Abstract
Context
Low back pain in young athletes is a common complaint and should be taken seriously. It frequently results from a structural injury that requires a high degree of suspicion to diagnose and treat appropriately.
Evidence Acquisition
A Medline search was conducted from 1996 to May 2008 using the search terms “low back pain in children” and “low back pain in athletes.” Known texts on injuries in young athletes were also reviewed. References in retrieved articles were additionally searched for relevant articles. Sources were included if they contained information regarding diagnosis and treatment of causes of low back pain in children.
Results
Low back pain is associated with sports involving repetitive extension, flexion, and rotation, such as gymnastics, dance, and soccer. Both acute and overuse injuries occur, although overuse injuries are more common. Young athletes who present with low back pain have a high incidence of structural injuries such as spondylolysis and other injuries to the posterior elements of the spine. Disc-related pathology is much less common. Simple muscle strains are much less likely in this population and should be a diagnosis of exclusion only.
Conclusion
Young athletes who present with low back pain are more likely to have structural injuries and therefore should be investigated fully. Muscle strain should be a diagnosis of exclusion. Treatment should address flexibility and muscle imbalances. Injuries can be prevented by recognizing and addressing risk factors. Return to sport should be a gradual process once the pain has resolved and the athlete has regained full strength.
Keywords: low back pain, adolescents, pediatric athletes
Low back pain is estimated to occur in 10% to 15% of young athletes,2 but the prevalence may be higher in certain sports.2,4,8,10,18,24 Studies show that back pain occurs frequently in college football players (27%), artistic gymnasts (50%), and rhythmic gymnasts (86%).8,10,18
Patterns of back pain in young athletes are significantly different from those in adults.11,16,23,25 Pars interarticularis injuries are more common, occurring in up to 47% of young athletes.16 Disc-related problems are relatively uncommon in children; only 11% of children have disc-related pathology compared with 48% of adults.16 Idiopathic pain is also less common in young athletes. Physicians who attribute low back pain in young athletes to simple back strains, without investigations, run the risk of delaying the diagnosis and appropriate treatment of more serious injuries, such as spondylolysis or spondylolisthesis.11,25
Injuries to the low back occur from either an acute traumatic event or from repetitive microtrauma (overuse injury), with overuse injuries being more common. Contact sports such as football or rugby tend to produce acute injuries from high-energy impacts, whereas sports involving repetitive flexion, extension, and torsion, such as gymnastics, figure skating, and dance, result in overuse injuries (Figure 1). It is very important to consider other more sinister causes of back pain, such as infection, tumors, or inflammatory conditions.
Figure 1.

A figure skater hyperextending her spine duringa spin.
Risk Factors
During periods of rapid growth, soft tissues such as muscles and ligaments are unable to keep pace with the rate of bone growth, resulting in muscle imbalances and a decrease in flexibility.2,19 This can place young athletes at greater risk for injury.
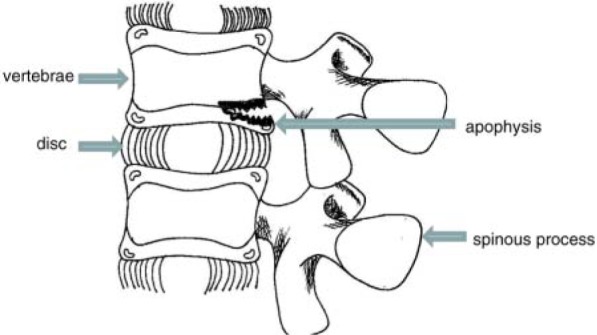
Growth cartilage and secondary ossification centers, present only in the skeletally immature, are particularly vulnerable to injury.2 During growth, these areas are the weakest link of force transfer and are susceptible to compression, distraction, and torsion injury.2,24 The anterior column of the lumbar spine is comprised of the vertebral bodies separated by the intervertebral discs (Figure 2). The vertebral bodies have epiphyseal growth plates at either end, with overlying cartilaginous end plates and ring apophyses. The ring apophyses are attached to the outer anulus fibrosus. The intervertebral disc may herniate through the ring apophysis, a secondary ossification center, with repetitive flexion. Injury to the ring apophysis can result in avulsion fractures.
Figure 2.
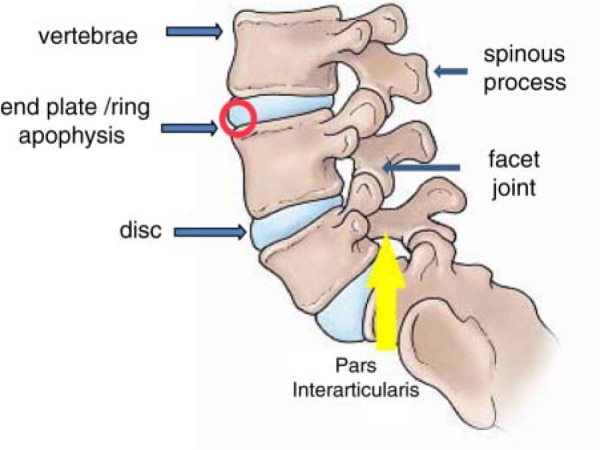
Anatomy of the lumbar spine.
