Abstract
Objective
Family factors such as conflict, blame, and poor cohesion have been found to attenuate response to cognitive behavior therapy (CBT) for pediatric obsessive compulsive disorder (OCD). This study examined the feasibility and acceptability of a brief, personalized intervention for cases of pediatric OCD complicated by these family features.
Method
Twenty youth with a primary DSM-IV diagnosis of OCD (mean age = 12.50 years; 55% male; 60% Caucasian) and their families participated. To be included in the study, families were required to evidence poor functioning on measures of blame, conflict, and/or cohesion. Eligible families were randomly assigned to either standard treatment (ST) with 12 weeks of individual child CBT that included weekly parent check ins and psychoeducation or to Positive Family Interaction Therapy (PFIT), which consisted of 12 weeks of individual child CBT plus an additional six sessions of family treatment aimed at shifting family dynamics. Clinical outcomes were determined by blind independent evaluators using the Clinician's Global Impressions-Improvement (CGI-I) scale.
Results
All families completed the study. High levels of satisfaction were reported among participants in both arms of the study, despite the added burden of attending the PFIT sessions. Both mothers and fathers attended 95% of the PFIT family sessions. Families in the ST condition demonstrated a 40% response rate on the CGI-I; families in the PFIT condition demonstrated a 70% response rate. Treatment gains were maintained in both conditions at 3-month follow-up.
Conclusions
Preliminary data suggest that PFIT is acceptable and feasible. Further testing and treatment development are needed to optimize outcomes for complicated cases of pediatric OCD.
Keywords: Family treatment, obsessive compulsive disorder, feasibility
Research examining effective interventions for pediatric obsessive compulsive disorder (OCD) has produced evidence in favor of both cognitive behavior therapy (CBT) and pharmacotherapy with serotonin reuptake inhibitors (SRIs) with respect to decreasing OCD symptomatology and impairment (Barrett et al., 2008; POTS, 2004). Despite their success in reducing symptoms, however, researchers and clinicians continue to struggle with the fact that many youth fail to respond to treatment or exhibit only partial response (Barrett et al., 2008; Ginsburg, Kingery, Drake, & Grados, 2008). Indeed, nearly 50% of youth completing treatment for OCD may be left with lingering symptoms (POTS, 2004). Efforts to understand the needs of these youngsters have focused on predictors of poor treatment response, with features such as baseline symptom severity, comorbidity, and family functioning frequently linked to poor outcome (Garcia et al., 2010; Ginsburg et al., 2008; Storch et al., 2010). Among these variables, family factors are of particular interest given the central role that families play in helping children adhere to treatment and maintain therapeutic gains. Recent research reveals several family variables that may influence treatment outcome for pediatric OCD, including parental OCD, accommodation of OCD symptoms, family conflict, blame, and cohesion (Garcia et al., 2010; Merlo, Lehmkuhl, Geffken, & Storch, 2009; Peris et al., 2012; Piacentini et al., 2011). Despite their relevance for outcome, however, interventions specifically targeting these variables are in short supply.
This paper presents preliminary data from a pilot feasibility trial of Positive Family Interaction Therapy (PFIT), a six-session family therapy module designed for use as an adjunct to individual child CBT in cases of OCD characterized by increased levels of family dysfunction. PFIT builds on prior research to provide a personalized intervention for pediatric OCD that co-occurs with challenging family dynamics such as conflict, blame, and poor cohesion. PFIT is distinct from existing family interventions in its emphasis on parental emotion regulation, family problem-solving, and careful functional analysis of family dynamics that may undermine successful exposure exercises.
Families may affect the treatment process in several ways, but perhaps the most direct influence is through their role in exposure exercises which are generally viewed as the central component to successful OCD treatment. Whether by issuing reminders for practice or participating in exposures directly, parents must understand the rationale for these exercises, appreciate their importance, and tolerate the anxiety they provoke (Freeman et al., 2003). Moreover, as family accommodation of OCD symptoms is common (Storch et al., 2007), exposures often involve family disengagement from symptoms, a challenging task for parent and child alike. It is no surprise then, that family therapy has been encouraged as an adjunct to individual child treatment (AACAP, 1998), and some form of family involvement is the norm in virtually all child CBT protocols.
