the 2001 and 2006 Canada Census database to impute socioeconomic status using aggregate level measures of income for audit data from 2002–2003 and 2004–2005, respectively. Within the Census data, we calculated the median income in each dissemination area (which contains 400 to 700 persons), and divided neighborhoods into income quintiles, with quintiles 1 and 5 having the lowest and highest median incomes, respectively.2 The dissemination area is the smallest geographical unit used for reporting census data, and has been shown to provide a better estimate of individual-level socioeconomic status than larger reporting areas.27 Each patient from the RCSN was linked to the dissemination area of his or her principal residence using the Statistics Canada Postal Code Conversion File. Following initial analyses using all 5 income quintiles, in order to simplify presentation of the results, the 2 lowest income quintiles were combined to create a “low-income” group, quintiles 3 and 4 were combined to create a “middle-income” group, and quintile 5 was designated as the “high-income” group.
Severity of illness and comorbid illness.
Stroke severity was recorded in the RCSN database using the Canadian Neurological Scale, which measures level of consciousness, orientation, language, and motor function, and ranges from 0 (most severe deficit) to 11.5 (no deficit), and has been shown to be valid and reliable even when done by retrospective chart abstraction.28 Many individual comorbid conditions and stroke risk factors were recorded in the database, however, certain risk factors, such as obesity, diet, exercise, and quantification of alcohol consumption, were not available. Comorbid illness was summarized according to the Charlson-Deyo comorbidity index score, which is a weighted summary score based on the presence or absence of 17 medical conditions, where a score of zero indicates that no comorbid illness is present and higher scores indicate a greater burden of comorbidity.29
Statistical analysis.
Baseline patient characteristics and use of stroke care interventions were compared across income groups using χ2 tests for categorical variables and analysis of variance and Kruskal-Wallis tests for continuous variables. Kaplan-Meier curves were created for survival after stroke by income group. Cox proportional hazards models were developed to determine the relationship of neighborhood income to 30-day and 1-year mortality, with adjustment for multiple prognostic factors, and with the low- and medium-income groups compared to the high-income group (reference category). Covariates were sequentially modeled to examine changes in the income-mortality gradient after adjusting for 1) demographic factors (age and sex); 2) comorbid conditions (diabetes, hypertension, atrial fibrillation, smoking, and previous myocardial infarction); 3) stroke severity (Canadian Neurological Scale score categorized as greater than or equal to 8, 5 to 7, or less than or equal to 4); 4) stroke type (ischemic, intracerebral hemorrhage, undetermined) or TIA; 5) processes of care, including type of hospital (teaching, large community, small community), most responsible physician (neurologist vs other), and care on an acute stroke unit; and 6) rural vs urban patient residence. Income group was treated as a categorical variable (“low,” “middle,” or “high” income). The assumptions of the proportional hazards model were verified using the no time-varying effect. The protective effect of neighborhood income on mortality was calculated using the formula [(adjusted β − unadjusted β)/unadjusted β × 100%], where adjusted β refers to the β coefficient obtained from multivariable Cox proportional hazards modeling, and unadjusted β refers to the β coefficient obtained from univariate Cox proportional hazards modeling.30 Bootstrapping methods (1,000 bootstrap samples) were used to estimate 95% confidence intervals around the relative changes in the protective effect of income on mortality rates. SAS version 9.2 was used for all analyses.
Standard protocol approvals, registrations, and patient consents.
The RCSN is “prescribed” under Ontario's Personal Health Information Protection Act, and patient data are collected without consent for the purpose of facilitating the provision of stroke care in the province of Ontario. The overall project is approved by the Research Ethics Board of Sunnybrook Health Sciences Centre.
RESULTS
The 2002–2003 and 2004–2005 RCSN Ontario Stroke Audits included 8,463 patients with stroke or TIA. After exclusions (241 with nonstroke, 263 with subarachnoid hemorrhage, 96 with in-hospital strokes, 7 with invalid postal codes, and 40 with missing income data), 7,816 were retained for the current analyses. Overall, 51% were women and the mean age was 73 years (table 1). Higher income was associated with being male, married, English or French-speaking, nonsmoking, and having a lower prevalence of diabetes mellitus (table 1). Stroke type was similar across income groups, except that those in the low-income group were less likely than those in the higher income groups to present with TIA (table 2). There were no significant differences in stroke severity by income groups, based on either mean Canadian Neurological Scale scores or the proportion of patients with Canadian Neurological Scale scores greater than or equal to 8 (table 2). Income was not associated with rates of use of ambulance services, and, among those arriving by ambulance, transport times were similar across income groups. Despite this, higher socioeconomic status was associated with a shorter duration between stroke onset and hospital arrival (table 2).
Table 1.