The posterior column of the lumbar spine consists of the neural arch, including the facet joints, spinous process, and the pars interarticularis (Figure 2). Ossification of the posterior column of the spine progresses from anterior to posterior and may be congenitally incomplete in the area of the superior portion of the pars interarticularis of the lower lumbar vertebrae, particularly L5, predisposing to spondylolytic stress fractures.2,25 The presence of spina bifida occulta at the lumbosacral junction appears to be an additional risk factor for spondylolysis. In addition, the growth cartilage of the facet joint and spinous process apophysis of the posterior arch is subjected to traction from the dorsolumbar fascia and lordotic impingement.2
Rate of growth and maturation varies from child to child, resulting in significant differences in size, strength, and skeletal maturity among children of the same chronological age. Children between 6 and 10 years of age, on average, grow about 5 to 8 cm per year and gain about 2 to 3 kg per year.13 During adolescence, growth rates increase, with increases in height occurring first, followed by weight. On average, girls enter their adolescent growth spurt and reach their maximal growth velocity about 2 years before boys (Table 1). Weight gain occurs during the maximal growth in height. Girls gain about 7 kg in fat-free mass, whereas boys gain about twice this amount.13
Table 1.
Growth characteristics during the adolescent growth spurt for girls and boys.13
| Growth Characteristics | Girls | Boys |
|---|---|---|
| Age at start | 9-10 y | 11-12 y |
| Age at maximum growth | 12 y | 14 y |
| Age at which growth slows | >12 y | >14 y |
| Age until growth continues | 16-18 y | 18-20 y |
| Age at maximum height growth | 11-13 y | 13-15 y |
Because the timing and tempo of growth varies considerably among children, smaller, skeletally less mature players may potentially be at higher injury risk from contact with bigger players, particularly in contact sports such as hockey and football.19,25
Training volume and intensity can also cause injury. Injuries occur more often when young athletes participate in a sport for longer periods of time such as during tournaments and specialized sports camps.25 It is difficult to determine the appropriate amount of training for young athletes because not all athletes will tolerate the same volume of training. Overuse injuries present more often in athletes experiencing rapid growth,2,25 suggesting that the volume and intensity of training that an athlete’s body can tolerate may vary as they grow and mature.25 Furthermore, poor technique is a risk factor for injury at any age.
Additional risk factors for low back injury include abdominal muscle weakness; hip flexor, hamstring, and thoracolumbar fascia tightness; increased femoral anteversion; genu recurvatum; and increased thoracic kyphosis.2,25 These factors increase lumbar lordosis and place additional stress on the posterior elements of the spine.
History
A thorough history and physical examination is essential when evaluating a young athlete with low back pain. Onset and duration of symptoms should differentiate between acute trauma and overuse injuries. Location, quality, and severity of pain should be determined, as well as eliciting any associated neurologic symptoms and aggravating factors.
The type of sport or activity and position played must be elicited, as well as the volume of training and level of competition.11,25 It is also important to ascertain if there have been recent increases in volume or intensity of training. Diet history, previous history of injuries, and menstrual history in female athletes should also be elicited.25
“Red flag” symptoms such as fever, malaise, weight loss, neurologic abnormalities, night pain, and morning stiffness may suggest more sinister causes of low back pain, such as infection, tumor, or arthritis.2,6,20,25 A past history or family history of human leukocyte antigen (HLA)-B27–associated conditions, such as psoriatic arthritis, ankylosing spondylitis, or inflammatory bowel disease, may help point to other causes of low back pain.
Physical Examination
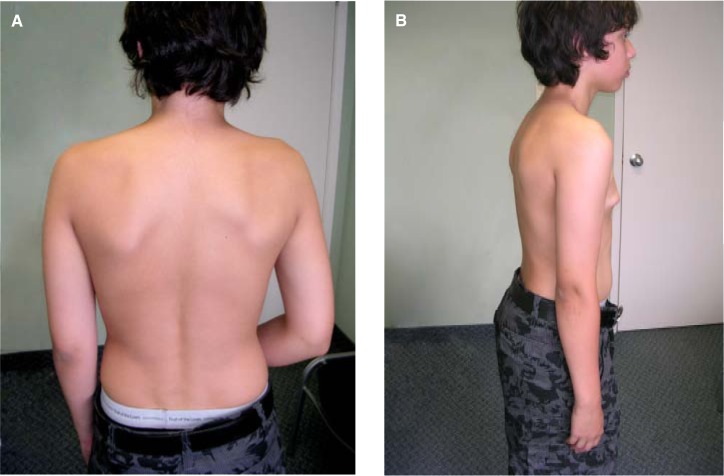
Physical examination of a young athlete with low back pain should include observation of the athlete’s gait and posture, noting any ataxia, antalgic gait, limp, or Trendelenburg gait. The back should be observed by having the patient wear a gown that opens in the back. From behind, the shoulders and pelvis should be level, and the bony and soft tissue structures on both sides of midline should be symmetrical (Figure 3A). Note should be made of any abnormalities, such as hemangiomas, café-au-lait spots, hairy patches, or skin dimples that may indicate spinal pathology.7,19 Spinal abnormalities such as scoliosis, kyphosis, or excess lordosis should also be noted. From the side, there should be a gentle lumbar lordosis (Figure 3B). To assess for scoliosis, a forward-bending test should be performed to look for a rib hump (Figure 4).