Several groups have examined the efficacy of family-based treatments for OCD (or FCBT), finding support for its ability to decrease symptoms of OCD and related impairment and finding evidence that FCBT produces favorable effects when delivered in individual and group formats (Barrett, Healy-Farrell, & March, 2004), over intensive and weekly visits (Storch et al., 2007), and when compared to active alternative treatment (Freeman et al., 2008; Piacentini et al., 2011). Moreover, response to FCBT has been maintained up to seven years post-treatment (O'Leary, Barrett, & Fjermestad, 2009) underscoring the durability of this approach.
Despite these positive developments, pressing issues remain. First the incremental efficacy of family therapy for OCD remains to be examined, and it is still unclear what, if anything, it adds above and beyond individual child treatment. Second, although current family treatments have performed admirably with respect to decreasing OCD symptomatology (Piacentini et al., 2011; Storch et. al. 2007), they have been less successful at shifting relevant family dynamics. With the exception of a few studies that have produced changes in family accommodation (Piacentini et al., 2011; Storch et al., 2007), most treatments have not facilitated shifts in conflict, cohesion, or other indicators of family dysfunction (Barrett et al., 2004; Freeman et al., 2008; Storch et al., 2007). This is not surprising given that most family treatments rely heavily on psychoeducation and general behavior management techniques which may be insufficient to change entrenched family dynamics. Aspects of broader family functioning typically have not been direct targets of family treatment. However, as evidence mounts for their role in CBT outcome, there is a need for tailored interventions that address these potential barriers to treatment.
Recent research suggests that affective family dynamics may be especially important. For example, Peris et al. (2012) found that only 10% of youngsters from families characterized by high levels of family conflict and blame and low levels of family cohesion were rated as responders to FCBT compared to a 93% response rate for youth from families with normative functioning on these variables. Although work in this area is just beginning to emerge, similar factors have been found important for child anxiety (Hudson & Rapee, 2005) and have been targeted in FCBT protocols for anxious youth (Silverman, Kurtines, Jaccard & Pina, 2009). The fact that families exert powerful influences on OCD treatment outcome, makes them logical targets for intervention, a point underscored by recent literature reviews (Ginsburg et al., 2008) and expert practice parameters (AACAP, 1998).
PFIT was developed as a personalized treatment for highly distressed and impaired families of youth with OCD. The treatment integrates aspects of traditional psychoeducation and parent training, but moves beyond typical protocols through its integration of emotion regulation exercises, individually-tailored functional analysis aimed at identifying the unique function of symptoms in the family context, and joint problem-solving techniques. These skills are thought to be central to helping highly distressed families navigate the demands of exposure-based treatment.
As part of the current feasibility trial, participants were randomly assigned to standard treatment with child CBT augmented with either some degree of family involvement (ST) or with six sessions of PFIT. At this preliminary stage of treatment development, the trial focused on establishing the acceptability and tolerability of the PFIT module. The specific goals were to examine (a) recruitment and retention of a high stress, less stable population of families and (b) patient satisfaction following PFIT administration. Although under-powered for examination of treatment effects and not a central focus at this stage of treatment development, we were also interested in a preliminary inspection of response rates in both treatment conditions.
Method
Participants
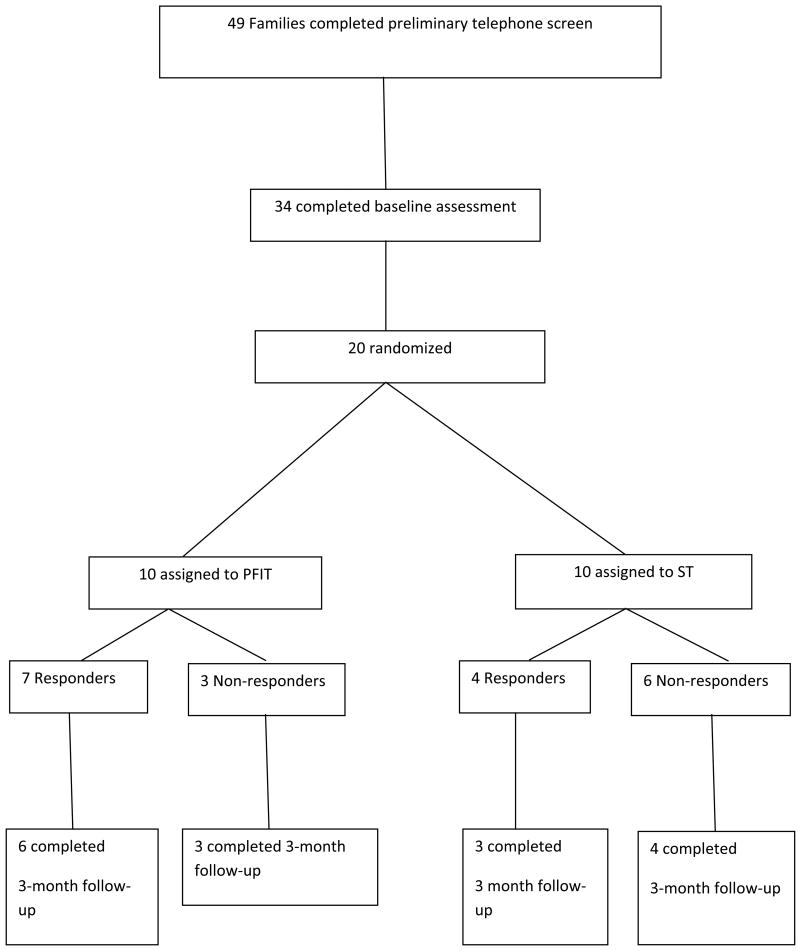