Baseline characteristics of patients by income group
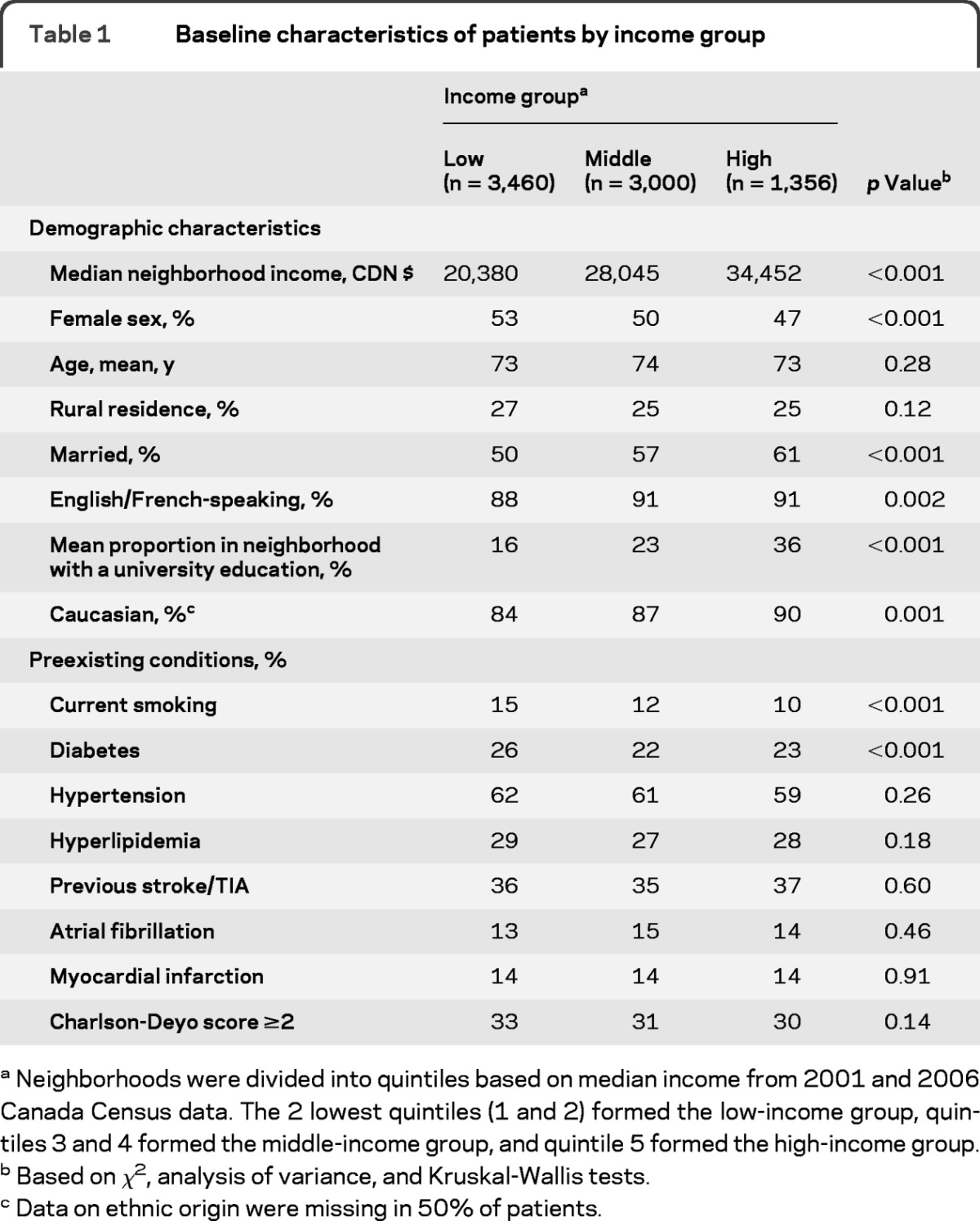
Neighborhoods were divided into quintiles based on median income from 2001 and 2006 Canada Census data. The 2 lowest quintiles (1 and 2) formed the low-income group, quintiles 3 and 4 formed the middle-income group, and quintile 5 formed the high-income group.
Based on χ2, analysis of variance, and Kruskal-Wallis tests.
Data on ethnic origin were missing in 50% of patients.
Table 2.
