Abstract
Objective
Examine the relationship between frailty and falls.
Methods
A total of 847 Mexican-Americans from the Hispanic Established Population for the Epidemiological Study of the Elderly were evaluated. The outcome variable was fall occurrence. Some predictor variables included were frailty, sociodemographic variables, functional and health status and prior falls.
Results
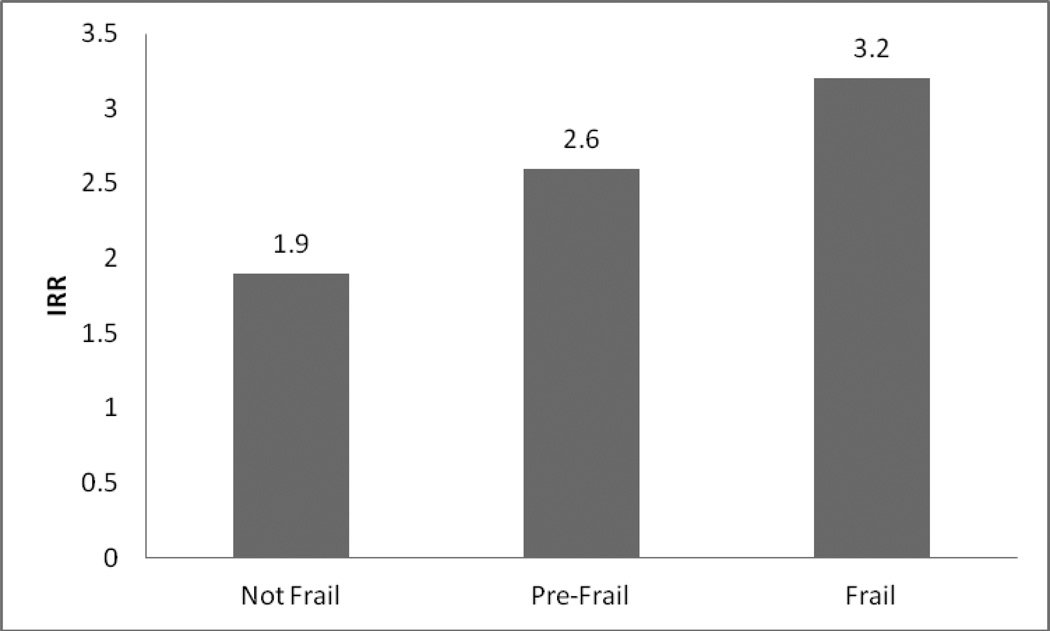
Those who fell were more likely to be women, not married, had prior falls, more functional problems and poorer health. The incidence-rate-ratio (IRR) for falls was 1.9 for non-frail individuals and 3.2 for frail individuals. Pre-frail individuals had 1.36 higher-odds of falls (95% CI 1.11–1.67), individuals with prior falls had 1.26 higher-odds of falls (95% CI 1.15–1.37), and those with poor balance had 1.49 higher-odds of falls (95% CI 1.15–1.95) over the two years (p<0.01).
Discussion
Frailty increases the odds of falls in older Mexican-Americans. Interventions tailored to reduce fall incidence and improve health-care quality for older Mexican-Americans are needed.
Keywords: older Mexican Americans, frail elderly, accidental falls
INTRODUCTION
Despite the lack of consensus on its definition, frailty is an important research topic and clinical concept in aging (Abellan, Rolland, Morley, & Vellas, 2008; Bergman, Hogan, & Karunananthan, 2008). There are several validated ways of measuring frailty and different authors have proposed indices in an attempt to operationalize the concept and facilitate detection of frailty for research and intervention purposes (Fried LP et al., 2001; Rockwood et al., 1999).
The frailty measure proposed by Fried and colleagues, using data from the Cardiovascular Health Study, has been widely used and validated in different populations (Espinoza & Hazuda, 2008; Fried LP et al., 2001; Ottenbacher KJ et al., 2005). Studies using this index have shown that it is associated with multiple adverse outcomes including falls, hospitalization, nursing home placement, disability and death (Abellan et al., 2008; Al Snih et al., 2009; Ensrud et al., 2007; Fried LP et al., 2001).