This study was conducted in an outpatient OCD specialty clinic housed in a large academic medical center. Participants were 20 treatment-seeking youth aged 8-17 (mean age=12.35 years; 55% male) and their families. Eligibility criteria included (a) a primary diagnosis of OCD as determined by DSM-IV-TR criteria (APA, 2004); (b) a score of 15 or higher on the Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997); and (c) high levels of family distress as demonstrated by elevations on at least two out of three measures of family functioning (conflict, blame, and cohesion as indicated below). Elevations on these measures were determined using previously established cut-points (Peris et al., in press); (d) no failed CBT trials for anxiety or OCD within the last two years; (e) both parent and child spoke sufficient English to participate in family therapy; (f) did not meet criteria for a comorbid psychiatric illness for which exposure-based CBT was contraindicated (e.g., schizophrenia, conduct disorder); youngsters with other co-occurring secondary diagnoses were allowed to participate. Youth on a stable dose of psychotropic medication were also allowed and 20% of participants were taking an SRI medication at intake. Of 49 families contacting the program, 34 completed baseline assessments and 20 were eligible and entered the trial (Figure 1).
Figure 1.
Study enrollment and retention.
Overall, 60% of youth self-identified as Caucasian, 15% Latino, 15% Persian, and 10% African American. Most (75%) came from homes with intact marriages. Among youth in divorced families, two had no contact with their fathers (one due to death of the father and the other due to paternal drug use); these two participants were randomized to ST. One participant lived with his paternal grandparents due to the level of conflict in the home and had separate weekly visits with each parent.
Measures
Anxiety Disorders Interview Schedule Child and Parent Versions (ADIS-C/P; Silverman & Albano, 1996)
A semi-structured psychiatric diagnostic interview, was used to determine study eligibility. A clinical severity rating (CSR) of 4 or higher on a 0-8 scale is indicative of clinically significant disorder and was required for a diagnosis of OCD. The ADIS has demonstrated sound psychometric properties (Silverman, Saavedra, & Pina, 2001), and interviewers were trained according to the procedures set forth by instrument developers. Although we did not conduct a formal reliability assessment, studies from this program utilizing similar training and supervision procedures as the present study have demonstrated excellent agreement on OCD diagnosis (k = .89) between diagnosticians and a best-estimate derived from a consensus case conference procedure (Piacentini et al., 2011).
Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997)
Is a semi-structured clinician-rated measure consisting of 10 items rated on a 5-point Likert scale. Separate scores are computed for obsessions and compulsions, and a total severity score is determined by summing all 10 items. The CY-BOCS possesses adequate internal consistency and convergent and discriminant validity (Storch et al., 2004). In the present sample, Cronbach's α= .71 for the total score. Inter-rater reliability ICC= .98.
Family Environment Scale (FES, Moos &Moos, 1994)
The FES is a 90-item self-report measure designed to tap ten domains of family social functioning. In the present study, parents completed the following two subscales: Cohesion, or the degree to which family members support each other (α= .62), and Conflict, a measure of overt discord among family members (α= .76).
Family Accommodation Scale (FAS; Calvocoressi et al, 1999)
Is a 13-item clinician-administered measure assessing the degree to which relatives of persons with OCD have accommodated symptoms over the preceding month. It measures both behavioral involvement in symptoms (e.g., participation in rituals) and the level of family distress and associated with this involvement. The FAS has good internal consistency and inter-rater reliability (Calvocoressi et al., 1999).
