Abstract
Proximal hamstring avulsions from the ischium are becoming more frequently recognized, secondary to their disability when treated nonoperatively. The acute repair of these injuries is becoming prevalent given the improved outcomes reported in the literature. Anatomic studies have recently been conducted on the proximal hamstring origin; however, there are few reports on surgical techniques for repair in the setting of injury. The present article describes the technique for proximal hamstring avulsion repair, as performed by the senior author. More than 30 cases have been performed based on this technique, with excellent results.
Keywords: proximal hamstring injury, avulsion, repair
Acute hamstring strains are one of the most common injuries in athletes, and the majority are successfully treated with nonoperative measures.1,2,21 However, proximal hamstring avulsions from the ischial tuberosity are a distinct type of injury. They are increasingly recognized as needing surgical intervention, leading to a delay in return to sport and to long-lasting functional impairments when not treated appropriately.2-8,10-14,19,20,22 Early case reports and anatomic studies show positive results from surgical repair of proximal hamstring injuries. For surgical repair, early diagnosis is critical to facilitating a successful outcome and preventing long-term functional impairment.
Ishikawa et al10 made the first such report of surgical repair in 1988—specifically, 2 cases of proximal hamstring tendon avulsions. Reported rates of return to preinjury levels have ranged from 88% to 100%, but each study included a small number of case reports.4,7,10,11,14-16 A repaired hamstring tendon may be almost as functional as the uninjured hamstring (88% to 91% on Cybex testing).11,16 Surgical repair of proximal hamstring injuries may lead to improved functional outcomes.2-8,10-14,19,20,22
Proximal hamstring tendon anatomy, injury classification, and repair techniques have been detailed in previous publications.6,9,17,18 Anatomic studies have shown that the proximal hamstrings consist of a conjoint tendon (biceps femoris and semitendinosus) that inserts posterior and inferior on the ischial tuberosity to the more proximal-anterior semimembranosus tendon. In considering the need for a surgical repair of the proximal hamstring tendons, injury classification is important, given that some injury patterns can be successfully treated nonoperatively.
The surgical procedure can be divided into 3 steps: patient positioning and surgical exposure, tendon repair, and postoperative protocol.
Operative Technique
Patient Positioning and Surgical Exposure
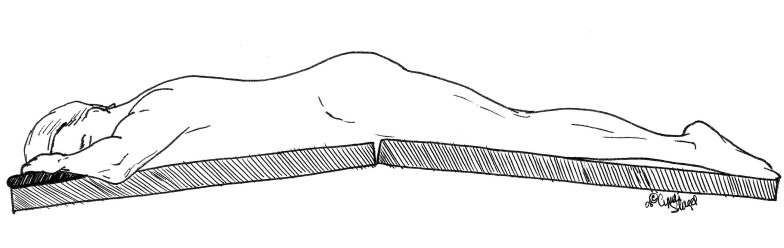
The patient is placed in the prone position on the operating room table, with all bony prominences padded and with the table flexed 20° (Figure 1).
Figure 1.
Hamstring repair reclining: table flexed 20°.
