Abstract
Systemic sclerosis is a rare connective tissue disorder with a wide range of oral manifestations. This case series reports significant oral and periodontal changes and also makes an attempt to correlate oral and systemic findings in these patients which enable the clinician for a better diagnosis and evolve a comprehensive treatment plan. Six patients with a known diagnosis of systemic sclerosis were included. After obtaining the patient's informed consent, relevant medical history, oral manifestations including periodontal findings and oral hygiene index simplified index were recorded. In these patients, oral changes included restricted mouth opening and, resorption of the mandible. The periodontal changes observed were gingival recession, absence or minimal gingival bleeding on probing, and widened periodontal ligament space, radiographically. Patients with systemic sclerosis often show wide range of oral manifestations, which is of major concern for the dentist.
Keywords: Bone resorption, calcinosis, panoramic radiography, periodontal ligament, scleroderma systemic, telangiectasis
INTRODUCTION
Systemic sclerosis is a chronic multisystem disorder, clinically characterized by thickening of the skin caused by excessive accumulation of connective tissue. It consists of two variants; 1) diffuse cutaneous scleroderma, which often shows involvement of proximal and distal extremities, face, trunk, kidney, and visceral organs and the 2) limited cutaneous scleroderma, which is limited to distal extremities and face, and also shows features of CREST syndrome (Calcinosis, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly and Telangiectasia). The involvement of visceral organs may also occur in the absence of skin involvement, which is referred to as systemic sclerosis sine scleroderma. The annual incidence has been estimated to be 19% per million populations and often shows more predilections for female compared to male (1:3 ratio). The incidence increases with age, peaking in the third to fifth decade.[1] The exact etiology is unknown, but it is characterized by both vascular injury and excessive production of normal collagen due to stimulation of fibroblasts caused by the mediators produced by T-lymphocytes. Also, another theory supports that defects in cell mediated immunity increases collagen production resulting in fibrosis.[2]
One of the first signs of the disease is Raynaud's phenomenon (bluish discoloration of hands on exposure to cold) followed by the resorption of the terminal phalanges and flexion contractures resulting in shortened, claw like fingers. Ulceration of the finger tips due to abnormal collagen deposition is also noted. The skin develops a diffuse, hard texture which is difficult to pinch (hide bound skin) and its surface is usually smooth, taut, mask like facies. Similarly, the nasal alae become atrophied, resulting in a pinched appearance to the nose, called a mouse facies.[3] Skin over the extremities, faces, and trunk may become darkly pigmented and contrasting areas of hypo pigmentation may also develop. The sparing of pigment around hair follicle gives the skin a ‘salt and pepper’ appearance.[4]
The oral manifestations include microstomia, xerostomia, telangietasia, increased decayed, missing and filled teeth.[3,5–7] The tongue can also become rigid, making speech and swallowing difficult. The soft tissues around the temperomandibular joint were also affected, which results in pseudoankylosis. The loss of attached gingiva and gingival recession may also occur. The radiographic findings include; uniform widening of the periodontal ligament space, especially around the posterior teeth. Also the mandible shows varying degree of bone resorption.[8] Since systemic sclerosis is a very rare, systemic disease having oral and periodontal implications and till date, to the best of our knowledge the periodontal manifestations associated with systemic sclerosis have not been described in the literature. This case series makes an attempt to correlate these findings with the systemic manifestations which enable the clinician in proper diagnosis and evolve a proper treatment plan for the individual cases.
CASE REPORT
Six patients with a confirmed diagnosis of systemic sclerosis referred from the Department of Dermatology and Venerology, JJM Medical College and Hospital, Davangere, to the Bapuji Dental College and Hospital, were included in this case series. After obtaining the patient's informed consent, relevant medical history and also oral findings including panaromic radiographs were recorded. Further analysis including Oral hygiene index simplified index (OHIS index) were done to assess the oral hygiene status.
A 36-year-old female was admitted to the dermatology ward with a complaint of difficulty in swallowing. Patient also reported a history of pain and bluish discoloration of her hands, on exposure to cold; ulceration over the digits; and progressive skin tightening with both hyper and hypo pigmentation since three years. As the disease progressed, she developed restricted mouth opening, heart burn, dysapnea, and altered bowel habits. Based on her history, clinical findings and further investigations, it was diagnosed as a case of systemic sclerosis.