Figure 3.
Observation of the back (A). From the side, there should be a gentle lumbar lordosis (B).
Figure 4.

Adams forward-bending test. The patient leans forward with the arms hanging down. The examiner stands behind the patient, observing for spinal abnormalities.
Range of motion of the spine should be assessed in flexion, extension, rotation, and lateral bending. Athletes should be able to flex forward and come close to touching their toes without bending their knees (Figure 5). Tight hamstrings can limit the amount of forward flexion. A single-legged hyperextension test can be performed to assess for possible injury to the posterior elements (Figure 6). Pain with flexion suggests injury to the anterior elements of the spine, or muscle strain/spasm. Pain with extension indicates injury to the posterior elements or sacroiliac joint.
Figure 5.

Adolescents should be able to come close to touching their toes with forward flexion of the spine.
Figure 6.

A single-legged hyperextension test, looking for pain in the posterior elements of the spine, is performed by having the patient stand on 1 leg and extend through the spine. A positive test provokes pain on the ipsilateral side to the standing leg.
Palpation of the spine and sacroiliac joints should be performed to assess for tenderness. The soft tissues, such as the paraspinal muscles and buttocks, should also be palpated for tenderness and to assess for muscle spasm.
Special tests in the examination of the lumbar spine include a figure-4 or FABER (flexion-abduction–external rotation) test, Gaenslen sign, and straight-leg test.25 The FABER test (Figure 7) and Gaenslen sign (Figure 8) assess the sacroiliac joint.19,25 The straight-leg test assesses for neural tension. With the patient supine, the examiner raises 1 leg until the patient reports severe pain in the back or buttock or the knee starts to bend. The ankle is then dorsiflexed to determine if the pain is increased. A patient who has no neural tension should be able to raise the leg close to 90° without pain.7,13
Figure 7.

The FABER (flexion-abduction–external rotation) test. The patient lies in the supine position on the examining table, with the hip flexed, abducted, and externally rotated and the foot on the opposite knee. The examiner then presses the flexed hip into the table while stabilizing the opposite hip. Pain in the back on the ipsilateral side as the hip is flexed is a positive test for sacroiliac joint pathology.
Figure 8.

Gaenslen sign. The patient lies supine on the examining table with 1 leg maximally flexed. The opposite leg is extended over the edge of the table. The examiner applies downward pressure on the hanging leg. Pain in the back elicited by this maneuver is a positive test for sacroiliac joint pathology.
The neurologic examination should assess motor strength, sensation, and deep tendon reflexes of the lower extremities. A hip examination should be done to rule out hip pathology, as well as an abdominal examination to rule out visceral pathology.
Specific Injuries
Spondylolysis
Sports involving repetitive extension and rotation of the lumbar spine, such as dance, figure skating, and gymnastics, increase the risk of injury to the posterior elements of the spine (Figure 1).24 Spondylolysis refers to a defect in the pars interarticularis, a stress fracture caused by repetitive extension and torsion of the spine (Figure 2). One study indicated that 47% of young athletes with back pain had spondylolysis.16 This occurs most often at L5 and more often on the left side.5
Bilateral spondylolysis at the same vertebral level can result in spondylolisthesis, the forward translation of 1 vertebra on the next caudal segment (Figure 9). Spondylolisthesis is graded according to the percentage of slip: grade I is a slip of 0% to 25%; grade II, a slip of 25% to 50%; grade III, a slip of 50% to 75%; and grade IV, a slip of >75%.
Figure 9.
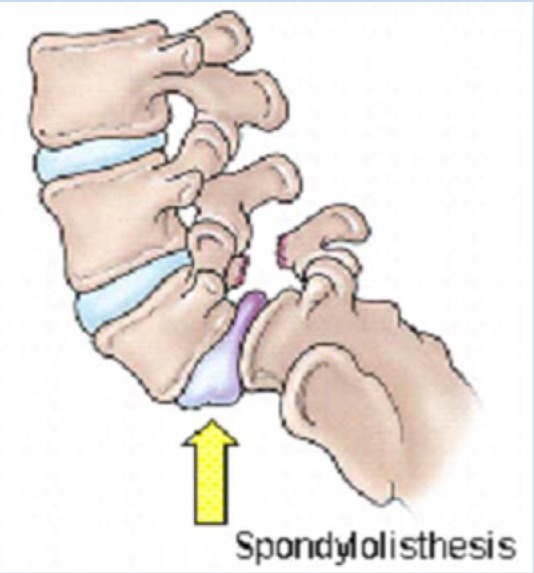
Spondylolisthesis of L5-S1.