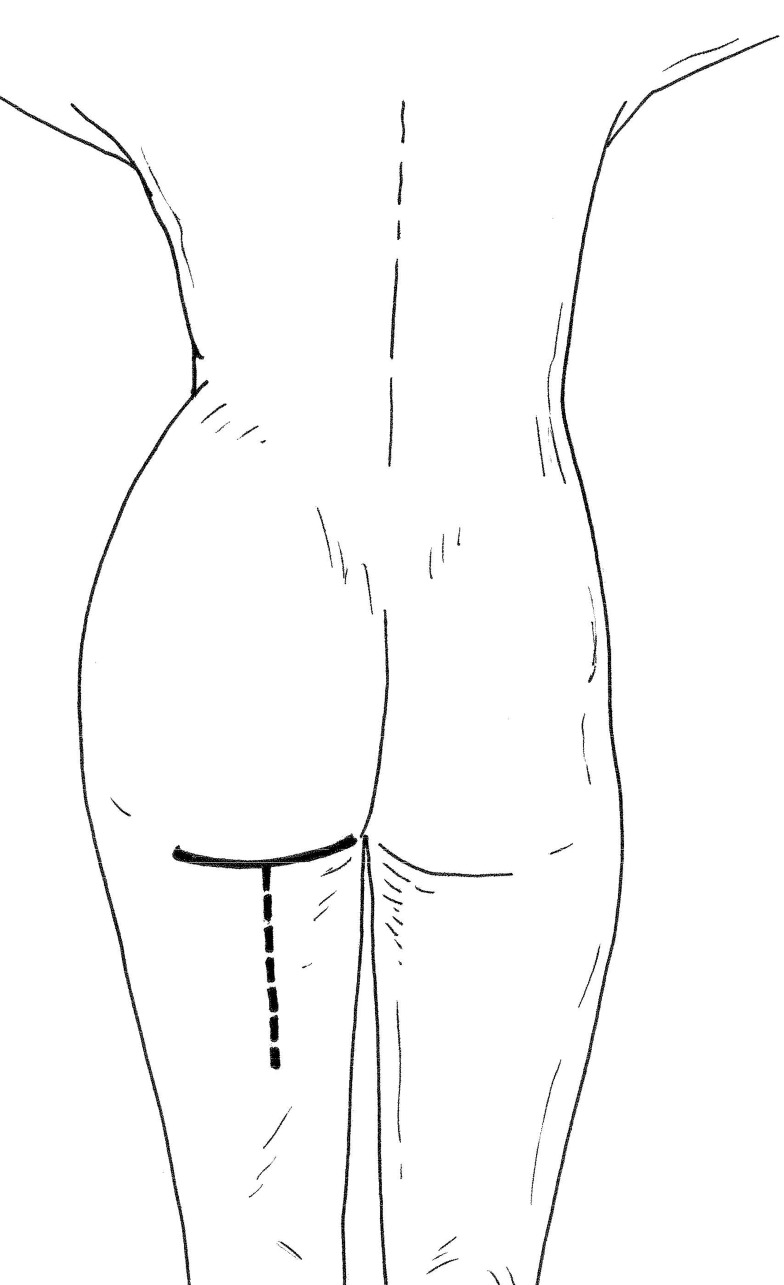
A transverse incision is made in the gluteal crease of the affected leg, directly inferior to the ischial tuberosity (Figure 2). A transverse incision is preferred to a traditionally described longitudinal incision, because of improved cosmesis and accessibility to the avulsed tendons. If inferior dissection is warranted to retrieve retracted tendons, this incision can be extended by making a T limb down the back of the thigh.
Figure 2.
Gluteal incision: inferior to the ischial tuberosity.
The incision is dissected to the gluteal fascia, which is incised transversely while taking care to avoid injury to the posterior femoral cutaneous nerve. This provides access to the gluteus maximus muscle.
When the muscle fibers of the gluteus maximus are exposed, the dissection is carried out longitudinally by splitting the muscle fibers in line with their length. This is accomplished by locating a raphe that is in line, and just inferior to, the ischial tuberosity at palpation. This will expose the hamstring fascia in which the hamstring tendons are located.
A longitudinal incision is made in the hamstring fascia. Typically, hematoma and/or serous fluid in an acute setting will be expressed. In more chronic settings, a layer of fibrous tissue (scar), or pseudosheath, can lie over the ruptured coalescence of the hamstring tendons and so give the appearance of intact tendons. This layer must be incised to expose the avulsed tendons.
Care should be taken to protect the sciatic nerve, which in chronic cases may become adherent and scarred to the area of injury. Staying within the hamstring fascia, or pseudosheath, is an important component in the protection of the sciatic nerve (Figure 3).
Figure 3.