Parental Attitudes and Behaviors Scale (PABS; Peris et al., 2008b)
Is a 24-item parent-report measure of attitudes and behaviors related to their child's OCD with good concurrent and predictive validity (Peris et al., 2008b). The PABS consists of three scales: Blame, Accommodation, and Empowerment; the Blame scale was used in the present investigation (Cronbach's α= .96).
Clinical Global Impression –Improvement Scale (CGI-I, NIMH, 1985)
Is an IE-rated global measure of clinical improvement from baseline with scores ranging from 1 (very much improved) to 7 (very much worse) with youth rated as 1 (very much improved) or 2 (much improved) considered treatment responders. Independent review of 30% (n= 6) of cases revealed excellent agreement (r=.95) on post-treatment CGI-I ratings.
Attendance and Satisfaction
Patient Satisfaction with PFIT
Was rated by parents at treatment completion on a 7-item inventory that included items such as, “To what extent has this program met your needs?” and “If a friend's child were in similar need, would you recommend the program?” Items were rated on a 4-point Likert scale with 0=not at all and 4=very much (maximum score= 28).
Attendance
Was measured via the number of individual sessions attended by the child and the number of family sessions (i.e., the parent portion of ST or the family sessions in PFIT) attended by at least one parent. Within PFIT, separate attendance rates for mothers, fathers, siblings, and other family members were also calculated.
Attrition
Subject retention was indicated by the number of sessions completed at baseline and at the follow-up assessment.
Procedure
This study was conducted in compliance with the University Institutional Review Board (IRB). Interested families participated in a brief telephone screen to ascertain eligibility and those appearing to qualify then completed the informed consent/assent process and a baseline evaluation with an independent evaluator (IE). IEs were trained to criterion on the ADIS-IV and CY-BOCS using procedures established by the instrument developers, and they administered these interviews, along with the FAS, jointly to parents and children. Additional self-report measures were also completed as part of the baseline evaluation.
Eligible families were randomly assigned to either standard treatment (ST) or to PFIT. In both conditions, the 12 child sessions were delivered over 14 weeks with the last two sessions held every other week. Both length and amount of therapy were equated across groups. IEs remained blind to study condition and completed assessments at mid-treatment, post-treatment, and 3-month follow-up. Several efforts were made to protect the blind, including the scheduling of assessments on days separate from treatment sessions, storing IE and therapist charts in separate locked cabinets, and verbal reminders from both RAs and IEs to families not to identify their treatment condition during their assessment.
Treatment Conditions
Standard Treatment (ST)
The standard treatment used in this study was based on an existing CBT manual for pediatric OCD (Piacentini, Langley, & Roblek, 2007) and consisted of twelve 90-minute sessions, the first 60 minutes of which were devoted to exposure and response prevention (ERP) and cognitive restructuring with the child. The remaining 30 minutes were spent with parents for weekly check-in and psychoeducation about OCD and the role of the family in OCD treatment. In the present study, the family component of ST focused primarily on psychoeducation about OCD and the ERP model, the importance of disengaging from OCD symptoms, and the range of emotional responses to OCD. Therapists were allowed to encourage parents to attempt to refrain from accommodation; however, they did not provide specific guidance on how to do this and no specific behavior management techniques were provided.
PFIT
Youth in the PFIT arm of the study received the same 12 sessions of individual child ERP as outlined above (60 minutes each). However, the standard 30 minute weekly family component was replaced with one hour of family therapy (PFIT) every other week following the individual child session. The PFIT protocol outlines a more intensive family therapy module designed specifically to address familial responses of conflict and blame and to enhance cohesion. In addition to psychoeducation about OCD and the principles of CBT treatment, families participate in weekly exercises designed to enhance emotion regulation and problem solving. This includes functional analysis of difficult family situations related to OCD as well as practice with negotiating effective solutions. Families practice weekly exercises to promote supportiveness and cohesion as well as exercises aimed at enhancing emotion regulation (e.g., emotion labeling and monitoring, relaxation, and disengagement from arousing situations). They also gain experience with family-problem solving related to OCD and exposure exercises, via practice with joint problem solving, negotiation, scaffolding, and communication skills.