Frailty is a dynamic process where different conditions interact to produce various levels or stages of frailty (Gill, Gahbauer, Allore, & Han, 2006; Ottenbacher et al., 2009). In a recent review, Nowak and Hubbard conceptualize the frail older person as a complex system on the threshold of collapse (Nowak & Hubbard, 2009). In this framework, falls also result from a complex system failure.
Researchers have shown that both frailty and falls are related yet distinct syndromes. Both frailty and falls share risk factors and both result in common adverse events. Additionally, frailty and falls share pathophysiologic mechanisms (Inouye, Studenski, Tinetti, & Kuchel, 2007). They are also considered geriatric syndromes and as geriatric syndromes they are “multifactorial health conditions that occur when the accumulated effects of impairments in multiple systems render [an older] person vulnerable to situational changes.”( Tinetti, Inouye, Gill, & Doucette, 1995) Several of the risk factors that have been identified for falls (older age, functional impairment, low activity level, musculoskeletal alterations and undernutrition) are part of the cycle of frailty proposed by Fried and colleagues (Fried LP et al., 2001; Inouye et al., 2007; Shumway-Cook et al., 2009; Tinetti & Kumar, 2010). Identification of pathways that lead from frailty to falls as well as from falls to frailty are therefore important to advance aging research.
To our knowledge there are no studies that address the relationship between frailty and falls in the older Mexican Americans. The purpose of this study is to analyze the relationship between frailty and falls in a well defined sample of older Mexican Americans. We hypothesize that risk factors for falls will differ from commonly accepted risk factors for other populations. We also hypothesize that being non-frail, pre-frail or frail imposes a different risk profile for falls among this population.
METHODS
Sample and procedures
Data were from the Hispanic Established Population for the Epidemiological Study of the Elderly (H-EPESE), a longitudinal study of Mexican Americans aged 65 and over, residing in five Southwestern states in the US. The sample and its characteristics are described elsewhere (Markides KS, Stroup-Benham CA, &, 1999). The sampling procedure assured a sample that could be generalized to approximately 500,000 older community dwelling Mexican Americans living in the Southwest at baseline. In the first wave of the Hispanic EPESE (1993–1994), 3,050 participants were interviewed. Participants were followed approximately every two years for 14 years. After waves 5 and 6, data to assess frailty were collected to examine the relationship of disability and frailty in this group of older adults. A sample of 1013 older Mexican Americans were selected from wave 5 of the Hispanic EPESE and re-interviewed in 2006 using a comprehensive battery of physical function tests. All components necessary to compute Fried’s frailty index were included as part of the evaluation (see description below). The same individuals were re-evaluated in 2009.
For our study we selected participants from the second and third interviews that had complete information on frailty and falls. Of the initial 1,013 subjects, 102 died before follow-up interview, and 64 did not have complete information on falls or one of the components of the frailty index. Thus, the final sample consisted of 847 participants who had complete information on the measures described below.
Measures
Frailty
Frailty was assessed according to criteria developed by Fried and colleagues(Fried LP et al., 2001). Their frailty index ranged from 0 to 5 and included weight loss, exhaustion, walking speed, grip strength, and physical activity (Fried LP et al., 2001). The original frailty index used the short version of the Minnesota Leisure Time Activity questionnaire to determine physical activity level (Fried LP et al., 2001). We used the Physical Activity Scale for the Elderly (PASE) (Washburn RA, Smith KW, Jette AM, & Janney CA, 1993). Participants who scored in the lowest quintile of PASE, adjusted by gender, were categorized as positive for low physical activity criterion (score=1). The other components of the frailty index were used following the criteria established by Fried at al. and validated in this population group(Fried LP et al., 2001; Ottenbacher KJ et al., 2005). Each component of the fraily index was scored as 0 or 1 resulting in a summary score of 0 to 5. The specific criteria for scoring each of the frailty components are described elsewhere (Ottenbacher KJ et al., 2005).