Stroke presentation, management, and outcomes by income quintile
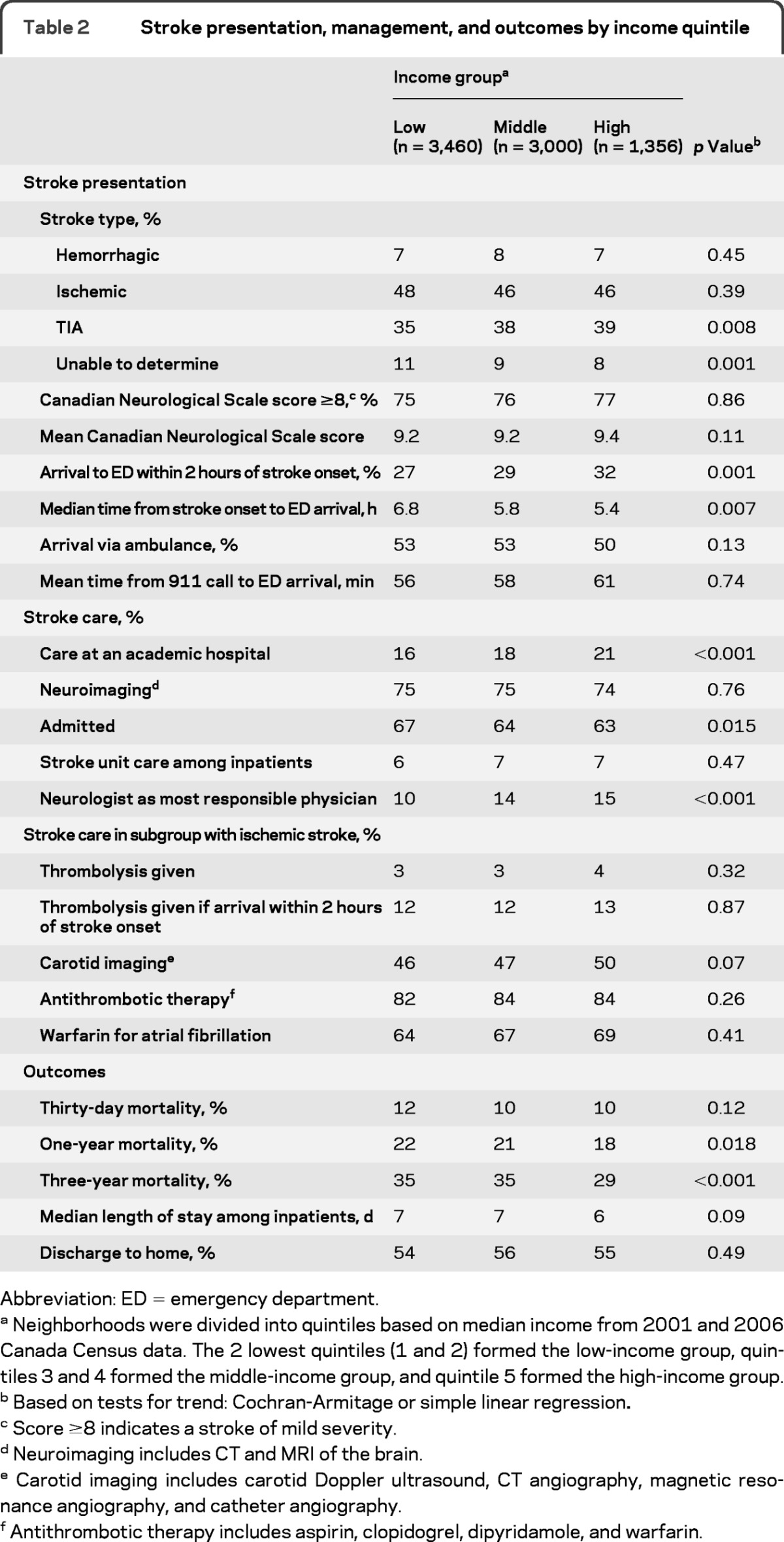
Abbreviation: ED = emergency department.
Neighborhoods were divided into quintiles based on median income from 2001 and 2006 Canada Census data. The 2 lowest quintiles (1 and 2) formed the low-income group, quintiles 3 and 4 formed the middle-income group, and quintile 5 formed the high-income group.
Based on tests for trend: Cochran-Armitage or simple linear regression.
Score ≥8 indicates a stroke of mild severity.
Neuroimaging includes CT and MRI of the brain.
Carotid imaging includes carotid Doppler ultrasound, CT angiography, magnetic resonance angiography, and catheter angiography.
Antithrombotic therapy includes aspirin, clopidogrel, dipyridamole, and warfarin.
Patients in the high-income group were more likely than those in the lower income groups to be seen at academic institutions (21%, 18%, and 16% for the high-, middle-, and low-income groups, respectively; p < 0.001) and to be cared for by a neurologist during hospital admission (15%, 14%, and 10% for the high-, middle-, and low-income groups, respectively; p < 0.001) (table 2). There was no difference based on income group in the use of neuroimaging, admission to a stroke unit, thrombolysis, antithrombotic therapy for ischemic stroke, or warfarin for ischemic stroke with atrial fibrillation (table 2).
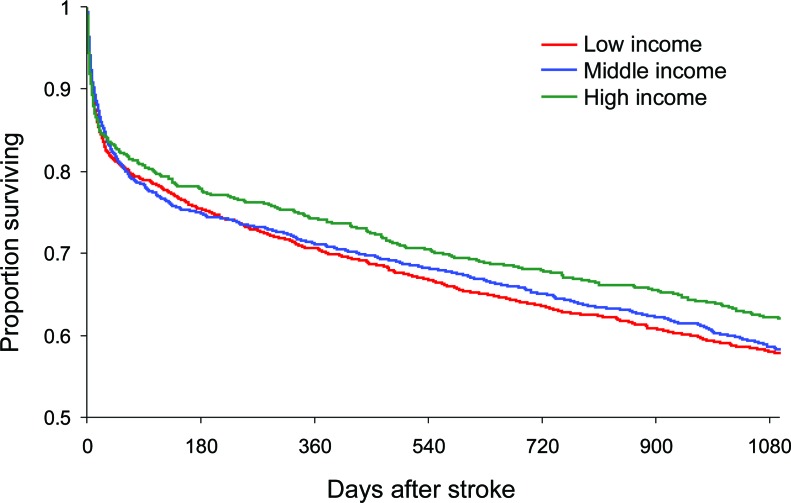
The overall crude 30-day and 1-year stroke mortality rates were 11% and 21%, respectively (table 2). There was no income-mortality gradient in survival at 30 days, however, at 1 year there was a survival advantage for those in the high-income group compared to the 2 lower income groups (figure). The difference in survival at 1 year persisted in the low- compared to the high-income group, even after adjustment for age, sex, comorbid conditions, and stroke type and severity (adjusted hazard ratio [HR] 1.18; 95% confidence interval [CI] 1.03 to 1.36), but was no longer significant for the middle- compared to the high-income group (adjusted HR 1.11; 95% CI 0.96 to 1.29) (table 3).