Therapist Training and Supervision
Treatment was administered by four study therapists, three Ph.D.-level clinicians and one graduate student with weekly supervision from the study PIs. Independent raters completed treatment integrity ratings on a random sample of 15% (n= 9) of PFIT session tapes using forms developed for this study. These forms measured adherence to the treatment protocol using a three-point Likert scale to rate key areas of each session's content. All tapes received adherence ratings of 86% (of the total possible points) or higher.
Results
Independent samples t-tests and chi square analyses were used to examine pre-treatment differences between the PFIT and ST groups. No baseline group differences in OCD symptom severity or demographics emerged, although ST youth were significantly younger and had fathers who were significantly more blaming (see Table 1).
Table 1. Child and Parent Baseline Characteristics.
| Measures | PFIT (N=10) | ST (N=10) | Full Sample (N=20) |
|---|---|---|---|
| Child Measures | |||
| Agea | 11.5 (1.90) | 13.20 (2.97) | 12.35 (2.58) |
| Gender (% Male) | 50% | 60% | 55% |
| CY-BOCS Total | 25.50 (2.87) | 25.40 (4.25) | 25.45 (3.53) |
| CGI-S | 5.40 (.52) | 5.40 (.85) | 5.45 (.69) |
| CGAS | 54.70 (4.30) | 53.50 (4.25) | 54.10 (4.20) |
| Family Measures | |||
| FES Cohesion-Mother | 7.00 (2.23) | 5.8 (1.48) | 6.37 (1.92) |
| FES Cohesion-Father | 5.67 (2.78) | 6.13 (1.89) | 5.88 (2.34) |
| FES Conflict-Mother | 6.11 (1.90) | 5.50 (1.84) | 5.79 (1.84) |
| FES Conflict-Father | 5.22 (1.86) | 6.13 (1.13) | 5.65 (1.58) |
| PABS Blame-Mother | 13.56 (5.03) | 17.67 (10.27) | 15.88 (8.22) |
| PABS Blame-Fathera | 15.50 (3.67) | 20.43 (8.71) | 17.56 (6.66) |
| Family Accommodation Scale | 25.90 (10.98) | 26.50 (8.25) | 26.20 (9.46) |
Note:
p < .05. CY-BOCS = Children's Yale-Brown Obsessive Compulsive Scale (Scahill et al., 1997); CGI-S = Clinician's Global Impressions-Severity Scale (Guy, 1976); CGAS = Clinician's Global Assessment Scale (Cite); FES= Family Environment Scale (Moos & Moos, 1994); PABS = Parental Attitudes and Behaviors Scale (Peris et al., 2008). For FES Conflict, higher scores indicate lower levels of conflict. For FES Cohesion, higher scores indicate better family functioning. For the PABS, higher scores reflect higher levels of blame.
Attendance
Families in both conditions attended all sessions. For families receiving PFIT, both mothers and fathers attended 95% of the family sessions together (9/10 families had perfect session attendance by both parents; in the remaining family, divorced parents attended three sessions together, with the mother attending one and the father two sessions on their own). One participant had grandparents who attended all six family sessions along with his parents. Among PFIT participants with siblings (n=5), 60% had a sibling who joined for at least one session.
Drop-out
No families dropped out of acute treatment, and 80% completed the 3-month follow-up. Two of the families that did not return for follow-up were ST participants and two were PFIT participants.
Satisfaction
Families reported similarly high levels of satisfaction for both treatment conditions despite the added burden of PFIT sessions which focused on emotion laden issues (Table 2).
Table 2. Feasibility and Acceptability.
| Measure | PFIT | ST |
|---|---|---|
| Attrition (% Drop-out) | 0 | 0 |
| Weeks to Completion | 15.97 | 14.30 |
| Satisfaction-Mother (n = 20) | 24.90 (4.61) | 24.1 (3.47) |
| Satisfaction-Father (n = 12) | 26.71 (1.50) | 19.60 (1.34) |
Note: With one outlier removed, the average PFIT satisfaction score for mothers = 26.22, p = .06.
Clinical and Family Outcomes
Overall, 70% of youth randomized to PFIT were designated responders on the Week 14 CGI-I compared to 40% of youth receiving ST. There was an average 5-point difference between conditions on the Week 14 CY-BOCS yielding a medium effect size (d = .65) for PFIT (Table 3). Remission rates were 50% for PFIT compared to 20% for ST CYBOCS ≤10; (POTS, 2004). Youth in both conditions maintained their gains at 3-month follow-up. Families receiving PFIT showed decreases in accommodation, blame, and family conflict over the course of the study, with mothers receiving PFIT reporting significantly lower blame at Week 24 compared to those receiving ST (Table 4).