Participants who scored 0 on the summary frailty index were categorized as not-frail. Participants scoring 1 or 2 were considered pre-frail, and those scoring 3 or greater were categorized as frail. The original index has been widely used in the aging research literature. The modified version of the index using the PASE was validated for Mexican American older adults in previous research(Ottenbacher KJ et al., 2005; Ottenbacher et al., 2009).
Falls
Prevalence of falls at baseline (2006) and follow-up (2009) interviews was assessed using the following question: “During the last 12 months, how many times did you fall and land on the floor or ground?” Fall status was dichotomized as having no falls versus having one or more falls.
Covariates
Sociodemographic variables included were age (continuous), gender, marital status (dichotomous) and years of formal education (continuous). To assess health status, medical conditions previously reported to increased risk of falls in older Mexican Americans were included. Participants were asked if they had ever been told by a doctor that they had: diabetes, arthritis, hypertension, heart attack, stroke, or urinary incontinence. Answers were dichotomized as either yes or no. Visual problems were assessed by asking individuals: “Can you see well enough to recognize a friend or a family member who is at an arm’s length away?” Urinary incontinence was evaluated with the question: “In the past month, how often have you had difficulty holding your urine until you could get to the toilet?” Answers were coded in five categories: never, hardly ever, some of the time, most of the time, or all of the time. Answers different from “never” were considered urinary incontinence.
Body mass index (BMI) was computed as weight in kilograms divided by height in meters squared. Anthropometric measurements were collected in the home using the methods and instructions similar to those employed in other EPESE studies. Height was measured using a tape placed against the wall and weight was established using a Metro 9800 scale.
Cognitive status was evaluated with the Mini Mental State Exam (MMSE), both English and Spanish versions (Folstein MF, Folstein SE, & McHugh PR, 1975). The total score ranges from 0–30 where higher scores indicate better cognitive function; the total score was used as a continuous variable. Depressive symptoms were measured using the Center for Epidemiological Study-Depression (CES-D) scale (Radloff LS, 1977). The total score ranges from 0–60 with higher scores indicating more depressive symptoms. The total score was used as a continuous variable.
Physical functioning was ascertained with activities of daily living (ADL) and instrumental activities of daily living (IADL). Respondents were asked if they needed help doing seven ADL tasks: walking across a small room, bathing, grooming, dressing, eating, transferring from bed to chair, and toileting. Respondents who indicated they needed help or were unable to do any ADL were coded as 1 for ADL disability, those with no difficulty were coded as 0 for ADL disability. For the IADL items, respondents were asked if they were able to do 10 activities: using a telephone, driving, shopping, preparing meals, performing light housework, taking medications, handling money, doing heavy housework, walking up and down stairs, and walking half a mile. Respondents able to perform all IADLs were coded as 0 for IADL disability and those with difficulties in any IADL were coded as 1 for IADL disability. Use of a walking aid was also considered. Participants were asked if they used a walking aid, answers were dichotomized as yes or no.
We also examined balance with the standing balance component of the Short Physical Performance Battery (SPPB) (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). Using previously established criteria, performance on standing balance was classified on a scale ranging from 0–4. Participants unable to perform the task were given a score of 0; all other participants were given a score between 1 and 4 depending on their performance.
Statistical analysis
To determine if there were differences in prevalence of falls by frailty status, incident rate ratios (IRR) were initially calculated. The sample was divided between those with falls and those without falls and incident risk as well as rate of falls and no falls was used to calculate IRR. Then, all covariates were compared by fall status. To identify predictors of falls in this population between baseline and follow-up, zero-inflated Poisson regression models were created due to the distribution of the dependent variable, where a significant percentage of individuals reported no falls. Variables included in the Poisson models were age, gender, frailty status, arthritis, urinary incontinence, vision, depression, disability, use of walking aid, previous falls, BMI, cognitive function and balance. All of these variables have been reported to be related to higher risk of falls among older Mexican Americans. All analyses were performed using the SAS system for windows, version 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
Figure 1 shows the unadjusted IRR of falls by frailty categories. Non-frail individuals presented the lowest rates of falls (IRR 1.9), followed by pre-frail individuals (IRR 2.6) and finally frail individuals (IRR 3.2) with the highest rates.
