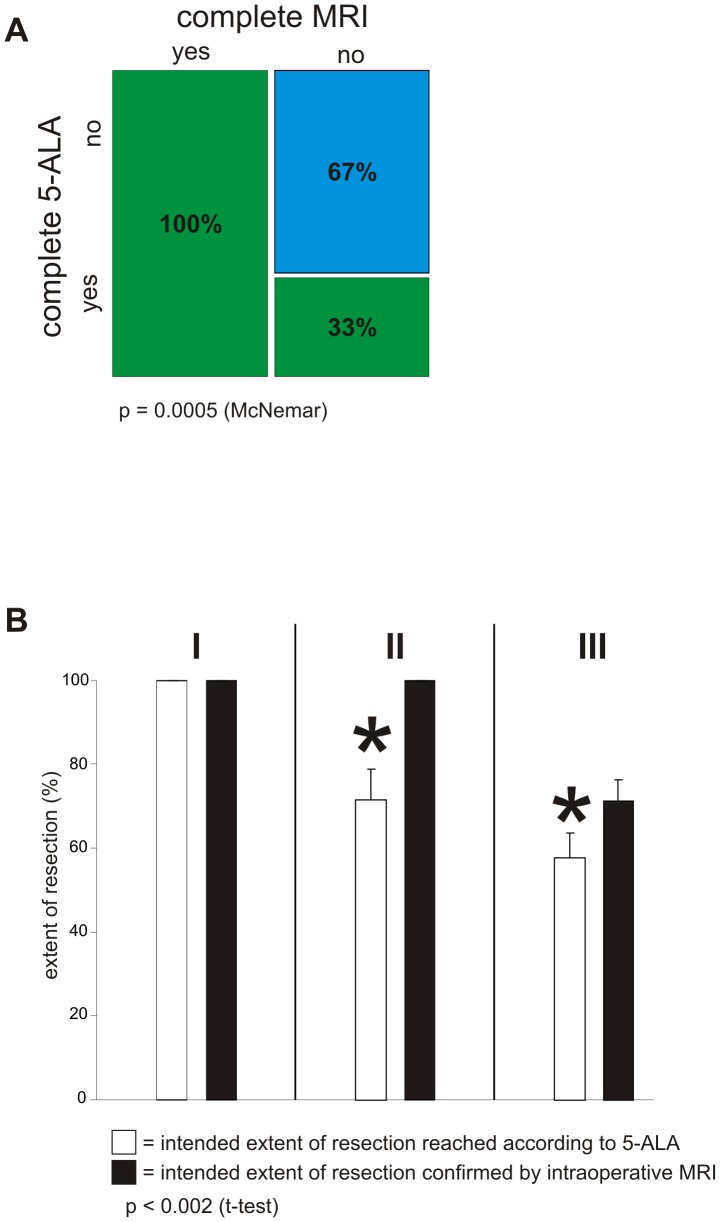
Figure 5. Dual intraoperative visualization approach in different functional grade patients.
A, Extent of resection was determined by 5-ALA and the results verified through iMRI. This was defined as one sequence of the procedure. 21 sequences showing complete resection according to 5-ALA were confirmed by iMRI (complete 5-ALA: yes, complete MRI: yes – green bar, first column). 14 sequences showing complete resection according to 5-ALA could not be confirmed by iMRI, which detected residual tumor (complete 5-ALA: yes, complete MRI: no – green bar, second column). 29 sequences showed residual tumor both according to 5-ALA as well as iMRI (complete 5-ALA: no, complete MRI: no – blue bar, second column). The order of these sequences resulted in a p-value = 0.0005 (McNemar). B, Functional tumor localization was categorized according to Sawaya [20]. Tumors in non-eloquent areas were defined as functional grade I [marked with I]. Functional grade II was defined as tumor localization close to an eloquent brain area [marked with II]. Functional grade III (given as III at the top) was defined as tumor localization in an eloquent brain area. Extent of resection was calculated as a percentage of prior tumor volume. Within the subgroup I the intended 100% resection was achieved by surgery with 5-ALA alone. In the subgroup II 5-ALA alone resulted in a tumor resection of 71.7% (±7.285 sem), whereas additional use of iMRI significantly increased tumor resection to 100% (p-value<0.002; Student's t-test). The subgroup III showed significant difference in extent of tumor resection. The results of tumor resection were 57.6% (±6.01 sem) achieved with 5-ALA alone, whereas a further tumor resection up to 71.2% (±5.257 sem) could be achieved through the additional use of iMRI.