On cutaneous examination, the skin over the face and extremities appeared shiny, stretched associated with hyper and hypo pigmented hidebound skin. She was having difficulty in dressing and holding onto objects because of the flexion deformities of her fingers [Figure 1a]. Digital pitted scars and receded pulp of the fingers were also noticed [Figure 1b], in addition to an ulcer on the ventral aspect of upper limb preceded by calcinosis cutis [Figure 1c]. Extra oral examination revealed loss of expression lines on the face, giving a mask like appearance, and the lips were thinned out resembling a fish mouth with a beak shaped nose [Figure 1d]. There was tenderness on tempero-mandibular joint on palpation on both the sides.
Figure 1.
(a) Deformed terminal phalanges with hyper and hypo pigmentation; (b) Digital pitted scars; (c) Calcinosis cutis; (d) Mask-like face, small pinched nose along with fish mouth appearance
Intraoral findings include; fibrosis of the tongue with reduced mobility, loss of papillae, generalized pallor and blanching of the mucous membrane, and diffuse fibrosis of the buccal mucosa with loss of normal elasticity. Also, a diminished oral aperture with the interincisal distance of 2.3 cm was noted. Periodontal findings include; generalized gingival recession and grade 1 mobility, in relation to lower anterior teeth [Figure 2]. Another striking gingival finding is that 95% of the sites examined showed no signs of gingival bleeding on probing, although her oral hygiene status was poor as demonstrated by OHI-S index. Patient's panoramic view revealed striking bilateral resorption of the angle, lower border and posterior border of ramus on right side of the mandible, and also generalized symmetrical widening of the periodontal ligament space was noticed [Figure 3]. Since patients were referred to us by the dermatologist for their dental care, all patients were given basic periodontal therapy that includes; motivation, education, and oral hygiene instructions, and scaling and root planing. All the patients were under observation. Additionally, mouth stretching exercises and facial grimacing was advised.
Figure 2.

Diffuse fibrosis of the buccal and labial mucosa and gingival recession in lower anterior teeth
Figure 3.

Panoramic radiograph of case 1 showing generalized symmetrical widening of the periodontal ligament space with bilateral resorption of the angle, lower border of the mandible and posterior border of ramus on right side
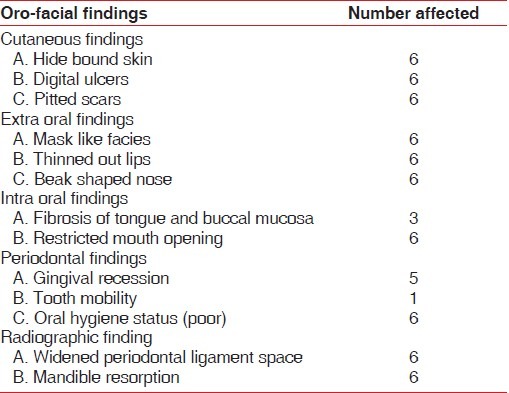
The findings observed in all the six patients have been summarized in Table 1.
Table 1.
Orofacial findings in systemic sclerosis patients
DISCUSSION
Systemic sclerosis (SS) is a generalized disorder of small arteries, microvessels and connective tissue, characterized by fibrosis and vascular obliteration in the skin, gastrointestinal tract, lungs, heart, and kidneys.[9] In the present case series, the soft tissue manifestations were similar to those reported in the earlier reports. Limited mouth opening was a major complaint among these patients, and was documented clinically. In a study of 21 patients with SS, Marmary and co-authors have found that 80% of SS patients were unable to open beyond 40 mm.[5] Although the sclerosis of the perioral tissues is considered to be the primary reason for limited opening, Weisman et al. and Eversole et al. have reported a significant percentage of temperomandibular joint (TMJ) dysfunction in their patients with systemic sclerosis. Associated dysphagia resulting from fibrosis of the tongue and smooth muscles of esophagus was also prevalent in these patients. However, xerostomia with high dental caries prevalence was not encountered in our patients as compared to other studies.[5,10,11]
Weisman et al.[12] and Eversole et al.[13] found that patients with SS who had severe buccal fibrosis with limited opening had mucogingival problems including loss of attached gingiva and multiple foci of gingival recession. In our present study, only one patient showed generalized gingival recession. Another striking feature in these patients was that only 94% of the examined sites showed the absence of gingival bleeding on probing, in spite of poor oral hygiene. This may be attributed to vasculopathy caused by excessive accumulation of collagen in the small arteries. These patients often suffer from severe flexion deformities of their fingers and other body joints; and thus have reduced manual dexterity. Maintenance of oral hygiene may be difficult due to the patient's inability to grip and manipulate a tooth brush or other oral hygiene aids. This particular problem of reduced manual dexterity may be attributed to the maintenance of poor oral hygiene by our patients.