Athletes with spondylolysis typically present with insidious onset of extension-related low back pain.2,11,15,25 Frequently, there is an associated reduction in hamstring flexibility. The athlete may complain of pain with impact, such as during running and jumping. Occasionally, radiating pain, numbness, or weakness may be present. These symptoms may make the diagnosis more difficult, as these symptoms also present with disc herniation.25
On examination, there may be hyperlordosis, ipsilateral paraspinal muscle spasm, and hamstring tightness. Pain is elicited with extension of the spine. The single-legged hyperextension test localizes the spondylolysis when standing on the ipsilateral leg (Figure 6),1,2,11,19,25 although recent evidence suggests that this may be an insensitive test.14 There may be focal tenderness to palpation.
Low back pain in the young athlete that has been present for more than 3 weeks should be investigated. Plain radiographs should be done initially (Figure 10).2,11,15 The anteroposterior view may identify anatomic variants or developmental defects, such as transitional vertebrae or spina bifida occulta (Figure 11), which is seen more frequently in patients with spondylolysis.22 The lateral view may demonstrate spondylolisthesis or a lytic lesion. Oblique views may demonstrate a stress reaction of the pars interarticularis, the pathognomonic “neck of the Scotty dog” lesion (Figure 10B). However, many institutions discourage the routine use of oblique views because of the increased dose of radiation and because only a third of stress fractures can be seen on plain radiographs.2,15
Figure 10.
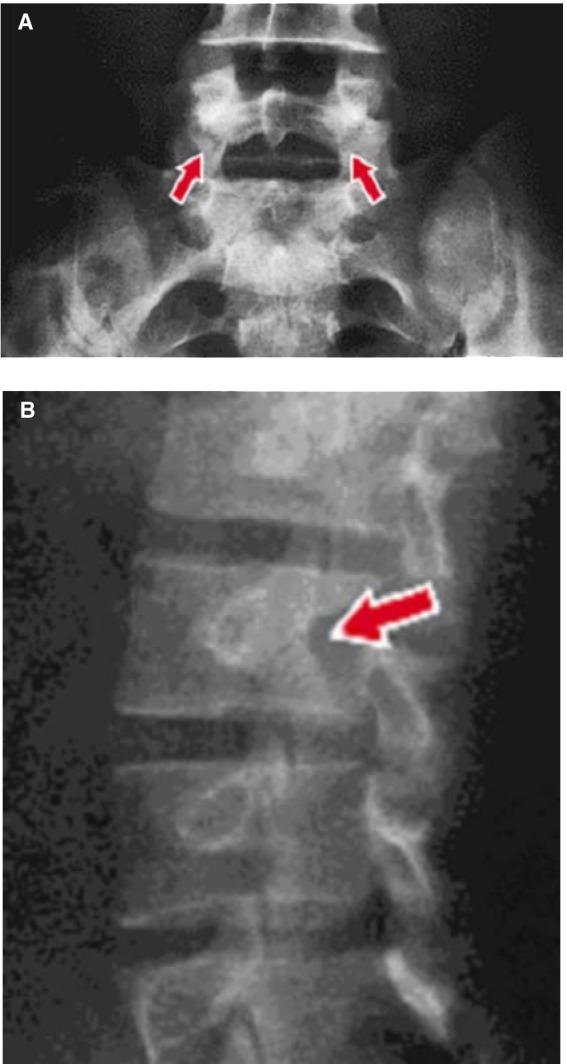
Anteroposterior radiograph (A) of lumbar spine. Arrows indicate sclerosis and fracture line of bilateral spondylolysis. Oblique radiograph (B) of lumbar spine. Arrow indicates sclerosis of the “neck of the Scotty dog.”
Figure 11.

Spina bifida occulta can be associated with spondylolysis.
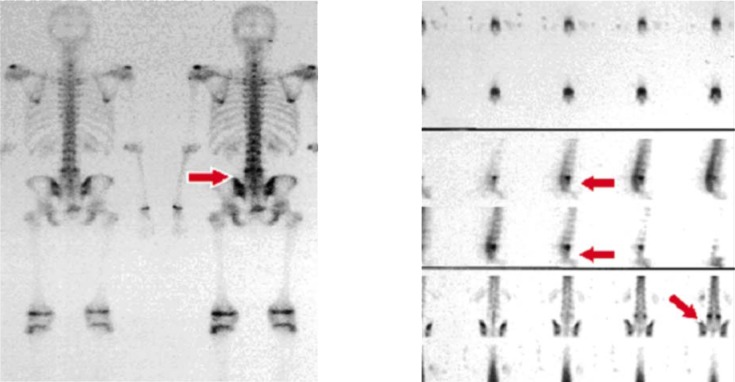
Plain radiographs should be followed up by single-photon emission computed tomography (SPECT) bone scan. Bony lesions in which active bony turnover is occurring are indicated by increased uptake on the bone scan (Figure 12).2,11,14,15,25
Figure 12.
Bone scan indicating an area of increased uptake consistent with spondylolysis.
