Abstract
Purpose: To determine if embryo cleavage state or morphology on day 3 correlates with implantation or live birth rates. A retrospective cohort study of all fresh embryo transfers over 2 years.
Methods: Patients were grouped by the average cleavage state and morphology. Cleavage state groups were: <6, ≥6, <8, and ≥8 cells. Morphology groups by average grade were: group 1 (best) = 1, group 2 = >1≤2, group 3 = >2≤3, and group 4 (worst) = >3≤4.
Results: The overall implantation rate for 158 cycles was 28.1% with a live birth rate of 37.3%. Morphologic state was highly predictive of both implantation rate and live birth rate. Implantation rates by group were 54.8% (group 1), 30.4% (group 2), 23.8% (group 3), and 11.1% (group 4). Likewise, live birth rates among groups were 61.5, 39, 20, and 21%, respectively. Cleavage state was not predictive of outcome.
Conclusions: Embryo grade is highly predictive of implantation and live birth rate and can be used to determine the number of embryos to transfer. Cleavage state is not predictive of outcome.
KEY WORDS: Cleavage-state embryo, embryo morphology, in vitro fertilization, pregnancy outcome.
INTRODUCTION
The first child was conceived by in vitro fertilization (IVF), in the United States, in 1983. Since that time, the success of IVF has steadily increased. In 2002, 45,751 children (0.8% of all live births) were born as a result of IVF (1). However, the increased probability of IVF pregnancy has come at a cost as multiple gestation is seen in approximately 35% of all IVF-related births (2), resulting in a 65% increase over baseline for twins and more than a 400% increase in higher order multiple births in the United States (1). This highly significant increase in multiple gestations is associated with escalating maternal and fetal morbidity and mortality. Therefore, efforts need to be made to decrease this IVF outcome. One solution for decreasing higher order multiple gestations from IVF would be to transfer only one embryo. However, the overall success of IVF is strongly correlated to the number of embryos transferred and the demand for successful outcomes is high because the treatment is expensive and stressful. Therefore, fertility specialists and embryologists continue to search for methods to predict which embryos have the greatest potential for implantation.
The purpose of this study was to evaluate the relationship of embryo morphology and cleavage state on live pregnancy rates after fresh embryo transfer. We hypothesized that cleavage state and/or embryo morphologic grade would be predictive of implantation and live birth rate. In addition, we desired to establish a predictive score for live birth rate based on the morphology and/or cleavage state of the embryo(s) being transferred to assist in counseling patients regarding the number of embryos to transfer and the probability of pregnancy. By improving the prediction of implantation and live birth rate, the least number of quality embryos can be transferred to maintain high pregnancy rates.
METHODS
All in vitro fertilization cycles that included a fresh embryo transfer on postretrieval day 3 at the Center for Reproductive Health in Cincinnati, Ohio between January 2002 and December 2003 were reviewed. Demographic information including age, gravidity, parity, infertility diagnosis, and number of previous IVF cycles were collected. IVF cycle information included the number of embryos transferred, cleavage state of each embryo transferred, morphologic grade of each embryo transferred, and the use of intracytoplasmic sperm injection (ICSI) and/or assisted hatching (AH). The number of embryos transferred was based on the patient's previous history and subjective embryo characteristics. Outcome measures included: 1) qualitative serum βhCG on day 14 after embryo transfer, 2) number of gestational sacs and fetal status (presence of fetal pole/cardiac activity) by ultrasound on day 28 after embryo transfer, and pregnancy outcome including spontaneous abortion and live birth. Implantation was defined as the presence of a gestational sac on ultrasound 28 days after transfer, and implantation rate was calculated by dividing the number of gestational sacs by the total number of embryos transferred. Live birth rate was calculated by dividing the number of liveborn deliveries by the total number of transfers.
Embryo Morphology
A single team of experienced embryologists evaluated the embryos on postretrieval day 3. Morphology of each embryo was determined by criteria as described by Veeck (3):
Grade I: blastomeres of equal size and no cytoplasmic fragments
Grade II: blastomeres of equal size with minor cytoplasmic fragments or blebs
Grade III: blastomeres of distinctly unequal size with few to no cytoplasmic fragments
Grade IV: blastomeres of equal or unequal size with significant cytoplasmic fragmentation
Grade V: few blastomeres of any size and severe or complete fragmentation
Patients were placed into one of four groups by mean morphology score. The morphology groups were Group 1 (best) = 1, Group 2 = >1≤2, Group 3 = >2≤3, and Group 4 (worst) = >3≤4.
The patients were also grouped by the average cleavage state. These cleavage groups were: group 1 < 6 cells, group 2 ≥6 cells and <8 cells, and group 3 ≥8 cells. Outcomes were analyzed by groups.
Statistics were analyzed using ANOVA for continuous variables and chi-square for proportional data. Correlation analysis was performed using Spearman's correlation.