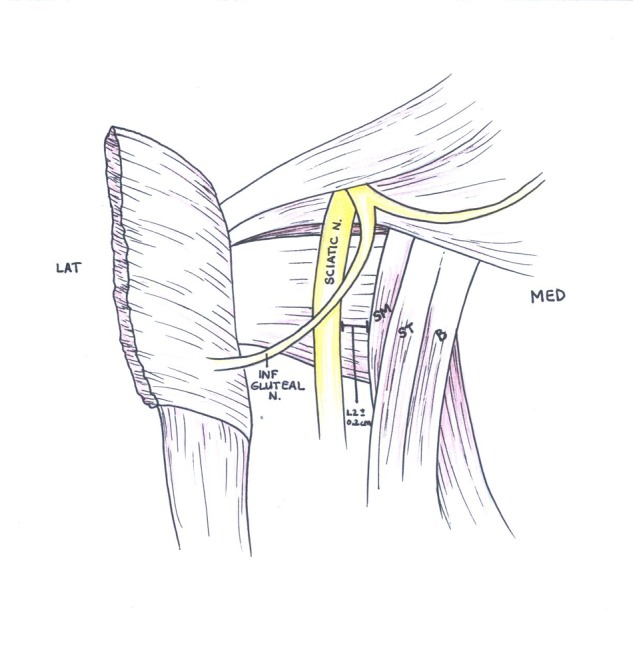
Normal proximal hamstring anatomy. The sciatic nerve is 1.2 ± 0.2 cm lateral to the tendons; the inferior gluteal nerve is more proximal but can be in danger with proximal and lateral deviation during exposure.
Tendon Repair
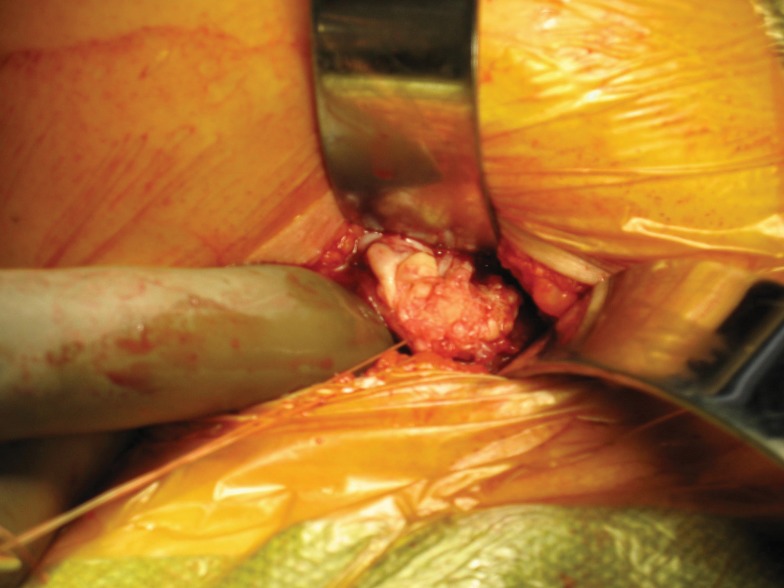
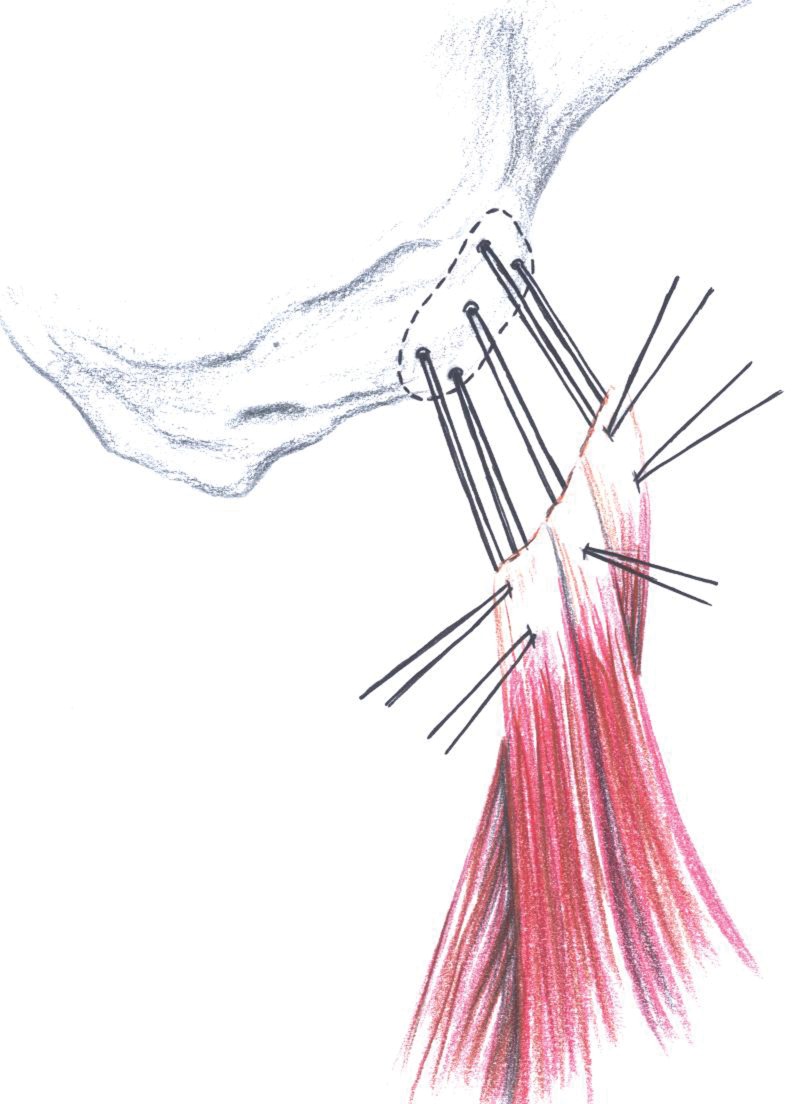
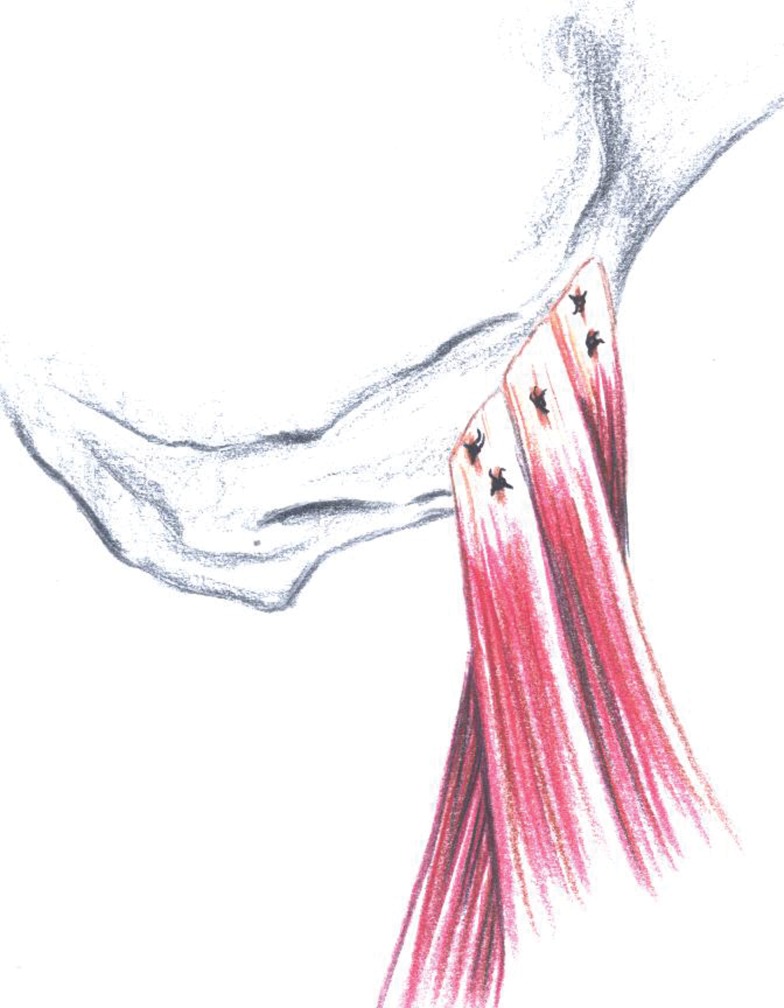
The sciatic nerve should be protected by gentle lateral blunt retraction. After the tendons have been exposed and the tear pattern identified, the fibrotic tissue on the ends of the tendons should be debrided to normal tissue (Figures 4 and 5). Care should be taken not to remove an excessive amount of tissue, because doing so may shorten the tendon.