Computed tomography can be used to confirm the presence of a pars interarticularis stress fracture and to monitor the process of healing (Figure 13).2,11 Because of the additional radiation involved in CT, some authors reserve CT scans for those patients not responding to treatment.25
Figure 13.
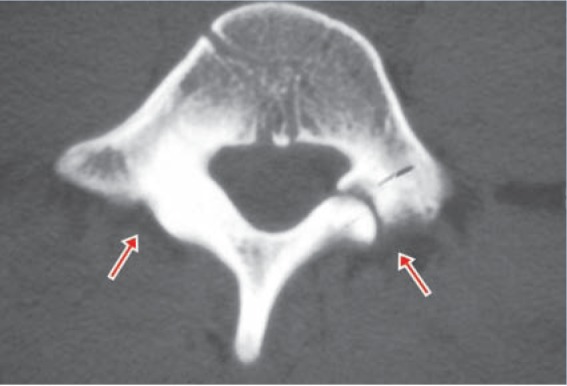
Computed tomography scan of lumbar vertebrae indicating a spondylolytic defect on the right and reactive sclerosis on the left.
Magnetic resonance imaging would be preferable because of the lack of ionizing radiation. However, MRI is not as sensitive for detecting spondylolysis as is a SPECT bone scan.14,25 A diagnostic algorithm for investigating spondylolysis is provided in Figure 14.
Figure 14.
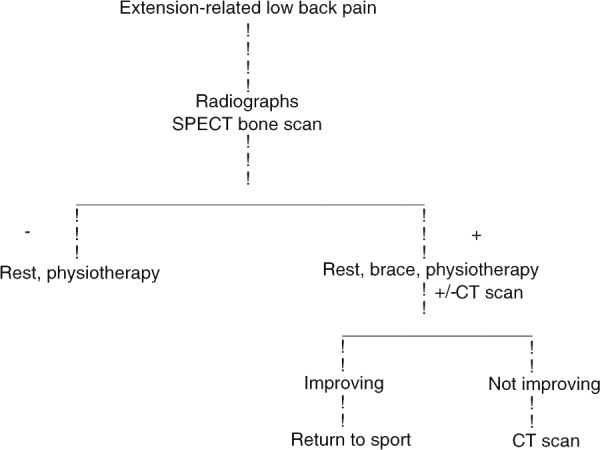
Diagnostic algorithm for investigation of spondylolysis.
Management of spondylolysis includes activity modification. Any activities that cause pain should be avoided, particularly extension activities. An exercise program including strengthening of the abdominal muscles, hip flexor and hamstring stretches, and antilordotic exercises for the lumbar spine should be initiated, either at home or under the supervision of a physiotherapist.4,19,25
Bracing is somewhat controversial. Some authors recommend early use of custom thoracolumbar orthoses to limit extension and rotation of the spine.1-3,9,11,15,22 Others simply restrict activities without bracing, in conjunction with physiotherapy.11,21 One study in young soccer players illustrated that the best results were obtained with a period of rest from sport for 3 months, regardless of whether bracing was used.17
Once the athlete becomes pain-free, activity can be gradually increased. If bracing is used, bracing continues until the athlete has resumed full activities without pain, and then the brace is gradually weaned until the athlete is participating fully with no pain.2,15 A patient who has resumed full pain-free activities out of the brace is considered clinically healed. Patients with spondylolisthesis should be followed every 4 to 6 months with standing lateral films until skeletal maturity to assess for progression of slip. Athletes are at low risk for worsening of spondylolisthesis. However, if the slip progresses beyond 50%, or if there are neurologic symptoms or persistent pain, surgical stabilization is indicated.2
Posterior Element Overuse Syndrome
Posterior element overuse syndrome, resulting from repeated extension and rotation of the spine, is a constellation of conditions involving muscle-tendon units, ligaments, facet joints, and joint capsules. It is also called hyperlordotic low back pain,2,16,19 mechanical low back pain, or muscular low back pain.1,11,19,20 After spondylolysis, it is the most common cause of low back pain in adolescents.14
Young athletes with posterior element overuse syndrome present with symptoms similar to those of spondylolysis. Pain is associated with extension of the spine and sometimes with rotation. There may be paraspinal muscle tenderness, as well as focal tenderness over the lower lumbar spine, adjacent to the midline. Imaging is typically negative, ruling out spondylolysis.
Management includes ice and nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and inflammation. Pain-free activities are permitted and extension of the spine is avoided. An exercise program emphasizing abdominal strengthening, antilordotic exercises, and hamstring and thoracolumbar stretches should be initiated at home or under the guidance of a physiotherapist.1,2,11,25 An antilordotic brace may be helpful in the short term.