RESULTS
Overview of All IVF–ET Cycles
A total of 158 fresh embryo cycles were included in this study. Subjects had a mean age of 34.6 years and 39% were parous. The mean number of previous IVF cycles was 1.5. On average, 2.77 embryos were transferred per IVF cycle for a total of 438 embryos replaced. ICSI was performed in 57% (n=90) of cycles, and AH was performed in 32% of cycles (n=50). The mean implantation rate was 28.1% and the mean live birth rate was 37.3%.
Demographics by Group Assignment
Analysis of the patient characteristics by both average morphology group (Table I) and average cleavage state revealed no significant difference in age, gravidity, parity, number of embryos transferred, infertility diagnosis, previous number of IVF cycles, use of ICSI, or use of AH.
Table I.
Subject Demographics by Their Assigned Morphologic Group
| Group 1 (n=30) | Group 2 (n=70) | Group 3 (n=41) | Group 4 (n=17) | p value | |
|---|---|---|---|---|---|
| Age (±SD) | 33.9 (6.1) | 35.4 (4.9) | 35.9 (3.0) | 33.5 (4.0) | ns |
| % Gravid | 38 | 61 | 65 | 64 | ns |
| % Parous | 15 | 41 | 45 | 45 | ns |
| Cycle number (±SD) | 1.5 (0.87) | 1.49 (0.75) | 1.95 (1.43) | 1.55 (0.52) | ns |
| Mean # embryos transferred (±SD) | 2.4 (0.87) | 2.7 (0.59) | 3.15 (1.35) | 2.45 (0.93) | ns |
| ICSI (%) | 67 | 58 | 55 | 82 | ns |
| Assisted hatching (%) | 33 | 46 | 55 | 27 | ns |
Outcomes by Cleavage State
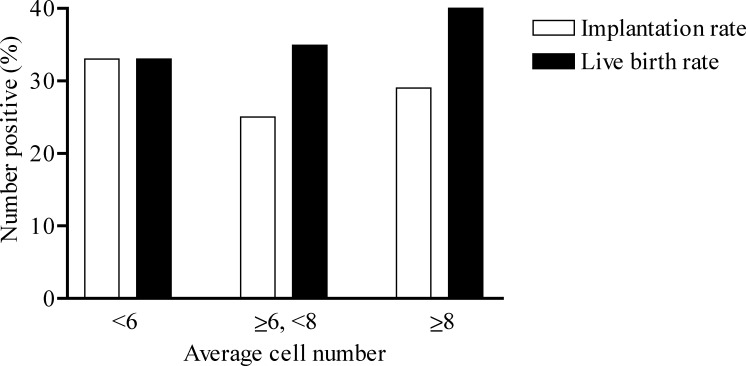
Cycles were sorted by average cleavage state and no significant difference in implantation rates or live birth rates was noted (Fig. 1). The live birth rates in these groups were 32, 35, and 40%, respectively.
Fig. 1.
Mean cleavage state is not associated with pregnancy outcome. There were no statistical differences in implantation rate or live birth rate when the cycles were sorted by the average cell number.
Outcomes by Morphology Group
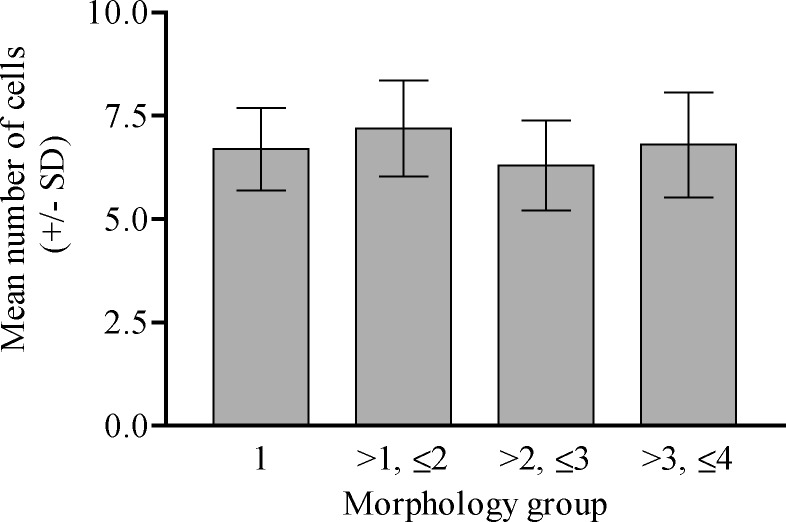
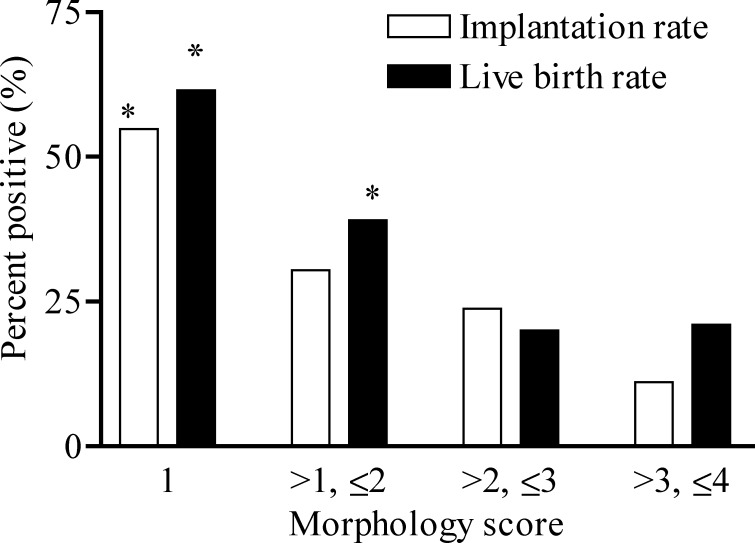
Cycles were sorted by morphology group, and no difference in average cleavage state existed between the four morphology groups (Fig. 2). When the average morphology groups were analyzed for implantation rate and live birth rate, a significant difference existed between the two highest quality morphology groups (groups I and II) and the two lowest quality groups (groups III and IV) for live birth rate (Fig. 3). The two higher morphology groups had significantly improved live birth rates of 61.5% (group 1) and 39% (group 2), compared to 20% (group 3) and 21% (group 4) in the lowest two morphology groups. In addition, the patients in morphology group 1 had a significantly increased rate of implantation compared to group 2 (54% vs. 30%) (Fig. 3).
Fig. 2.
Mean cleavage state did not differ by morphology group. The number of cells in the transferred embryos were examined in each morphologic group and found to be statistically the same.
Fig. 3.
Mean morphology score is predictive of implantation and live birth rates. A morphology score of 2 or less was statistically predictive of pregnancy (* denotes a p > 0.05 when compared to groups with a score greater than 2).
DISCUSSION