Figure. Kaplan-Meier survival curves by income group.
Table 3.
Multivariate analysis of predictors of 1-year mortality after stroke
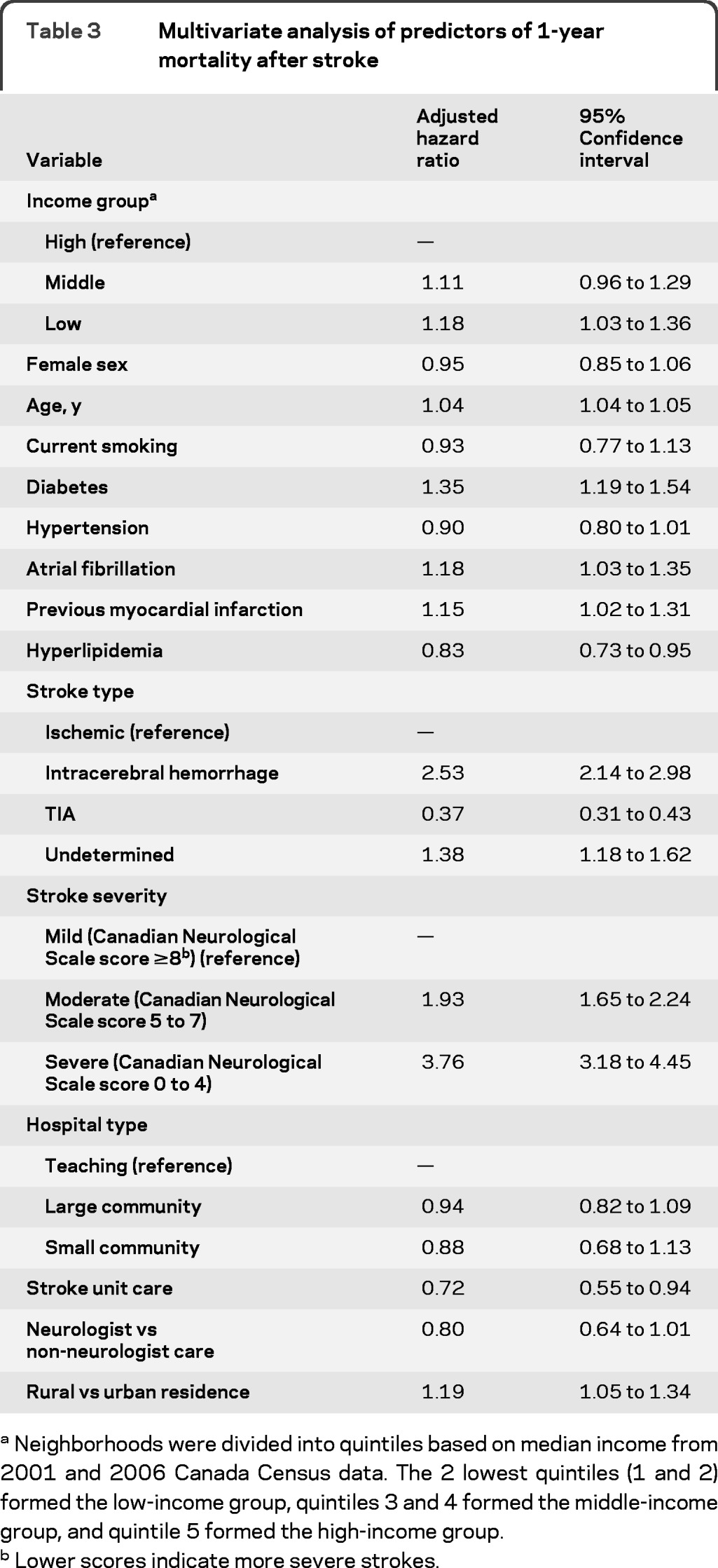
Neighborhoods were divided into quintiles based on median income from 2001 and 2006 Canada Census data. The 2 lowest quintiles (1 and 2) formed the low-income group, quintiles 3 and 4 formed the middle-income group, and quintile 5 formed the high-income group.
Lower scores indicate more severe strokes.
Table 4shows the effect of sequential risk adjustment. Age, sex, and comorbid conditions accounted for only 0.7% (95% CI 0.0% to 27.6%) of the difference in mortality rates after stroke between the low- and high-income groups, while stroke severity accounted for an additional 3.5% (95% CI 0.0% to 36.9%), stroke type for 2.9% (95% CI 0.0% to 42.8%), processes of care and hospital and physician characteristics for 5.6% (95% CI 0.0% to 28.4%), and rural residence for 1.9% (95% CI, 0.0% to 15.0%). Collectively, all factors under consideration explained only 13.9% (95% CI 0.0% to 78.3%) of the disparity in stroke mortality between the low- and high-income groups.
Table 4.