Radiographically, the striking feature of this disease is the widening of the periodontal ligament space. Seifert, White and others have reported that this is an inconsistent finding in all patients with Progressive systemic sclerosis; however, this was contradicted by Marmary and others, who observed widened periodontal ligament space in all 21 patients examined.[5,14,15] In our study, 66% of the patients showed widened periodontal ligament space, and only one patient demonstrated more pronounced widening periodontal ligament space in posterior teeth when compared to anterior teeth as observed by Alexandridis and White.[16] Enlarged periodontal ligament space may be caused by excess deposition of collagen and oxytalan fibers and subsequent resorption of the alveolar crest bone surrounding the roots.[7,17] Despite of widening, the teeth were not mobile and the gingival attachment was intact which required no intervention.
Taveras[18] reported the first documented case of osteolysis of the mandibular angle and condyle in adult patients with scleroderma. Subsequently, several studies have documented the resorption of the condyle, zygomatic arch, angle, and coronoid process.[15,18–21] The exact etiology of the osteolysis is unknown, but there are three proposed theories: 1) tightening of the facial skin may exert excessive pressure on the mandible and induce the bone loss; 2) the vasculopathy associated with this disease may diminish the blood supply to the mandible resulting in bone ischemia and necrosis; and 3) atrophy of the muscles of mastication may lead to bone necrosis.[22]
In our study, the angle of the mandible was involved in 83.33% of patients followed by the condyle and the posterior border of the ascending ramus, similar to the observations made by Haers and Sailer.[23] There are conflicting reports on the correlation between progression or duration of systemic sclerosis and severity of bone resorption. Wood and Lee,[7] in a study of 31 women with systemic sclerosis found that 29% had resorption of the mandible, and all these patients demonstrated greater restriction in mouth opening and more widespread organ involvement. Another study found no correlation between bone resorption at the angle of the mandible, widening of periodontal ligament, age, duration of the disease and medication/clinical or laboratory findings.[5] Follow-up of these patients with periodic panoramic radiographs is essential to monitor and intercept potential consequences like pathological fractures and neuropathies.
Systemic sclerosis can give rise to various oral problems, most commonly limited mouth opening. Mouth stretching exercises and facial grimacing probably are the best treatment options for this problem. Good oral care is essential for patients with systemic sclerosis helping them to keep the mouth free of dental caries and periodontal diseases. It is advised that patients with scleroderma should visit the dentist and dental hygienist at least once in three months to ensure the maintenance of good oral health care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Gilliland BC. Systemic sclerosis (scleroderma) In: Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 15th edition. Vol. 2. New York City, U.S: Mc Graw–Hill company; 2001. pp. 937–38. [Google Scholar]
- 2.Martin SG. Immunological diseases. In: Malcolm AL, Vernon JB, Martin SG, editors. Burkitt's oral medicine diagnosis and treatment. 8th edition. Philadelphia: J.B. Lippincott Company; 1994. p. 579. [Google Scholar]
- 3.Neville BW. Dermatologic diseases. In: Neville BW, Damm DD, Carl MA, Jerry EB, editors. Oral and maxillofacial pathology. 2nd edition. Netherlands: Elsevier; 2002. pp. 692–693. [Google Scholar]
- 4.Gilliland BC. Systemic sclerosis (scleroderma) In: Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 15th edition. Vol. 2. New York City, U.S: Mc Graw-Hill Company; 2001. p. 1941. [Google Scholar]
