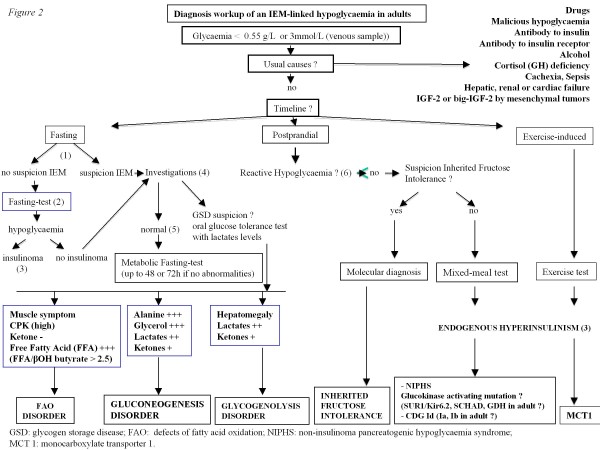
Figure 2.
Diagnosis workup of an IEM-linked hypoglycaemia in adults. (1) suspicion IEM: familial history of hypoglycaemia or rhabdomyolysis, hypoglycaemia starting during childhood, unexplained muscular symptoms (myalgias, high CPK levels), cardiac involvement and/or hepatomegaly. (2) fasting of up to 72 h if no abnormalities. Blood glucose, cortisol, Growth Hormone, insulin, C peptide, proinsulin and beta hydroxybutyrate should be measured every 6 h if the blood glucose level is > 0.6 g/L and then every 1 to 2 h (with capillary blood glucose test) if this level drops below 0.6 g/L. Fasting should be stopped if the blood glucose level is <0.45 g/L and occurs with hypoglycaemia symptoms, or if this level is <0.3 g/L regardless of the symptoms. Baseline blood measurements should be performed before glucose intake. (3) if glycaemia < 0.55 g/L (3 mmol/L): Detectable insulin (> 3 mIU/L (18 pmol/L), IRMA), C peptide > 0.6 ng/ml (0.2 nmol/l), β-OH butyrate < 2.7 mmol/L, sulfamide and repaglinide negative, 1 mg Glucagon IV test : + 0.5 g/L at 30 min (1.4 mmol/L). (4) investigations: abdominal ultrasound, EKG, echocardiography and laboratory measurements including acylcarnitine profile, total and free carnitin, urine organic acids, CPK, blood lactate levels, triglycerides, uric acid, liver enzymes. (5) normal or no evidence for defects of FAO. (6) CGMS (Continuous Glucose Monitoring System).