Sacroiliac Joint
The sacroiliac (SI) joint disperses the forces between the trunk and the lower extremities. This joint can be a source of pain in young athletes because of excessive or reduced motion within the SI joint. Pathology of the lumbar spine can alter the mechanics of the lumbar spine, resulting in stress to the SI joints.25 Inflammation of the SI joint can also result in SI joint pain. SI joint inflammation can occur from infection, such as Reiter syndrome, as well as from seronegative spondyloarthropathies, such as Crohn disease, psoriatic arthritis, and juvenile ankylosing spondylitis. Another cause of SI joint pain is a stress fracture of the sacrum.25
Athletes with SI joint pain present with extension pain that is insidious in onset.11,25 On examination, pain is localized to the lumbar or buttock region with extension of the spine. They may have poor pelvic stability on Trendelenburg testing, as well as a positive FABER test (Figure 7). Palpation elicits tenderness over the affected SI joint.2,11,25
Plain radiographs should be obtained if symptoms have been present for more than 3 weeks. Bone scan may demonstrate a stress fracture of the sacrum. Magnetic resonance imaging can more precisely define the anatomic abnormality. If infection or a spondyloarthropathy is suspected, blood work, including erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, antinuclear antibody, and HLA-B27, should be obtained.25
Management of SI joint dysfunction includes ice, NSAIDs, activity modification, bracing, and physical therapy. Ice and NSAIDs help alleviate pain and inflammation. Activity should be restricted to those that do not provoke pain. If a sacral stress fracture is present, protected weightbearing is necessary until pain resolves.25 Bracing can help stabilize the joint. Physical therapy involves possible manipulation of the SI joint, pelvic stabilization exercises, and hip girdle and abdominal strengthening.2,4,11,25
Atypical (Lumbar) Scheuermann
Lumbar Scheuermann can present in athletes who participate in sports involving rapid flexion and extension, such as diving, rowing, and gymnastics.19 This results in end-plate fractures of the lumbar vertebrae, Schmorl nodes, and vertebral apophyseal avulsions visible on plain x-rays of the lumbar spine (Figure 15). Young athletes present with low back pain, a flat back (decreased thoracic kyphosis and lumbar lordosis) and tight thoracolumbar fascia.2 Management includes a physiotherapy program of stretching the thoracolumbar fascia and core stabilization exercises. Bracing in 15° of lordosis can help athletes return to their sport.1,2,19,25
Figure 15.

A lateral radiograph of the spine in a patient with Scheuermann kyphosis. The arrow indicates end-plate irregularities.
Vertebral Body Apophyseal Avulsion Fracture
Activities that involve repetitive flexion and extension of the spine can result in injury to the ring apophysis. Fractures of the cartilaginous ring apophysis may occur with displacement posteriorly into the spinal canal, along with the intervertebral disc (Figure 16).19,25
Figure 16.
Vertebral body apophyseal avulsion fracture.
Avulsion fractures occur most often in sports such as gymnastics, wrestling, volleyball, and weight lifting.19,25 Athletes present with lumbar pain on flexion of the spine. There are usually no associated neurologic symptoms. On examination, both spine flexion and extension are limited. There may be paraspinal muscle spasm. The neurologic examination is usually normal.
Lateral radiographs of the lumbar spine may show an ossified fragment in the canal. Computed tomography can better identify the fractured apophysis and displaced piece of bone, which may be missed on MRI.
Management consists of rest, heat, NSAIDs, and possibly massage for pain relief. If there are significant neurologic findings resulting from neural compression, the fragment may need to be surgically excised.1,19,25
Disc Herniation
Acute herniation of the nucleus pulposus is uncommon in young athletes. Adolescents present with flexion-related back pain, associated with back muscle spasm, hamstring tightness, and possibly buttock pain.2,23-25 Radicular symptoms in this age group are often not present.11,19 A potential complication of disc herniation is cauda equina syndrome.25 Cauda equina syndrome is caused by the compression of the nerves in the lower portion of the spinal canal and can result in the loss of bowel and bladder function, as well as paralysis of the legs. It is considered a surgical emergency because the deficits may be permanent if left untreated.25
On examination, there is usually decreased lumbar motion, particularly in flexion, a positive straight-leg raise, and possibly decreased reflexes and strength on the affected side. However, presentation can be quite variable. Pain may be mild to moderate, and sometimes severe. Patients may have a negative straight-leg test, or the back pain may be increased with a straight-leg test in the absence of radicular symptoms. Patients may have only flexion-related back pain without any other findings.
Lumbar radiographs should be obtained to rule out osseous injury. Magnetic resonance imaging studies can indicate the extent of the herniation and show nerve root impingement (Figure 17). Magnetic resonance imaging scans are usually obtained if symptoms are progressive or refractory to treatment.
Figure 17.

An MRI scan of the lumbar spine. There is a disc herniation at L5-S1.