Figure 1.
Incident rate ratio of falls at follow-up by frailty status.
Table 1 shows the characteristics of the sample by fall status at baseline (2006). In the group that fell, the percentage of pre-frail and frail individuals was higher compared to the group that didn’t fall (52.0% vs. 46.6% for pre-frail and 14.5% vs. 10.6% for frail respectively). Individuals that fell were older (82.2 years), more likely to be women (70.4%), had lower education (4.8 years), were less likely to be married (36.0%), had higher rates of depressive symptoms (21.9%) and lower cognitive function (20.9 in mean total MMSE). They also had higher prevalence of disability (as seen with the ADls and IADLs), had higher prevalence of medical conditions overall, more reported using a walking aid and people who fell had problems with balance compared to those that didn’t fall.
Table 1.
Characteristics of the sample at baseline by fall status at follow-up (n=847)
| Covariates | Falls (n=392) | No Falls (n=455) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age, mean (±SD) | 82.2 (±4.5) | 81.9 (±4.3) | |||
| Education, mean (±SD) | 4.8 (±3.9) | 5.2 (±3.8) | |||
| Gender (women) | 276 | 70.4 | 272 | 59.8 | |
| Marital Status (married) | 141 | 36.0 | 209 | 45.9 | |
| Diabetes | 149 | 38.0 | 137 | 30.1 | |
| Arthritis | 258 | 66.2 | 269 | 59.5 | |
| Hypertension | 186 | 54.9 | 218 | 55.1 | |
| Heart Attack | 12 | 3.1 | 13 | 2.9 | |
| Stroke | 20 | 5.1 | 23 | 5.1 | |
| Urinary Incontinence | 181 | 46.3 | 163 | 35.8 | |
| Near Vision | 14 | 3.6 | 7 | 1.5 | |
| Depressive Symptoms | 86 | 21.9 | 58 | 12.8 | |
| ADL disability | 147 | 37.5 | 146 | 32.1 | |
| IADL disability | 314 | 80.1 | 317 | 69.7 | |
| Uses Walking Aid | 48 | 14.0 | 52 | 12.9 | |
| MMSE total, mean(±SD) | 20.9 (±4.4) | 21.4 (±4.5) | |||
| Balance (From SPPB) | |||||
| 0 (Unable) | 88 | 22.6 | 91 | 20.1 | |
| 1 | 56 | 14.4 | 29 | 6.4 | |
| 2 | 64 | 16.4 | 60 | 13.3 | |
| 3 | 41 | 10.5 | 57 | 12.6 | |
| 4 | 141 | 36.2 | 216 | 47.7 | |
| Frailty Index | |||||
| Not Frail | 131 | 33.4 | 195 | 42.9 | |
| Pre-frail | 204 | 52.0 | 212 | 46.6 | |
| Frail | 57 | 14.5 | 48 | 10.6 | |
SD= Standard Deviation; ADL = Activities of Daily Living; IADL = Instrumental Activities of Daily Living; MMSE = Mini Mental State Exam; SPPB = Short Physical Performance Battery
Table 2 shows the Poisson regression model analyzing predictors of falls at follow-up. Individuals considered pre-frail, those with history of previous falls and those with poor balance, had significantly increased likelihood of falls at follow-up (p<.01). The odds of falling for pre-frail individuals were 1.36 higher compared to non-frail (95% CI 1.11–1.67), for those with a history of falls the odds were 1.26 higher (95% CI 1.15–1.37) and for those with poor balance the odds were 1.50 higher (95% CI 1.15–1.95) compared to those with good balance. Individuals with arthritis had 1.22 higher odds of falling (95% CI 1.00–1.49), however, the odds were not statistically significant (p=.05). Having a better MMSE score was a protective factor against falls (OR 0.98) however it was not statistically significant (p=.05). None of the other covariates significantly affected the likelihood of falling at follow-up.