Table 3. Pre- and Post-Treatment Primary Outcome Measures.
| Week 0 | Week 14 | Week 24 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| PFIT | ST | PFIT | ST | PFIT | ST | |
| CY-BOCS | ||||||
| Mean | 25.50 | 25.40 | 11.00 | 16.10 | 13.25 | 15.25 |
| SD | 2.88 | 4.25 | 7.37 | 8.27 | 8.43 | 5.52 |
| CY-BOCS Δ | ||||||
| Mean | -- | -- | -14.50 | -9.30 | -13.25 | -9.63 |
| SD | -- | -- | 8.99 | 8.54 | 5.34 | 8.77 |
| CGAS | ||||||
| Mean | 54.70 | 53.50 | 68.00 | 62.78 | 67.75 | 62.16 |
| SD | 4.30 | 4.25 | 7.11 | 10.41 | 7.75 | 6.01 |
Note: n= 20 at Weeks 0 and 14; n = 16 at Week 24. PFIT = Positive Family Interaction Therapy; ST= Standard treatment with individual child CBT plus a weekly family check-in. CY-BOCS = Children's Yale-Brown Obsessive Compulsive Scale. CGAS= Clinician's Global Assessment Scale.
Table 4. Pre- and Post-Treatment Secondary Outcome Measures.
| Week 0 | Week 14 | Week 24 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| PFIT | ST | PFIT | ST | PFIT | ST | |
| FAS | ||||||
| Mean | 25.90 (10) | 26.50 (10) | 7.90 (10) | 14.50 (10) | 8.50 (8) | 14.50 (8) |
| SD | 10.97 (10) | 8.25 (10) | 5.95 (10) | 8.55 (10) | 9.21 (8) | 7.41 (8) |
| Maternal Blame | ||||||
| Mean | 14.00 (10) | 17.70 (10) | 11.50 (9) | 15.56 (6) | 10.63 (8)* | 17.71 (7) |
| SD | 4.74 (10) | 9.68 (10) | 1.64 (9) | 8.20 (6) | 2.07 (8) | 9.41 (7) |
| Paternal Blame | ||||||
| Mean | 15.50 (10)* | 20.00 (8) | 12.33 (6)* | 18.29 (7) | 11.42 (7) | 18.40 (5) |
| SD | 3.50 (10) | 8.16 (8) | 1.75 (6) | 8.01 (7) | 3.36 (7) | 6.99 (5) |
| Maternal Cohesion | ||||||
| Mean | 7.20 (10) | 5.80 (10) | 7.00 (6) | 6.00 (7) | 7.25 (8) | 7.57 (7) |
| SD | 2.20 (10) | 1.48 (10) | 1.79 (6) | 1.33 (7) | 1.58 (8) | 1.72 (7) |
| Paternal Cohesion | ||||||
| Mean | 6.00 (10) | 6.13 (8) | 7.40 (6) | 5.86 (7) | 7.00 (7) | 6.40 (5) |
| SD | 2.82 (10) | 1.89 (8) | 1.52 (6) | 1.95 (7) | 2.38 (7) | 1.14 (5) |
| Maternal Conflict | ||||||
| Mean | 6.20 (10) | 5.50 (10) | 6.33 (6) | 4.20 (10) | 7.13 (8) | 4.43 (7) |
| SD | 1.81 (10) | 1.84 (10) | 1.63 (6) | 1.23 (10) | 1.81 (8) | 1.40 (7) |
| Paternal Conflict | ||||||
| Mean | 5.00 (10) | 6.13 (8) | 6.50 (6) | 4.57 (7) | 6.29 (7) | 4.00 (5) |
| SD | 1.89 (10) | 1.13 (8) | 2.35 (6) | 2.57 (7) | 1.80 (7) | 1.87 (5) |
Note:
significant group difference p = .01. Conflict and Cohesion were measured using the respective scales of the Family Environment Scale with higher scores on both measures reflecting better family functioning (i.e., high conflict score = low levels of family discord). n for each group at each time-point is listed in parentheses. All families (n = 20) completed the FAS at baseline and post-treatment (Week 14) via clinical interview with the IE and all mothers (n= 20) and available fathers (n = 18 as two subjects had no contact with their fathers) had complete data at baseline. Four families were lost to follow-up at Week 24 (two in each condition) with remaining missing data due to (a) only one parent completing measures at the assessment visit (b) incomplete completion of study measures or (c) telephone assessment with families who did not mail in their self-report forms.
