Figure 1. Algorithm for the evaluation and treatment of MDS after allogeneic hematopoietic stem cell transplantation.
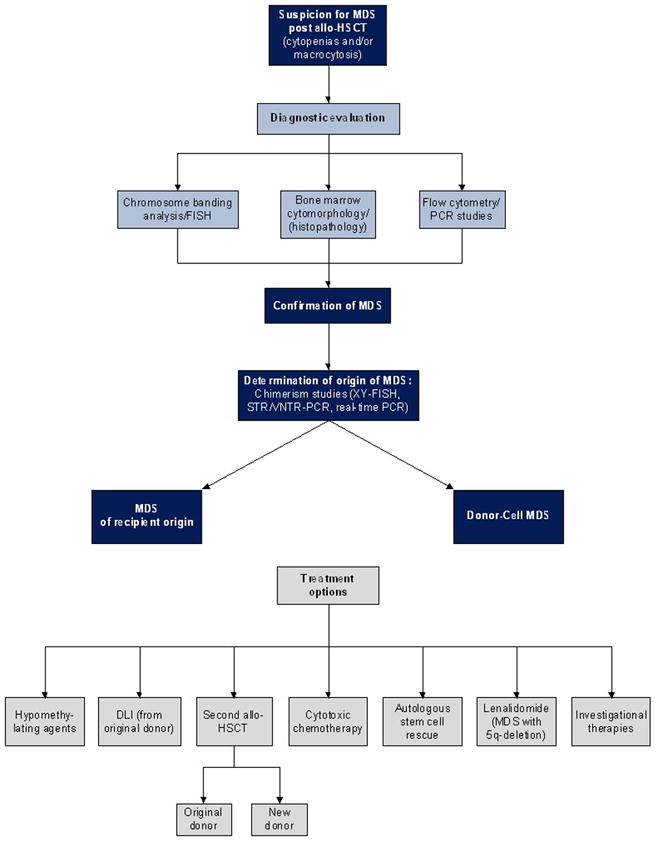
This algorithm provides general guidelines for the evaluation and treatment of MDS after allogeneic hematopoietic stem cell transplantation.
MDS should be considered in the differential diagnosis of persistent cytopenias and/or macrocytosis that are not otherwise explained by medication effect or post-transplant complications. Diagnostic bone marrow aspirate and biopsy should be performed for morphologic evaluation and extra aspirate samples collected for possible additional studies as detailed below. If dysplasia, atypia and/or increased blasts are detected, samples should be sent for cytogenetic evaluation by means of chromosome banding analysis and/or FISH, flow cytometry, PCR studies specific to previously documented molecular markers of the underlying disease, and/or chimerism analysis. The origin of the MDS as either recipient- or donor- derived should be determined. In patients previously transplanted for AML/MDS, relapse is more likely than de novo donor-cell MDS. In patients transplanted for other conditions, donor-cell MDS is most likely. Methods for determining the origin of MDS include STR/VNTR PCR, real-time PCR, and XY-FISH (in sex mismatched transplants). Treatment options for MDS after alloHSCT include hypomethylating agents, DLI, second alloHSCT (from the original or a new donor), cytotoxic chemotherapy, high-dose therapy with autologous stem cell rescue, and lenalidomide (for those with 5q-deletion). Enrollment in clinical trials should be considered. The decision regarding the best treatment for an individual patient is dependent upon the origin of the MDS (recipient versus donor), the rapidity of disease progression to AML, cytogenetic abnormalities, and co-morbidities. Treatment options should be weighed carefully and individualized with close considerations of such factors. Specifically, the origin of MDS plays an important role in determining the best therapy. For example, DLI may be a reasonable first choice to manage relapsed MDS of recipient origin, whereas a therapeutic GVL effect would not be expected in donor-derived MDS and thus an alternative treatment would be preferred in that setting. Although some treatment options have curative potential (e.g., second alloHSCT), these may be associated with high risk of treatment-related mortality. In contrast, other approaches are less likely to be curative, however, they may offer reduced toxicity and higher likelihood of improved short-term quality of life.