Effect of sequential risk adjustment on income-mortality gradients
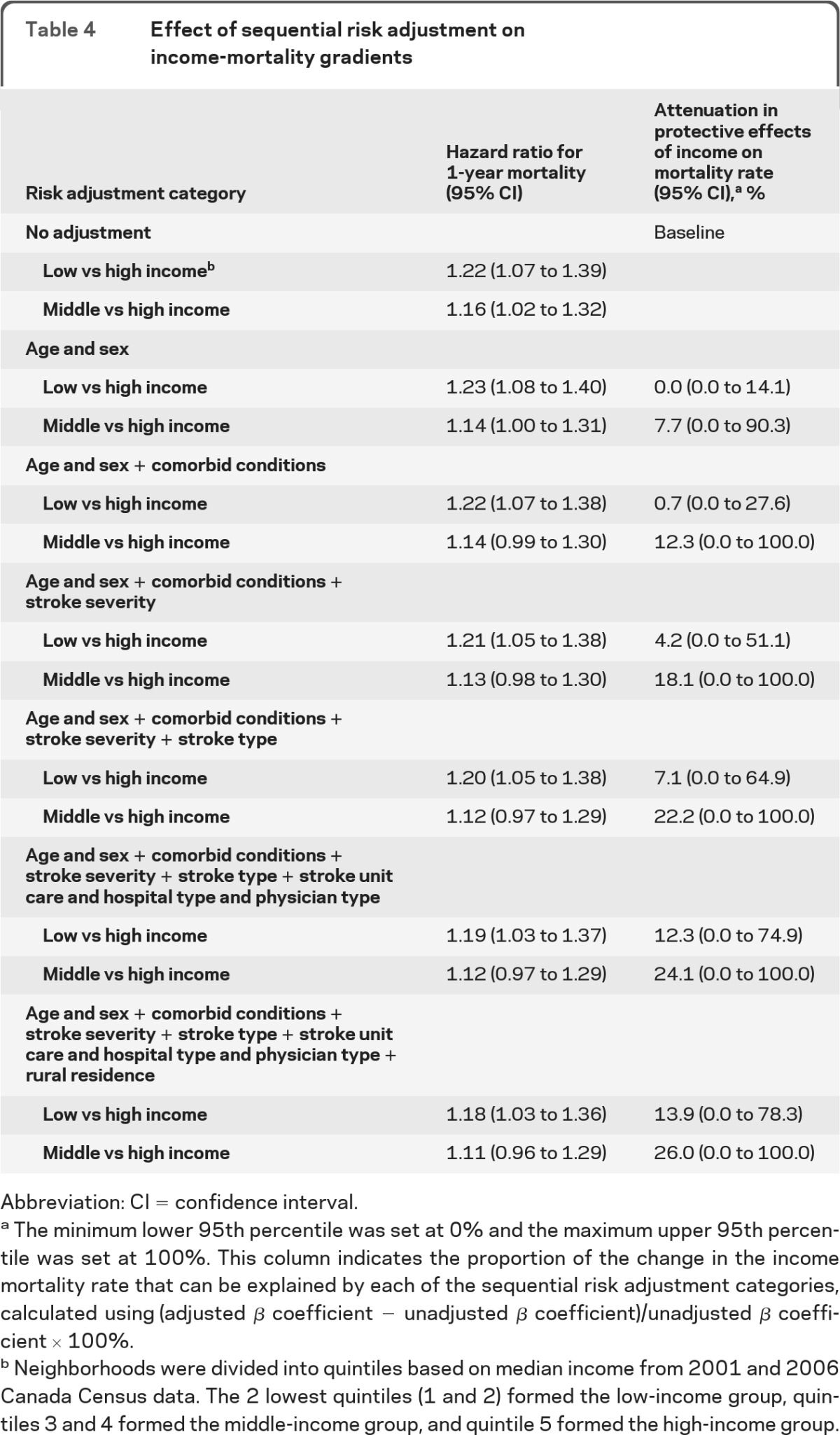
Abbreviation: CI = confidence interval.
The minimum lower 95th percentile was set at 0% and the maximum upper 95th percentile was set at 100%. This column indicates the proportion of the change in the income mortality rate that can be explained by each of the sequential risk adjustment categories, calculated using (adjusted β coefficient − unadjusted β coefficient)/unadjusted β coefficient × 100%.
Neighborhoods were divided into quintiles based on median income from 2001 and 2006 Canada Census data. The 2 lowest quintiles (1 and 2) formed the low-income group, quintiles 3 and 4 formed the middle-income group, and quintile 5 formed the high-income group.
DISCUSSION
We found that individuals from low-income neighborhoods were less likely to present with TIA, had longer times from stroke onset to hospital arrival, and had slightly lower rates of neurologist care compared to those from higher income neighborhoods. However, all other measured aspects of stroke care delivery were similar across income groups. At 1 year after stroke there was a persistent survival advantage for those in the highest compared to the lowest income areas, even after adjustment for age, sex, cardiovascular risk factors, stroke type and severity, in-hospital processes of care, and hospital and physician characteristics. These identifiable risk factors only accounted for a small proportion (13.9%) of the observed disparity in survival between the low- and high-income groups.