Discussion
This study examined the feasibility of implementing a brief family intervention for youth with pediatric OCD complicated by challenging family dynamics. Building on research suggesting that conflict, blame, and low cohesion attenuate response to CBT, we recruited families with poor functioning in these areas and targeted these variables with a 6-session family treatment delivered adjunctively to ST. Preliminary data provide support for the feasibility of recruiting and retaining these families and for the acceptability of PFIT to families.
Given that PFIT was developed to reach patients struggling with complex, dysfunctional family dynamics, an overarching question pertained to whether these families would respond to outreach efforts and complete treatment successfully. Our experiences thus far suggest that high conflict, low cohesion families are eager for family treatment and committed to attending sessions. Indeed, we found high levels of involvement from mothers, fathers, and other family members during PFIT sessions as well as high levels of satisfaction with the treatment despite the added time burden and, at times, highly emotional content. Given that PFIT sessions bring high conflict families together to work on emotion-laden family problems related to OCD, their satisfaction with the family treatment is heartening. In addition, preliminary data suggest that the family recruitment criteria used in this study resulted in a more ethnically diverse sample than those found in typical pediatric OCD studies (Barrett et al., 2008). To the extent that PFIT may eventually help under-served populations, these early data are encouraging.
To our knowledge, PFIT is among the first tailored interventions for pediatric OCD. It builds on research identifying family-level predictors of CBT treatment response (Garcia et al., 2010; Peris et al., 2012) to identify specific family targets and techniques and its strategies mark a departure from extant family treatments. In particular, they move beyond psychoeducation and basic behavior management techniques to address emotion regulation, cohesion, and problem solving in the family system. Although not powered for a comparison of clinical outcomes, and indeed, not the primary focus at this preliminary stage, the present findings provide some indication of the utility of PFIT for high stress, high conflict families of youth with OCD, with effect sizes in the medium range.
Notably, this pilot trial employed an active comparison group with the goal of exploring early on how PFIT performed relative to the current gold standard treatment. The rigorous comparison group, which also specified some degree of family involvement, equalized therapist contact across conditions and enhanced the credibility of the control treatment. To our knowledge, this is among the first studies to examine the use of a tailored family treatment for pediatric OCD complicated by challenging family dynamics. The present findings provide some indication of the benefits of such treatment for homes characterized by conflict, blame, and poor cohesion. Indeed, only 40% of youth in the ST arm were designated treatment responders, a finding that closely parallels earlier research indicating that youth in families with poor functioning on these variables respond more poorly to family focused CBT compared with youth who have no such difficulties (Peris et al., 2012). Thus, the present findings provide further indication that conflict, blame, and cohesion may be important targets for family OCD interventions.
Naturally, these preliminary data must be interpreted in light of several limitations. First, given that this study pilot tested an intervention that may only be appropriate for a subset of families of youth with OCD, its sample size was small. Future studies with larger samples are needed to more definitively test the efficacy of the intervention and to examine its mechanisms of action. Second, in keeping with many clinical trials, there was missing data at follow-up, especially from fathers, despite generally encouraging subject retention. This is particularly problematic for interpretation of secondary family outcome measures. Third, the follow-up period was relatively brief and it will be important to assess potential maintenance of treatment gains over a longer period of time.
Implications for Research, Policy, and Practice
These limitations notwithstanding, this study marks an important step towards attempting to provide personalized care for youth with OCD. There has been a growing call for prescriptive intervention (Insel, 2006), and, in particular, for efforts to reach youth at high risk for treatment non-response. The present findings speak to the value of pursuing this line of treatment development, as they provide some indication that families are willing and able to participate and that their involvement may enhance clinical outcomes. Whether changes in family functioning mediate treatment outcome remains an open question. Future studies with larger samples are needed in order to assess more definitively what this family treatment module adds relative to individual child treatment, how it compares to other family treatments, and whether it offers advantages with respect to time course of response or long-term maintenance of gains.
Acknowledgments
This research was supported by grants from the Obsessive Compulsive Foundation (Piacentini, Peris), a NARSAD Young Investigator Award (Peris), and NIMH K23 MH085058 (Peris). We gratefully acknowledge the contributions of Katharina Kircanski, Shannon Bennett, Joyce Lee, Lynn Lim and the families who participated in this project.