Recent guidelines published in September 2004 by the American Society for Reproductive Medicine (ASRM) recommend the number of embryos transferred to be limited to two or less embryos in women under 35 and only one embryo in women with the “best prognosis” (4). The most favorable prognosis is defined as a woman undergoing her first IVF cycle or with a previously successful IVF cycle, with good embryo quality, and with excess embryos available for cryopreservation. These recommendations are a reflection of the nationwide and worldwide awareness for the need to reduce the higher-order multiple pregnancy rate from IVF. By limiting the quantity of embryos transferred per cycle, the quality of the embryo becomes of paramount importance.
A general consensus exists that better quality embryos lead to improved pregnancy rates. Many investigators have tried to delineate the properties of an embryo that make it more likely to lead to a successful pregnancy. Properties that have been investigated include cleavage state, fragmentation, cytoplasmic pitting, compaction, and equality of cell size. Cleavage state is likely an important characteristic of an embryo because data suggest that embryos with either lagging or rapid cleavage have high rates of chromosomal abnormalities and decreased rates of implantation (5). Morphology, based on fragmentation and blastomere size, is also an important property of embryo development because embryo fragmentation is theorized to occur as a result of apoptosis with subsequent loss of regulatory proteins (6). The loss of these regulatory proteins may ultimately affect the developmental competency of the embryo and its ability to implant. Significantly higher rates of congenital malformations have been described in pregnancies derived from highly fragmented embryos (5).
The criteria for choosing optimal embryos remain controversial. Several investigators suggest that cleavage state is a superior predictor for embryo implantation (7–9) and that embryo morphology analysis adds little to prediction of implantation. These studies conclude that cell number should always be used when selecting embryos; however, a “good prognosis” patient generally has multiple embryos in the six- to eight-cell stage on postretrieval day 3 limiting the predictive value of the cell number alone. Morphology may be a better indicator for success in patients with appropriately growing embryos. However, the selection of the morphologically best embryos by experienced embryologists on day 3 has only a 23% predictive value for day 5 blastocyst formation in vitro, suggesting to some investigators that day 3 morphology may be an inaccurate predictor of an embryo's implantation capability (10,11). However, other studies also have shown that moderately fragmented embryos (grade II) implant with similar rates to higher quality (grade I) embryos, but highly fragmented embryos (grade III and grade IV) have significantly decreased implantation rates (8). Because of these discrepancies, several authors promote using a “combined” or “cumulative” embryo score based on combined cleavage states and morphologies of all embryos being transferred (12–15). Unfortunately, these combined or generalized transfer scores can underestimate the potential of a single higher quality embryo to implant.