Table 2.
Poisson regressions predicting likelihood of falls between baseline and follow-up (n=847)
| Parameter | Estimate (β) | SE | p-value |
|---|---|---|---|
| Age (years) | 0.01 | 0.01 | 0.42 |
| Gender (male) | −0.16 | 0.11 | 0.13 |
| Arthritis | 0.20 | 0.10 | 0.05 |
| Urinary Incontinence | 0.09 | 0.09 | 0.37 |
| Near Vision | 0.37 | 0.26 | 0.16 |
| Depressive Symptoms | 0.00 | 0.13 | 0.99 |
| ADL disability | 0.10 | 0.11 | 0.39 |
| IADL disability | −0.02 | 0.13 | 0.91 |
| Uses walking aid | −0.28 | 0.17 | 0.09 |
| Frailty Index | |||
| Not Frail | 1.00 | 1.00 | 1.00 |
| Pre Frail | 0.31 | 0.11 | 0.003 |
| Frail | 0.32 | 0.17 | 0.06 |
| History of Falls | 0.23 | 0.04 | <.0001 |
| BMI | 0.01 | 0.01 | 0.33 |
| MMSE | −0.02 | 0.01 | 0.05 |
| Balance (From SPPB) | |||
| 0 | 0.30 | 0.18 | 0.09 |
| 1 | 0.40 | 0.14 | 0.003 |
| 2 | 0.19 | 0.13 | 0.16 |
| 3 | 0.17 | 0.15 | 0.26 |
| 4 | 1.00 | 1.00 | 1.00 |
SE = Standard Error; ADL = Activities of Daily Living; IADL = Instrumental Activities of Daily Living; BMI = Body mass index; MMSE = Mini Mental State Exam; SPPB = Short Physical Performance Battery
DISCUSSION
In this study the risk of falling is lowest for those individuals deemed not frail, followed by those labeled pre-frail and then those identified as frail. Individuals that fell during the two-year period are more likely to be women, are older, have less education, have higher prevalence of diseases, higher prevalence of disability and are likely to be frail. Statistically significant predictors of falls for this sample are pre-frail status, prior history of falls, and poor balance.
Forty percent of our sample reported having falls at follow-up. Previous studies on Mexican American populations have reported lower rates of falls (Reyes-Ortiz, Al Snih, Loera, Ray, & Markides, 2004; Schwartz et al., 1999). The rates we report are also higher compared to other Hispanic populations (Reyes-Ortiz, Al Snih, & Markides, 2005). These differences are probably related to the unique characteristics of the Mexican American population that have been previously reported (Markides & Eschbach, 2005).
A recent publication reports that the five strongest risk factors for falls in older adults are: previous falls, muscle weakness, gait alterations, balance problems and polypharmacy (Tinetti & Kumar, 2010). Previous falls and balance problems are significant predictors of falls in our study. Muscle weakness and gait alterations are part of the frailty index we used and being pre-frail is also a risk factor for falls in our study. However, unlike other population groups, commonly accepted risk factors for falls such as female gender, age, visual impairment and disability(Shumway-Cook et al., 2009; Tinetti, 2003), among others, were not significant in our multivariable analysis.
Several authors suggest that older Mexican Americans are a unique population with a special morbidity and mortality profile (Markides & Eschbach, 2005). Other authors show that in addition to this profile, older Mexican Americans have high rates of disability (Al Snih et al., 2009; Ottenbacher et al., 2009; Peek, Ottenbacher, Markides, & Ostir, 2003). Another alternative is that the disability rates observed at baseline among those who fell, along with the high prevalence of medical conditions and lower quality of health care, contribute to the different fall risk profile observed in our sample.