An important finding is that mortality at 30 days was similar among socioeconomic groups, and mortality differences were not observed until after the acute care period. This may be due to lower event rates at 30 days with consequent reduced power to observe smaller differences, or due to the fact that stroke severity—rather than processes of care or baseline risk factors—is the principal determinant of early stroke mortality.31 However, this observation also suggests that stroke aftercare may be an important determinant of late mortality after stroke, and is consistent with the structure of our health care system where, in a broad sense, acute care is similar for all.
The finding of lower stroke case fatality rates with higher socioeconomic status has been previously documented, even in Canada and in other countries with universal access to health care.6, 9, 13, 15 Our results suggest that better outcomes among those from high-income areas are not due to marked differences in acute stroke care delivery, and are only partially explained by baseline risk factors and stroke characteristics. This contrasts with findings from a Canadian study of patients with acute myocardial infarction, where age and vascular risk factors appeared to account for the majority of the income-mortality gradient.30 We note that within the CIs, a larger effect of baseline risk factors is possible, and risk factor medication should therefore be a target for interventions designed to improve outcomes in low socioeconomic groups. It is also likely that unmeasured risk factors, including important stroke risk factors such as blood pressure control, physical activity, and waist-to-hip ratios, could account for some of the difference in survival between those from low- and high-income areas, as could differences in adherence to medications and access to follow-up care.32 Of note, in our cohort, higher socioeconomic status was associated with a clustering of risk factors likely to be associated with better outcomes, including low smoking levels and less diabetes, as well as a clustering of sociodemographic factors which could affect access and adherence to care, such as urban residence, higher education, male sex, and fluency in English or French.
Although socioeconomic status has been shown to be an important predictor of the use of certain medical services, such as angiography after myocardial infarction, previous studies have found no consistent association between socioeconomic status and stroke care delivery.2,13,33–36 Given the association between lower socioeconomic status and rural residence, with the potential for limited access to larger hospitals with more stroke-specific resources, one might have anticipated lower rates of specialized interventions such as carotid imaging, neuroimaging, and stroke unit care among patients from low-income neighborhoods. However, Ontario has developed a provincial stroke system aimed at optimizing and coordinating care across the province, and although the system had not been fully implemented during the study period, this might have permitted some patients from rural areas to have been transferred for care and evaluation at regional stroke centers.37 Thus, our results may not be generalizable to jurisdictions without a coordinated stroke care strategy, or to countries without universal access to health care. Of note, the finding of a longer time from stroke onset to hospital arrival in those from lower compared to higher income areas—despite similar rates of ambulance use and similar transport times—suggests that those from lower income neighborhoods may have delays in symptom recognition or in activation of emergency medical services. Knowledge of stroke symptoms and the need for rapid assessment of transient symptoms could also explain the more frequent presentation with TIA in the higher income groups.
Our study has a number of limitations which merit comment. First, we used area-level rather than individual-level measures of socioeconomic status. This may result in nondifferential misclassification of socioeconomic status and lead to underestimates of social gradients in mortality. However, neighborhood-level income measures have the advantage of capturing aspects of neighborhoods, such as the availability of parks, schools, and hospitals, that may affect health, and have been found to provide results that are complementary to those found using individual level data.38,39 Second, we used income as our primary measure of socioeconomic status rather than wealth, occupation, social class, or other composite measures. Although most measures of socioeconomic status tend to be highly correlated and to predict mortality in a similar direction, they may not be consistent in direction and magnitude for all outcomes.14,17,40 In addition, although the socioeconomic status of both an individual and an area may fluctuate over time, the cross-sectional nature of our study meant that we were only able to capture neighborhood income at a single time point. Finally, our data were collected through hospital chart audits rather than prospective data collection or patient or provider interviews. Thus, we were unable to capture information on stroke symptom awareness and potential barriers to stroke care delivery, and we were unable to evaluate risk factor modification and treatment adherence after hospital discharge. In addition, we do not have information on potentially important explanatory variables such as obesity, social isolation, and mental illness. Despite these limitations, our database contains high-quality clinical data on a population-based patient sample, and is strengthened by its linkage to administrative databases to provide long-term follow-up outcomes.
In Ontario's universal health care system, we found higher survival rates after stroke for individuals from the richest compared to the least wealthy neighborhoods. This was not fully explained by differences in stroke type, stroke severity, or processes of stroke care delivery, and may be related in part to a lower burden of unmeasured baseline risk factors for poor health. The superior health outcomes seen for the wealthiest members of society may provide a benchmark for what could be achieved for all through targeted interventions to reduce socioeconomic disparities in health.
Supplementary Material
ACKNOWLEDGMENT
The authors thank the hospitals, investigators, and research coordinators who participated in the Ontario Stroke Audit of the Registry of the Canadian Stroke Network, as well as the staff at the Institute for Clinical Evaluative Sciences and the Canadian Stroke Network who assisted in the coordination of the Registry.
GLOSSARY
- CI
confidence interval
- CIHI
Canadian Institute for Health Information
- DAD
discharge abstract database
- HR
hazard ratio
- ICD
International Classification of Diseases
- ICES
Institute for Clinical Evaluative Sciences
- NACRS
National Ambulatory Care Reporting System
- RCSN
Registry of the Canadian Stroke Network
Footnotes
Editorial, page 1190.