Figure 4.
Fibrotic tissue on the ends of the tendons debrided to normal tissue.
Figure 5.
Open repair: avoid removing excessive amount of tendon tissue to avoid shortening the tendon.
The tendons are mobilized and tagged with heavy suture for traction. The ischial tuberosity is identified, as is the hamstring insertion on its inferolateral aspect. A periosteal elevator, rongeur, and curette are used to expose the anatomic origin of the tendons, which will denude the bone and so provide for direct tendon healing to bone. Motorized burrs should not be used because they may cause iatrogenic injuries to the sciatic nerve. The semimembranosus tendon is located anterior and lateral to the conjoint tendon (composed of the long head of the biceps femoris and the semitendinosus tendons).17
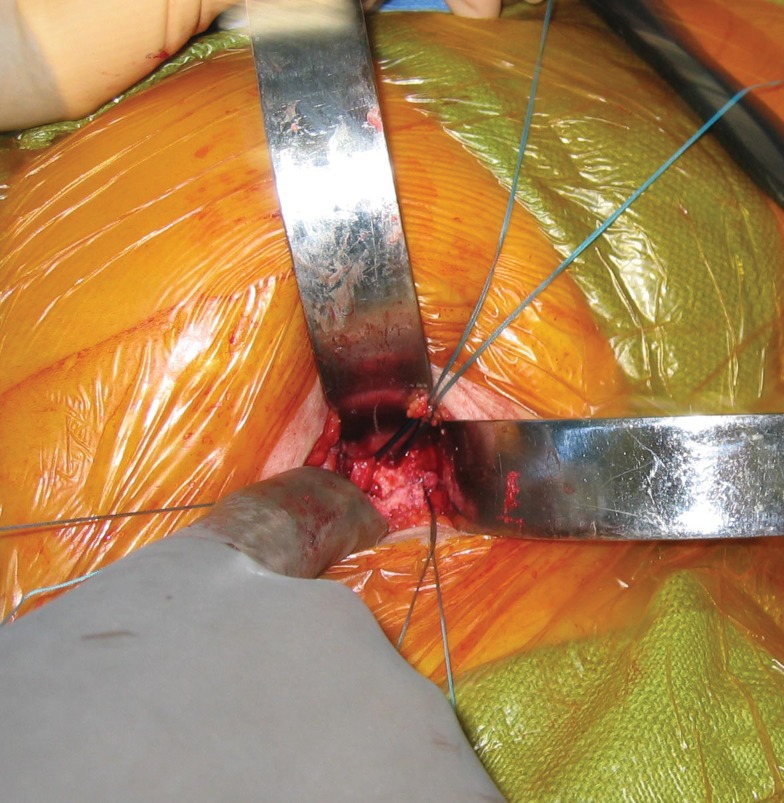
Five suture anchors are placed into the ischial tuberosity, in an X-shaped configuration, by drilling perpendicular to the facet of the hamstring origin. Care is taken not to plunge through both cortices of the tuberosity. The authors prefer bioabsorbable suture anchors with abrasion resistant suture (2.8 mm × 18.0 cm, BioRoc EZ, Dupuy Mitek, Raynham, Massachusetts). The sutures are then passed through the tendon in a similar X-like fashion, using horizontal mattress sutures (Figure 6). The Bunnell, modified Kessler, and modified Mason-Allen stitches are not used because they bunch up the tendon at the bony interface and thus shorten the tendon.
Figure 6.
Hamstring repair: sutures passed through tendon in X-like formation.
At this point, the knee is flexed 30° to 60° to take tension off the proximal hamstring before finalizing the repair. The sutures are then tied, from the inferior position to the superior (Figure 7).
Figure 7.
Hamstring repair: sutures tied, inferior to superior.
After repair, the gluteus fascia is closed. A postoperative hip-knee orthosis is used to limit hip flexion to 15° to reduce stress on the tendon repair. Knee motion is not restricted in the orthosis.