Almost 90% of patients improve with conservative management.1,12,20 A temporary lordotic brace may allow for early resumption of daily activities. Physical therapy should be initiated to help relieve pain and to establish an extension-based stabilization program.1,2,19,24,25 Pain is managed with NSAIDs and, occasionally, epidural corticosteroids. Surgery is indicated if cauda equina is present, neurologic deficit is progressive, or if pain is refractory to conservative management.1,2,24,25 Athletes with disc herniation may return to activity once they have attained full pain-free range of motion, full strength, and have progressed through sport-specific activities in a controlled setting.2,19
Other Causes of Low Back Pain
Injury is not the only cause of low back pain in young athletes.2,6,9,20,25 Infection (discitis or osteomyelitis), inflammation (seronegative spondyloarthropathies), and tumors (eg, osteoid osteoma, osteoblastoma, bone cysts, Ewing sarcoma, osteogenic sarcoma) can also cause back pain, as well as visceral pathology such as pyelonephritis. A high index of suspicion is necessary to avoid missing these potential reasons for low back pain. Systemic symptoms such as fever, night pain, weight loss, and malaise are red flags for more sinister causes of back pain and should prompt further investigation.
Prevention
Although injuries are a part of sport, there are ways to reduce the risk of injury in young athletes. Recognizing risk factors are a key component to reducing injury.25 Prior to the start of a sport season, a preparticipation evaluation may identify certain risk factors, such as previous injuries that have not been fully rehabilitated or muscle weaknesses or inflexibility. These areas can then be addressed prior to the start of the season. Additionally, athletes should start general strength and fitness conditioning several weeks before the start of the season.19 Increases in the frequency and intensity of training should be gradual to allow for safe adaptation to the demands of the sport.
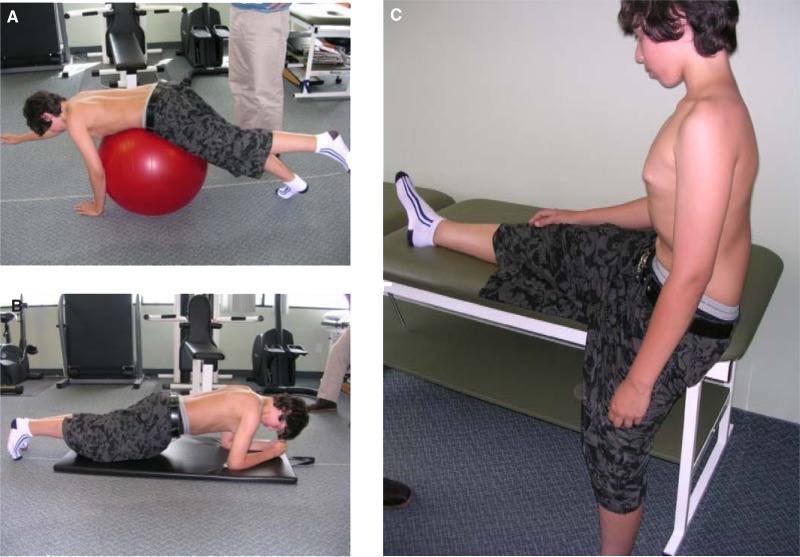
During periods of growth, young athletes are prone to loss of flexibility and muscle imbalances that can predispose them to injury.19,25 Because of this concern, young athletes should reduce the amount of training and the volume of repetitive motions during growth spurts. Certain sports require maneuvers that place a lot of stress on the posterior spine, such as layback spins in figure skating (Figure 1) and walkovers in gymnastics. Athletes may need to limit the number of repetitions of these maneuvers, particularly if there is pain associated with these maneuvers. Core-strengthening exercises and stretches for tight hamstrings and hip flexors may help reduce the risk of low back pain (Figure 18).19,25
Figure 18.
Core-strengthening exercises are part of rehabilitation for back injuries but can also be incorporated into conditioning programs to prevent injuries. Examples include: (A) using a stability ball, the athlete lies prone on the ball and extends the opposite hand and leg and holds this position for as long possible; (B) in the plank, the athlete rests on elbows and toes and holds back straight as long as possible. Hamstring stretches are also important in both conditioning and rehabilitation of back injuries. One way to stretch the hamstrings is to stand next to a table with 1 leg extended on the table. The athlete bends forward from the waist until a stretch is felt in the hamstrings of the extended leg (C).
Proper technique should be emphasized. For all athletes, correct posture to limit the amount of lordosis of the lumbar spine can help prevent injuries to the lumbar spine. In sports requiring lifting, such as pairs skating and dance, proper lifting techniques must be employed to prevent back injuries.25
In team sports, there can be large discrepancies in the sizes and relative strengths of participants on any given team. Attempts should be made to match athletes in size and strength to prevent injuries from contact with larger, stronger participants.19,25
Another important aspect of prevention is recognizing that back pain is not part of the sport. Increasing complaints of pain, particularly if it is interfering with activity, should be taken seriously and addressed early to avoid significant injury.25
Return-To-Play Guidelines
When an injured athlete is returning to sport, recommendations must take into account the diagnosis, the sport or activity, the age and skeletal maturity of the child, and the amount of cooperation of the athlete, parents, and coaches in allowing activity modifications during healing.19,25 In general, relative rest is indicated to allow for healing. Activities that cause pain should be avoided until the patient is pain-free. Most athletes are able to continue in their sport with modifications of the activity. Once the athlete has attained pain-free range of motion with all activities and has obtained normal strength, he or she can return to full sport participation.