AUTHOR CONTRIBUTIONS
Drs. Kapral, Chan, Alter, Bronskill, Hill, Manuel, Tu, and Anderson contributed to the study concept and design, interpretation of the data, and drafting and revisions to the manuscript. Dr. Fang contributed to the study design, performed data analyses, and revised the manuscript.
Study funding
This work was funded by an operating grant from the Canadian Stroke Network. The Registry of the Canadian Stroke Network is funded by the Canadian Stroke Network and the Ontario Ministry of Health and Long-Term Care. The Institute for Clinical Evaluative Sciences is supported by an operating grant from the Ontario Ministry of Health and Long-Term Care. Dr. Kapral is supported by a Career Investigator Award from the Heart and Stroke Foundation of Canada. Dr. Bronskill is supported by a New Investigator Award in the Area of Aging from CIHR. Dr. Hill is supported by a scholarship from the CIHR and Heart & Stroke Foundation of Alberta/NWT/Nunavut. Dr. Tu holds a Canada Research Chair in Health Services Research and a Career Investigator Award from the Heart and Stroke Foundation of Ontario. Dr. Manuel holds a Chair in Applied Public Health from CIHR. Dr. Anderson holds the Chair in Health Management Strategies in the Faculty of Medicine, University of Toronto. The results and conclusions are those of the authors, and should not be attributed to any of the sponsoring or funding agencies. The funding agencies had no role in the design or conduct of the study or the collection, management, analysis, and interpretation of the data. The manuscript was reviewed and approved by the publications committee of the Registry of the Canadian Stroke Network.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1. Kunst AE, Groenhof F, Mackenbach JP, the EU Working Group on Socioeconomic Inequalities in Health Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies. BMJ 1998;316:1636–1641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med 1999;341:1359–1367 [DOI] [PubMed] [Google Scholar]
- 3. Marmot MG. Status syndrome: a challenge to medicine. JAMA 2006;295:1304–1307 [DOI] [PubMed] [Google Scholar]
- 4. Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z. Income inequality, mortality and self rated health: meta-analysis of multilevel studies. BMJ 2009;339:b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stjarne MK, Fritzell J, De Leon AP, Hallqvist J, for the SHEEP Study Group Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology 2006;17:14–23 [DOI] [PubMed] [Google Scholar]
- 6. Cox AM, McKevitt C, Rudd AG, Wolfe CD. Socioeconomic status and stroke. Lancet Neurol 2006;5:181–188 [DOI] [PubMed] [Google Scholar]
- 7. Arrich J, Lalouschek W, Mullner M. Influence of socioeconomic status on mortality after stroke: retrospective cohort study. Stroke 2005;36:310–314 [DOI] [PubMed] [Google Scholar]
- 8. Jakovljevic D, Sarti C, Sivenius J, et al. Socioeconomic status and ischemic stroke: the FINMONICA stroke register. Stroke 2001;32:1492–1498 [DOI] [PubMed] [Google Scholar]
- 9. Kapral MK, Wang H, Mamdani M, Tu JV. Effect of socioeconomic status on treatment and mortality after stroke. Stroke 2002;33:268–273 [DOI] [PubMed] [Google Scholar]
- 10. Kleindorfer DA, Lindsell C, Broderick J, et al. Impact of socioeconomic status on stroke incidence: a population-based study. Ann Neurol 2006;60:480–484 [DOI] [PubMed] [Google Scholar]
- 11. Weir N, Gunkel A, McDowall M, Dennis MS. Study of the relationship between social deprivation and outcome after stroke. Stroke 2005;36:815–819 [DOI] [PubMed] [Google Scholar]
- 12. Avendano M, Kawachi I, van Lenthe F, et al. Socioeconomic status and stroke incidence in the US elderly: the role of risk factors in the EPESE study. Stroke 2006;37:1368–1373 [DOI] [PubMed] [Google Scholar]
- 13. Langagergaard V, Palnum KH, Mehnert F, et al. Socioeconomic differences in quality of care and clinical outcome after stroke: a nationwide population-based study. Stroke 2011;42:2896–2902 [DOI] [PubMed] [Google Scholar]
- 14. Grimaud O, Bejot Y, Heritage Z, et al. Incidence of stroke and socioeconomic neighborhood characteristics: an ecological analysis of Dijon Stroke Registry. Stroke 2011;42:1201–1206 [DOI] [PubMed] [Google Scholar]
- 15. Li C, Hedblad B, Rosvall M, Buchwald F, Ali Khan F, Engstrom G. Stroke incidence, recurrence, and case-fatality in relation to socioeconomic position: a population-based study of middle-aged Swedish men and women. Stroke 2008;39:2191–2196 [DOI] [PubMed] [Google Scholar]
- 16. Cesaroni G, Agabiti N, Forastiere F, Perucci CA. Socioeconomic differences in stroke incidence and prognosis under a universal health care system. Stroke 2009;40:2812–2819 [DOI] [PubMed] [Google Scholar]
- 17. Avendano M, Glymour MM. Stroke disparities in older Americans: is wealth a more powerful indicator of risk than income and education? Stroke 2008;39:1533–1540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Avendano M, Kunst AE, van Length F, et al. Trends in socioeconomic disparities in stroke mortality in six European countries between 1981–1985 and 1991–1995. Am J Epidemiol 2005;161:52–61 [DOI] [PubMed] [Google Scholar]