Postoperative Protocol
The first phase of rehabilitation lasts 6 weeks. The patient is kept at touch down weight bearing for 2 weeks and is advanced to 25% weight bearing over the following 3 weeks. This allows slight hip and knee flexion but limits the stress at the repair site. Passive range of motion of the knee and hip begins at 2 weeks, and active hip range of motion begins at 4 weeks. Hip range of motion is advanced 10° each week after surgery in the hip-knee orthosis until the end of the first phase.
The second phase starts with full weight bearing at 6 weeks postoperatively. Gait training is initiated. Passive and active range of motion is progressed. Isotonic exercises and aquatherapy are begun within a limited range, avoiding terminal range of hip flexion (more than 110°). At 8 weeks, isotonic strengthening is begun and dynamic training is advanced. At 10 weeks, an isometric strength evaluation is performed at 60° of knee flexion.
The final phase of rehabilitation begins at 10 weeks postoperatively. Dry-land jogging is initiated with continued strengthening. A full isokinetic evaluation at 60°, 120°, and 180° is performed and then compared to that of the uninjured leg. Sport-specific activities are emphasized and return to play permitted when isokinetic testing on the repaired leg is 80% of the unaffected side. This typically occurs between 6 and 9 months.
Footnotes
No potential conflict of interest declared.
References
- 1. Agre JC. Hamstring injuries: proposed aetiological factors, prevention, and treatment. Sports Med. 1985;2:21-33 [DOI] [PubMed] [Google Scholar]
- 2. Blasier RB, Morawa LG. Complete rupture of the hamstring origin from water skiing injury. Am J Sports Med. 1990;18:435-437 [DOI] [PubMed] [Google Scholar]
- 3. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13:411-418 [DOI] [PubMed] [Google Scholar]
- 4. Chakravarthy J, Ramisetty N, Pimalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39:569-572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237-248 [DOI] [PubMed] [Google Scholar]
- 6. Cohen S, Bradley JP. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350-355 [DOI] [PubMed] [Google Scholar]
- 7. Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26:785-788 [DOI] [PubMed] [Google Scholar]
- 8. Garrett WE, Jr, Califf JC, Bassett FH. Histological correlates of hamstring injuries. Am J Sports Med. 1989;2:98-103 [DOI] [PubMed] [Google Scholar]
- 9. Garrett WE, Jr, Ross RF, Nikolaou P, Vogler JB. Computed tomography of hamstring muscle strains. Med Sci Sports Exerc. 1984;5:506-514 [PubMed] [Google Scholar]
- 10. Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity. A report of two cases. Clin Orthop Relat Res. 1988;232:153-155 [PubMed] [Google Scholar]
- 11. Johnson AE, Granville RR, DeBerardino TM. Avulsion of the common hamstring tendon origin in an active duty airman. Mil Med. 2003;168:40-42 [PubMed] [Google Scholar]
- 12. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742-747 [DOI] [PubMed] [Google Scholar]
- 13. Kujala UM, Orava S, Jarvinen M. Hamstrings injuries: current trends in treatments and prevention. Sports Med. 1997;23:397-404 [DOI] [PubMed] [Google Scholar]
- 14. Kurosawa H, Nakasita K, Nakasita H, Sasaki S, Takeda S. Complete avulsion of the hamstring tendons from the ischial tuberosity. A report of two cases sustained in judo. Br J Sports Med. 1996;30:72-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40:688-691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med. 1985;13:349-358 [DOI] [PubMed] [Google Scholar]
- 17. Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study. J Bone Joint Surg Am. 2007;89:44-48 [DOI] [PubMed] [Google Scholar]
- 18. Miller SL, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. Surgical technique. J Bone Joint Surg Am. 2008;90:108-116 [DOI] [PubMed] [Google Scholar]
- 19. Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23:702-705 [DOI] [PubMed] [Google Scholar]
- 20. Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130-136 [DOI] [PubMed] [Google Scholar]
- 21. Speer KP, Lohnes J, Garrett WE., Jr Radiographic imaging of muscle strain injury. Am J Sports Med. 1993;21:89-96 [DOI] [PubMed] [Google Scholar]
- 22. Thomsen NO, Jensen TT. Late repair of rupture of the hamstring tendons from the ischial tuberosity—a case report. Acta Orthop Scand. 1999;70:89-91 [DOI] [PubMed] [Google Scholar]