Our study demonstrated that pre-frail individuals have higher risk of falls. One possibility is that despite alterations that place them in the pre-frail category, they are still independent and more mobile than frail individuals putting them at higher risk for falling. Researchers have shown that pre-frail individuals are less likely to be disabled and have fewer comorbidities compared to frail individuals(Gill et al., 2006; Ottenbacher et al., 2009), making them more mobile and more likely to engage in activities where falls can occur. Another option is that frail individuals, because of their underlying medical condition and how family members and healthcare providers perceive their health, may have more social support compared to pre-frail individuals. Data supports that higher social support is related to fewer falls (LaPlante, Kaye, Kang, & Harrington, 2004; Peel, McClure, & Hendrikz, 2007). Additionally, social support has been proposed as one of the factors contributing to health advantages in older Mexican Americans (Markides & Coreil, 1986).
In this study, more than 65% of older Mexican Americans reported IADL disability and more than 30% reported ADL disability regardless of their fall status (Table 1). These numbers are higher than previously reported in other ethnic groups (Dunlop, Song, Manheim, Daviglus, & Chang, 2007). High disability rates increase the risk of falls (Reyes-Ortiz et al., 2005; Shumway-Cook et al., 2009). Similarly, more than 30% of our sample reported having diabetes, more than 55% reported having arthritis, greater than 50% reported having hypertension and more than 35% reported having urinary incontinence. These large percentages suggest that our sample has poor health. Poor health is also an important predictor of falls (Tinetti et al., 1995). Finally, it is reported that Mexican Americans have lower quality of healthcare compared to other populations (Higashi et al., 2005).
Falls are proposed as a quality of care indicator for older adults (Higashi et al., 2005). In our study a history of falls is a significant predictor of falls. A history of falls, in addition to high prevalence of medical conditions suggests that quality of care is poor for our group and provides a plausible explanation for some of our findings.
Strengths of our study include a well-defined and thoroughly analyzed cohort of older Mexican Americans. We used a widely accepted and objective measure of frailty and included several valid and reliable assessments of disability, functional status, and emotional health (e.g., depressive symptoms) that have been used in previous EPESE studies. However, our study has some limitations. First, we only have two data points, limiting our ability to analyze trends in falls. Also, our short follow-up reduces our ability to analyze the effect of different factors on falls over time. Finally, our sample size limits the power of some of our sub-analyses. Also, given the dynamic nature of frailty, where individuals move between frailty categories, we might not be identifying individuals that recover or get worse due to the single follow-up period.
In conclusion, frailty, and more precisely pre-frailty are significant predictors of falls in older Mexican Americans. Factors related to quality of care and disability were also important predictors of falls in this sample. Given the catastrophic effects associated with falls in older adults, future studies need to build on these findings and develop interventions tailored to older Mexican Americans to help prevent falls and reduce disability and loss of independence in this population.
Supplementary Material
Reference List
- Abellan VK, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J.Nutr.Health Aging. 2008;12:29–37. doi: 10.1007/BF02982161. [DOI] [PubMed] [Google Scholar]
- Abellan VK, Rolland YM, Morley JE, Vellas B. Frailty: toward a clinical definition. J.Am.Med.Dir.Assoc. 2008;9:71–72. doi: 10.1016/j.jamda.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Al Snih S, Graham JE, Ray LA, Samper-Ternent R, Markides KS, Ottenbacher KJ. Frailty and incidence of activities of daily living disability among older Mexican Americans. J Rehabil.Med. 2009;41:892–897. doi: 10.2340/16501977-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman H, Hogan DB, Karunananthan S. Frailty: A clinically relevant concept? The Canadian Journal of Geriatrics. 2008;11:124–129. [Google Scholar]