Conclusion
Young athletes who present with low back pain are more likely to have structural injuries and therefore should be investigated fully. Muscle strain should be a diagnosis of exclusion. Treatment should address flexibility and muscle imbalances. Injuries can be prevented by recognizing and addressing risk factors. Return to sport should be a gradual process once the pain has resolved and the athlete has regained full strength.
Acknowledgments
We extend special thanks to Evan Karigianis, Melanie Lumsden, and Matthew Perrie for their invaluable help with photography.
Footnotes
No potential conflict of interest declared.
References
- 1. Brown TD, Micheli LJ. Spinal injuries in children’s sports. In: Maffuli N, Chan KM, Macdonald R, Malina RM, Parker AW, eds. Sports Medicine for Specific Ages and Abilities. London: Churchill Livingstone; 2001:31-44 [Google Scholar]
- 2. d’Hemecourt P, Gerbino PG, II, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000;19:663-679 [DOI] [PubMed] [Google Scholar]
- 3. d’Hemecourt P, Zurakowski D, Kriemler S, et al. Spondylolysis: returning the athlete to sports participation with brace treatment. Orthopedics. 2002;25:653-657 [DOI] [PubMed] [Google Scholar]
- 4. George SZ, Delitto A. Management of the athlete with low back pain. Clin Sports Med. 2002;21:105-120 [DOI] [PubMed] [Google Scholar]
- 5. Gregory PL, Batt ME, Kerslake RW, Webb JK. Single photon emission computerized tomography and reverse gantry computerized tomography findings in patients with back pain investigated for spondylolysis. Clin J Sport Med. 2005;15:79-86 [DOI] [PubMed] [Google Scholar]
- 6. Hollingworth P. Back pain in children. Br Rheumatol. 1996;35:1022-1028 [DOI] [PubMed] [Google Scholar]
- 7. Hoppenfeld S. Physical examination of the lumbar spine. In: Hoppenfeld S. Physical Examination of the Spine and Extremities. Upper Saddle River, NJ: Prentice Hall; 1976:237-263 [Google Scholar]
- 8. Hutchison MR. Low back pain in elite rhythmic gymnasts. Med Sci Sports Exerc. 1999;31:1686-1688 [DOI] [PubMed] [Google Scholar]
- 9. King HA. Back pain in children. Orthop Clin North Am. 1999;30:467-474 [DOI] [PubMed] [Google Scholar]
- 10. Kolt GS, Kirkby RJ. Epidemiology of injury in elite and subelite female gymnasts: a comparison of retrospective and prospective findings. Br J Sports Med. 1999;33:312-318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kraft DE. Low back pain in the adolescent athlete. Pediatr Clin N Am. 2002;49:643-653 [DOI] [PubMed] [Google Scholar]
- 12. Lively MW, Bailes JE., Jr Acute lumbar disk injuries in active patients: making optimal management decisions. Available at www.physsportsmed.com/index.php?art=psm_04_2005?article=71 Accessed March 20, 2009 [DOI] [PubMed]
- 13. Malina R. Growth and maturation: applications to children and adolescents in sports. In: Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Philadelphia: Lippincott Williams & Wilkins; 2002:39-58 [Google Scholar]
- 14. Masci L, Pike J, Malara F, Phillips B, Bennell K, Brukner P. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40:940-946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McTimoney CA, Micheli LJ. Current evaluation and management of spondylolysis and spondylolisthesis. Curr Sport Med Rep. 2003;2:41-46 [DOI] [PubMed] [Google Scholar]
- 16. Micheli LJ, Wood R. Back pain in young athletes. Arch Pediatr Adolesc Med. 1995;149:15-18 [DOI] [PubMed] [Google Scholar]
- 17. Rassi GE, Takemitsu M, Woratanarat P, Shah SA. Lumbar spondylolysis in pediatric and adolescent soccer players. Am J Sports Med. 2005;33:1688-1693 [DOI] [PubMed] [Google Scholar]
- 18. Semon RL, Spengler D. Significance of lumbar spondylolysis in college football players. Spine. 1981;6:172-174 [DOI] [PubMed] [Google Scholar]
- 19. Simon LM, Jih W, Buller JC. Back pain and injuries. In: Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Philadelphia: Lippincott Williams & Wilkins; 2002:306-325 [Google Scholar]
- 20. Sponseller PD. Evaluating the child with back pain. Am Fam Phys. 1996;54:1933-1941 [PubMed] [Google Scholar]
- 21. Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000;34:415-422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Steiner ME, Micheli LJ. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine. 1985;10:937-943 [DOI] [PubMed] [Google Scholar]
- 23. Trainor TJ, Trainor MA. Etiology of low back pain in athletes. Curr Sport Med Rep. 2004;3:41-46 [DOI] [PubMed] [Google Scholar]
- 24. Watkins RG. Lumbar disc injury in the athlete. Clin Sport Med. 2002;21:147-165 [DOI] [PubMed] [Google Scholar]
- 25. Zetaruk M. Lumbar spine injuries. In: Micheli LJ, Purcell LK, eds. The Adolescent Athlete. New York: Springer; 2007:109-140 [Google Scholar]