In this study, the average morphologic grade of the embryos on postconception day 3 was highly predictive of implantation rate and live birth rate. The embryo cell number on postconception day 3 was greater than six in the majority of transfers and, therefore, was not predictive of pregnancy outcome. This is the first study to demonstrate the superior predictive value of embryo morphology over blastomere number (cleavage state) for the outcome of live birth within a cohort of women undergoing IVF.
REFERENCES
- 1.Martin J, et al. Natl Vital Stat Rep. December 2003;52:16. [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2002 Assisted Reproductive Technology Report Success. National Summary and Fertility Clinic Reports, December 2004
- 3.Veeck L: An Atlas of Human Gametes and Conceptuses. An Illustrated Reference for Assisted Reproductive Technology, 1999
- 4.Practice Committee, Society for Assisted Reproductive Technology and the American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril 2004 Sep;82(3):773–774. [DOI] [PubMed]
- 5.Ebner T, Yaman C, Moser M, Sommergruber M, Polz W. Tews G: Embryo fragmentation in vitro and its impact on treatment and pregnancy outcome. Fertil Steril. 2001;76:281–285. doi: 10.1016/S0015-0282(01)01904-5. [DOI] [PubMed] [Google Scholar]
- 6.Alikani M, Cohen J, Tomkin G, Garrisi J, Mack C, Scott R. Human embryo fragmentation in vitro and its implication for pregnancy implantation. Fertil Steril. 1999;71:836–842. doi: 10.1016/S0015-0282(99)00092-8. [DOI] [PubMed] [Google Scholar]
- 7.Hsu M, Mayer J, Aronshon M, Lanzendorf S, Muasher S, Kolm P, et al. Embryo implantation in in vitro fertilization and intracytoplasmic sperm injection: Impact of cleavage status, morphology grade, and number of embryos transferred. Fertil Steril. 1999;72:679–685. doi: 10.1016/S0015-0282(99)00320-9. [DOI] [PubMed] [Google Scholar]
- 8.Ziebe S, Petersen K, Lindenberg S, Anderson AG, Gabrielsen A, Nyboe Andersen A. Embryo morphology or cleavage state: How to select the best embryos for transfer after in-vitro fertilization. Hum Reprod. 1997;12:1545–1549. doi: 10.1093/humrep/12.7.1545. [DOI] [PubMed] [Google Scholar]
- 9.De Placido G, Wilding M, Strina I, Alviggi E, Alviggi C, Mollo A, et al. High outcome predictability after IVF using a combined score for zygote and embryo morphology and growth rate. Hum Reprod. 2002;17:2402–2409. doi: 10.1093/humrep/17.9.2402. [DOI] [PubMed] [Google Scholar]
- 10.Miliki A, Hinckley M, Gebhardt J, Dasig D, Westphal L, Behr B. Accuracy of day 3 criteria for selecting best embryos. Fertil Steril. 2002;77:1191–1195. doi: 10.1016/S0015-0282(02)03104-7. [DOI] [PubMed] [Google Scholar]
- 11.Rijnders P, Jansen CA. The predictive value of day 3 embryo morphology regarding blastocyst formation, pregnancy and implantation rate after day 5 transfer following in-vitro fertilization or intracytoplasmic sperm injection. Hum Reprod. 1998;13:2869–2873. doi: 10.1093/humrep/13.10.2869. [DOI] [PubMed] [Google Scholar]
- 12.Desai N, Goldstein J, Rowland D, Goldfarb J. Morphological evaluation of human embryos and derivation of an embryo quality scoring system specific for day 3 embryos: A preliminary study. Hum Reprod. 2000;15:2190–2196. doi: 10.1093/humrep/15.10.2190. [DOI] [PubMed] [Google Scholar]
- 13.Terriou P, Sapin C, Giorgetti C, Hans E, Spach JL, Roulier R. Embryo score is a better predictor of pregnancy than the number of transferred embryos or female age. Fertil Steril. 2001;75:525–531. doi: 10.1016/S0015-0282(00)01741-6. [DOI] [PubMed] [Google Scholar]
- 14.Fisch JD, Sher G, Adamowicz M, Keskintepe L. The graduated embryo score predicts the outcome of assisted reproductive technologies better than a single day 3 evaluation and achieves results associated with blastocyst transfer from day 3 embryo transfer. Fertil Steril. 2003;80:1352–1358. doi: 10.1016/j.fertnstert.2003.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999;14:2345–2349. doi: 10.1093/humrep/14.9.2345. [DOI] [PubMed] [Google Scholar]
- 16.Peterson CM, Reading JC, Hatasaka HH, Jones KP, Udoff LC, Adashi EY, et al. Use of outcomes-based data in reducing high-order multiple pregnancies: The role of age, diagnosis, and embryo score. Fertil Steril. 2004;81:1534–1541. doi: 10.1016/j.fertnstert.2004.01.023. [DOI] [PubMed] [Google Scholar]