- 19. Thrift AG, Dewey HM, Sturm JW, et al. Greater incidence of both fatal and nonfatal strokes in disadvantaged areas: the Northeast Melbourne Stroke Incidence Study. Stroke 2006;37:877–882 [DOI] [PubMed] [Google Scholar]
- 20. van Rossum CT, van de Mheen H, Breteler MM, Brobbee DE, Mackenbach JP. Socioeconomic differences in stroke among Dutch elderly women: the Rotterdam Study. Stroke 1999;30:357–362 [DOI] [PubMed] [Google Scholar]
- 21. Hart CL, Hole DJ, Smith GD. Influence of socioeconomic circumstances in early and later life on stroke risk among men in a Scottish cohort study. Stroke 2000;31:3092–2097 [DOI] [PubMed] [Google Scholar]
- 22. Saposnik G, Jeerakathil T, Selchen D, Baibergenova A, Hachinski V, Kapral MK. Socioeconomic status, hospital volume, and stroke fatality in Canada. Stroke 2008;39:3360–3366 [DOI] [PubMed] [Google Scholar]
- 23. Anderson GA, Bronskill SE, Mustard CA, Culyer A, Alter DA, Manuel DG. Both clinical epidemiology and population health perspectives can define the role of health care in reducing health disparities. J Clin Epidemiol 2005;58:757–762 [DOI] [PubMed] [Google Scholar]
- 24. Kurth T, Berger K. The socioeconomic stroke puzzle. Stroke 2007;38:4–5 [DOI] [PubMed] [Google Scholar]
- 25. Pilote L, Tu JV, Humphries K, Behouli H, Belisle P, Austin PC, Joseph L. Socioeconomic status, access to health care, and outcomes after acute myocardial infarction in Canada's universal health care system. Med Care 2007;45:638–646 [DOI] [PubMed] [Google Scholar]
- 26. Kapral MK, Hall RE, Silver FL, et al. The Registry of the Canadian Stroke Network Report on the 2004/05 Ontario Stroke Audit, Toronto, Institute for Clinical Evaluative Sciences, 2009. Available at: http://www.ices.on.ca/file/RCSN_2004-05%20Ontario%20Stroke%20Audit%20Report_Final_April%2006.pdf Accessed July 28, 2012
- 27. Southern DA, Ghali WA, Faris PD, et al. Misclassification of income quintiles derived from area-based measures. Can J Public Health 2002;93:465–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cote R, Battista RN, Wolfson C, Boucher J, Adams J, Hachinski VC. The Canadian Neurological Scale: validation and reliability assessment. Neurology 1989;39:638–643 [DOI] [PubMed] [Google Scholar]
- 29. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 30. Alter DA, Chong A, Austin AC, et al. Socioeconomic status and mortality after acute myocardial infarction. Ann Intern Med 2006;144:82–93 [DOI] [PubMed] [Google Scholar]
- 31. Saposnik G, Hill MD, O'Donnell M, Hachinski V, Fang J, Kapral MK. Variables associated with 7-day, 30-day and 1-year mortality after ischemic stroke. Stroke 2008;39:2318–2324 [DOI] [PubMed] [Google Scholar]
- 32. O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010;376:112–123 [DOI] [PubMed] [Google Scholar]
- 33. McKevitt C, Coshall C, Tilling K, Wolfe CDA. Are there inequalities in the provision of stroke care? Analysis of an inner-city stroke register. Stroke 2005;36:315–320 [DOI] [PubMed] [Google Scholar]
- 34. van den Bos GAM, Smits JPJM, Westert GP, van Straten A. Socioeconomic variations in the course of stroke: unequal health outcomes, equal care? J Epidemiol Community Health 2002;56:943–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Arrich J, Mullner M, Lalouschek W, Greisenegger S, Crevenna R, Herkner H. Influence of socioeconomic status and gender on stroke treatment and diagnostics. Stroke 2008;39:2066–2072 [DOI] [PubMed] [Google Scholar]
- 36. Kleindorfer DA, Lindsell C, Broderick J, et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: do poorer patients have longer delays from 911 call to the emergency department? Stroke 2006;37:1508–1513 [DOI] [PubMed] [Google Scholar]
- 37. Heart and Stroke Foundation of Ontario, Ontario Ministry of Health and Long-Term Care. Towards an integrated stroke strategy for Ontario: report of the Joint Stroke Strategy Working Group. 2000. Available at: http://health.gov.on.ca/en/common/ministry/publications/reports/stroke/strokereport.pdf Accessed July 28, 2012
- 38. Huston SL, Evenson KR, Bors B, Gizlice Z. Neighborhood environment, access to places for activity, and leisure-time physical activity in a diverse North Carolina population. Am J Health Promotion 2003;18:58–69 [DOI] [PubMed] [Google Scholar]
- 39. Southern DA, McLaren L, Hawe P, Knudtson ML, Ghali WA, APPROACH Investigators Individual-level and neighbourhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care 2005;43:1116–1122 [DOI] [PubMed] [Google Scholar]
- 40. Alter DA, Austin PC, Tu JV, Canadian Cardiovascular Outcomes Research Team Community factors, hospital characteristics and inter-regional outcome variations following acute myocardial infarction in Canada. Can J Cardiol 2005;21:247–255 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.