References
- American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:27S–45S. doi: 10.1097/00004583-199810001-00003. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000. [Google Scholar]
- Barrett PM, Healy-Farrell L, March JS. Cognitive behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Farrell L, Pina AA, Peris TS, Piacentini J. Evidence-based psychosocial treatments for child and adolescent obsessive compulsive disorder. Journal of Clinical Child and Adolescent Psychology. Special Issue: Evidence-based psychosocial treatments for children and adolescents: A ten year update. 2008;37:131–155. doi: 10.1080/15374410701817956. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Mazure C, Kasl S, Skolnick J, Fisk D, Vegso S, et al. Family accommodation of obsessivecompulsive symptoms: Instrument development and assessment of family behavior. Journal of Nervous & Mental Disease. 1999;187:636–642. doi: 10.1097/00005053-199910000-00008. [DOI] [PubMed] [Google Scholar]
- Freeman JB, Garcia AM, Coyne L, Ale C, Przeworski A, Himle M, et al. Early childhood OCD: Preliminary findings from a family-based cognitive-behavioral approach. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:593–602. doi: 10.1097/CHI.0b013e31816765f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS, Foa EB. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1024–1033. doi: 10.1016/j.jaac.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kingery JN, Drake KL, Grados MA. Predictors of treatment response in pediatric obsessive-compulsive disorder. Journal of the American Academy of Child& Adolescent Psychiatry. 2008;47:868–878. doi: 10.1097/CHI.0b013e3181799ebd. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM. Psychopathology and the family. New York: Elsevier Science; 2005. [Google Scholar]
- Insel T. Director's update. Mental health research: into the future. [May 9, 2006];2006 http:llwww.nimh.mh.gov/about/director/updates/2006/mentalhealth -research-into-the -fiiture.shtml.
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 3rd. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- NIMH. Clinical Global Impressions Scale. Psychopharmacology Bulletin. 1985;21:839–843. [Google Scholar]
- O'Leary EM, Barrett P, Fjermestad KW. Cognitive-behavioral family treatment for childhood obsessive-compulsive disorder: A 7-year follow-up study. Journal of Anxiety Disorders. 2009;23:973–978. doi: 10.1016/j.janxdis.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Pediatric OCD Treatment Study Team. Cognitive-behavioral therapy, sertraline, and their combination for children and adolescents with obsessive–compulsive disorder: The Pediatric OCD Treatment Study (POTS) randomized controlled trial. Journal of the American Medical Association. 2004;292:1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Chang S, Langley A, Sugar C, Piacentini J. Family Factors Predict Treatment Outcome for Pediatric Obsessive Compulsive Disorder. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of family accommodation of childhood obsessive compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2008a;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Roblek T, Langley A, Benazon N, Piacentini J. Parental responses to obsessive compulsive disorder: development and validation of the parental attitudes and behaviors scale (PABS) Child and Family Behavior Therapy. 2008b;30:199–214. [Google Scholar]
- Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood J, McCracken J. Controlled Comparison of Family Cognitive Behavioral Therapy and Psychoeducation/Relaxation-Training for Child OCD. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:1149–1161. doi: 10.1016/j.jaac.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Langley A, Roblek T. Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm. New York, NY: Oxford University Press; 2007. [Google Scholar]
- Scahill L, Riddle MA, McSwiggan-Hardin MT, Ort SI, King RA, Goodman WK, et al. Children's Yale–Brown Obsessive Compulsive Scale: Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Silverman W, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Parent Version. San Antonio, TX: Graywing; 1996. [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology. 2009;77:474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Murphy TK, Geffken GR, et al. Psychometric evaluation of the Children's Yale-Brown Obsessive Compulsive Scale. Psychiatry Research. 2004;129:91–98. doi: 10.1016/j.psychres.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ. Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child & Adolescent Psychology. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Storch EA, Bjorgvinsson T, Riemann B, Lewin AB, Morales MJ, Murphy TK. Factors associated with poor response in cognitive behavioral therapy for pediatric obsessive compulsive disorder. Bulletin of the Menninger Clinic. 2010;74:167–185. doi: 10.1521/bumc.2010.74.2.167. [DOI] [PubMed] [Google Scholar]
- Waters TL, Barrett PM, March J. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: Preliminary findings. American Journal of Psychotherapy. 2001;55:372–387. doi: 10.1176/appi.psychotherapy.2001.55.3.372. [DOI] [PubMed] [Google Scholar]