- Dunlop DD, Song J, Manheim LM, Daviglus ML, Chang RW. Racial/ethnic differences in the development of disability among older adults. American Journal of Public Health. 2007;97:2209–2215. doi: 10.2105/AJPH.2006.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J.Gerontol.A Biol.Sci.Med.Sci. 2007;62:744–751. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- Espinoza SE, Hazuda HP. Frailty in older Mexican-American and European-American adults: is there an ethnic disparity? Journal of the American Geriatrics Society. 2008;56:1744–1749. doi: 10.1111/j.1532-5415.2008.01845.x. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. "Mini-Mental State" A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fried LP, Tangen CM, Walston JD, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J.Gerontol.A Biol.Sci.Med.Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Archives of Internal Medicine. 2006;166:418–423. doi: 10.1001/archinte.166.4.418. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England Journal of Medicine. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higashi T, Shekelle PG, Adams JL, Kamberg CJ, Roth CP, Solomon DH, et al. Quality of care is associated with survival in vulnerable older patients. Ann.Intern.Med. 2005;143:274–281. doi: 10.7326/0003-4819-143-4-200508160-00008. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. Journal of the American Geriatrics Society. 2007;55:780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaPlante MP, Kaye HS, Kang T, Harrington C. Unmet need for personal assistance services: estimating the shortfall in hours of help and adverse consequences. J.Gerontol B Psychol.Sci.Soc.Sci. 2004;59:S98–S108. doi: 10.1093/geronb/59.2.s98. [DOI] [PubMed] [Google Scholar]
- Markides KS, Stroup-Benham CA, B S. The health of Mexican-American elderly: selected findings from the Hispanic EPESE. New York: Springer; 1999. [Google Scholar]
- Markides KS, Coreil J. The Health of Hispanics in the Southwestern United-States - An Epidemiologic Paradox. Public Health Reports. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(Spec No 2):68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Nowak A, Hubbard RE. Falls and frailty: lessons from complex systems. Journal of the Royal Society of Medicine. 2009;102:98–102. doi: 10.1258/jrsm.2009.080274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher KJ, Ostir GV, Peek MK, Al Snih S, Raji MA, Markides KS. Frailty in older mexican americans. Journal of the American Geriatrics Society. 2005;53:1524–1531. doi: 10.1111/j.1532-5415.2005.53511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher KJ, Graham JE, Al Snih S, Raji M, Samper-Ternent R, Ostir GV, et al. Mexican Americans and frailty: findings from the Hispanic established populations epidemiologic studies of the elderly. American Journal of Public Health. 2009;99:673–679. doi: 10.2105/AJPH.2008.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek MK, Ottenbacher KJ, Markides KS, Ostir GV. Examining the disablement process among older Mexican American adults. Social Science and Medicine. 2003;57:413–425. doi: 10.1016/s0277-9536(02)00367-2. [DOI] [PubMed] [Google Scholar]
- Peel NM, McClure RJ, Hendrikz JK. Psychosocial factors associated with fall-related hip fractures. Age and Ageing. 2007;36:145–151. doi: 10.1093/ageing/afl167. [DOI] [PubMed] [Google Scholar]
- Radloff LS. 'The CES-D scale: A self report depression scale for research in the general population'. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reyes-Ortiz CA, Al Snih S, Loera J, Ray LA, Markides KS. Risk Factors For Falling in Older Mexican Americans. Ethnicity and Disease. 2004;14:417–422. [PubMed] [Google Scholar]
- Reyes-Ortiz CA, Al Snih S, Markides KS. Falls among elderly persons in Latin America and the Caribbean and among elderly Mexican-Americans. Revista Panamericana de Salud Publica. 2005;17:362–369. doi: 10.1590/s1020-49892005000500008. [DOI] [PubMed] [Google Scholar]
- Rockwood K, Stadnyk K, MacKnight C, McDowell I, Hebert R, Hogan DB. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353:205–206. doi: 10.1016/S0140-6736(98)04402-X. [DOI] [PubMed] [Google Scholar]
- Schwartz AV, Villa ML, Prill M, Kelsey JA, Galinus JA, Delay RR, et al. Falls in older Mexican-American women. Journal of the American Geriatrics Society. 1999;47:1371–1378. [PubMed] [Google Scholar]
- Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Physical Therapy. 2009;89:324–332. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME. Clinical practice. Preventing falls in elderly persons. New England Journal of Medicine. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- Tinetti ME, Kumar C. The patient who falls: "It's always a trade-off". JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.