Figure 6.
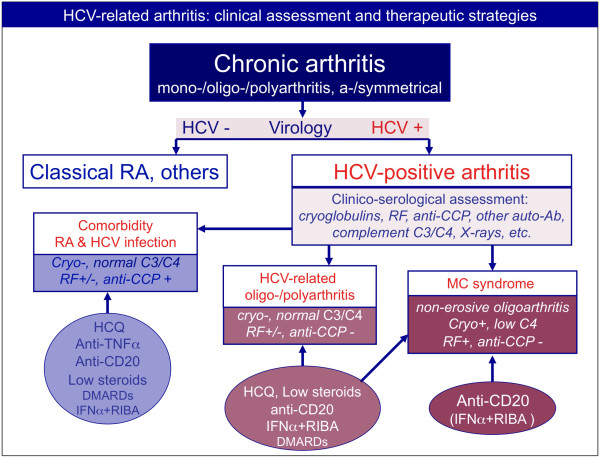
Differential diagnosis among patients with arthritis and concomitant hepatitis C virus infection, and therapeutic strategies. Clinico-serological and virological work-up is mandatory in patients presenting with chronic arthritis. Patients with polyarthritis and hepatitis C virus (HCV) infection can be classified as either having simple comorbidity, that is, HCV infection and rheumatoid arthritis (RA) or other forms of chronic arthritis, or having HCV-associated arthritis. This latter may represent one extrahepatic manifestation of HCV infection or it can be a symptom of MCs. The comorbidity may be treated with the standard therapeutic strategies for RA, with some precautions because of concomitant viral infection, in particular for methotrexate and leflunomide. On the contrary, biologics (anti-TNFα and anti-CD20 rituximab) have been usefully employed without significant side effects in HCV-positive RA patients. The antiviral therapy of IFNα plus ribavirin (RIBA) can also be employed after careful hepatologic evaluation of patients. Interestingly, anti-TNFα, rituximab, and cyclosporine A seem to have a potential synergistic effect if associated with antiviral treatment (IFNα + RIBA). Usually, HCV-associated arthritis is poorly aggressive and may respond to low doses of steroids and hydroxychloroquine (HCQ). The use of other disease-modifying anti-rheumatic drugs (DMARDs) presents the above-mentioned limitations, while rituximab may be usefully employed, especially in patients with more aggressive arthritis. Finally, rituximab may represent the first-choice treatment in patients with arthritis in the setting of MCs. Ab, antibody; CCP, cyclic citrullinated peptide; RF, rheumatoid factor.