- 5.Marmary Y, Glaiss R, Pisanty S. Scleroderma: Oral manifestations. Oral surg Oral Med Oral Pathol. 1981;52:32–37. doi: 10.1016/0030-4220(81)90169-9. [DOI] [PubMed] [Google Scholar]
- 6.Parma BS, Ferreira PA, Fugazzotto PA, Calura G, Berdichevsky M, Ruben MP. Progressive systemic sclerosis (scleroderma): Oral – mucosal changes. Gen Dent. 1986;34:107–12. [PubMed] [Google Scholar]
- 7.Wood RE, Lee P. Analysis of the oral manifestations of systemic sclerosis. Oral Surg Oral Med Oral Pathol. 1988;65:172–178. doi: 10.1016/0030-4220(88)90161-2. [DOI] [PubMed] [Google Scholar]
- 8.Martin SG. Immunological diseases. In: Malcolm AL, Vernon JB, Martin SG, editors. Burkitt's oral medicine diagnosis and treatment. 8th edition. Philadelphia: J.B. Lippincott Company; 1994. p. 580. [Google Scholar]
- 9.Leroy CE, Black C, Flieschmajer R, Jablonska S, Krieg T, Medsger TA, Jr, et al. Scleroderma (Systemic sclerosis): Classification, subsets and pathogenesis. J Rheumatol. 1988;15:202–205. [PubMed] [Google Scholar]
- 10.Alarcon SD, Ibanez G, Hernandez-Ortiz J, Velazquez-Forero F, Gonzalez-Jimeneez Y. Sjogren's syndrome in progressive systemic sclerosis (Scleroderma) Am J Med. 1974;57:78–85. doi: 10.1016/0002-9343(74)90771-2. [DOI] [PubMed] [Google Scholar]
- 11.Michanowicz AE. Arrested diffuse scleroderma. Oral Surg Oral Med Oral Pathol. 1962;15:1325. doi: 10.1016/0030-4220(62)90352-3. [DOI] [PubMed] [Google Scholar]
- 12.Man RA, Calcuterra TC. Head and neck manifestations of scleroderma. Ann Otol Rhinol Laryngol. 1978;87:332–339. doi: 10.1177/000348947808700307. [DOI] [PubMed] [Google Scholar]
- 13.Eversole LR, Jacobsen PL, Stone SS. Oral and gingival changes in systemic sclerosis (scleroderma) J Periodontol. 1984;55:175–178. doi: 10.1902/jop.1984.55.3.175. [DOI] [PubMed] [Google Scholar]
- 14.White SC, Frey NW, Blaschke DD, Ross MP, Clements PJ, Furst DE, et al. Oral radiographic changes in patients with progressive systemic sclerosis (scleroderma) J Am Dent Assoc. 1977;94:1178–82. doi: 10.14219/jada.archive.1977.0367. [DOI] [PubMed] [Google Scholar]
- 15.Seifert MH, Steigerwald JC, Cliff MM. Bone resorption of the mandible in progressive systemic sclerosis. Arthritis Rheum. 1975;18:507–12. doi: 10.1002/art.1780180514. [DOI] [PubMed] [Google Scholar]
- 16.Alexandridis C, White SC. Periodontal ligament changes in patients with progressive systemic sclerosis. Oral Surg Oral Med Oral Pathol. 1984;58:113–118. doi: 10.1016/0030-4220(84)90375-x. [DOI] [PubMed] [Google Scholar]
- 17.Stafne EC, Austin JL. A Characteristic dental finding in acrosclerosis and diffuse scleroderma. Am J Orthod Oral Surg. 1944;30:25–9. [Google Scholar]
- 18.Taveras JM. In: The interpretation of radiographs in disorders of the temperomandibular joint. L Schwartz ED, editor. Philadelphia: WD Saunders CO; 1959. p. 15960. [Google Scholar]
- 19.Hopper FE, Giles AD. Oral changes in systemic sclerosis - report of a case of resorption of mandibular angles and zygomatic arches. Br J Oral Surg. 1982;20:129–34. doi: 10.1016/0007-117x(82)90020-8. [DOI] [PubMed] [Google Scholar]
- 20.Bassets LW, Blocka KL, Furst DE, Clements PJ, Gold RH. Skeletal findings in progressive systemic sclerosis. AJR Am J Roentgenol. 1981;136:1121–6. doi: 10.2214/ajr.136.6.1121. [DOI] [PubMed] [Google Scholar]
- 21.Wardrop RW, Heggie AA. Progressive systemic sclerosis- oro-manifestations.Case report. Austr Dent J. 1981;32:258c–62. doi: 10.1111/j.1834-7819.1987.tb04150.x. [DOI] [PubMed] [Google Scholar]
- 22.Pogrel MA. Unilateral osteolysis of the mandibular angle and coronoid process in scleroderma. Int J Oral Maxillofac Surg. 1988;17:155–56. doi: 10.1016/s0901-5027(88)80020-1. [DOI] [PubMed] [Google Scholar]
- 23.Haers PE, Sailer HF. Mandibular resorption due to systemic sclerosis. Int J Oral Maxillofac Surg. 1995;24:261–267. doi: 10.1016/s0901-5027(95)80025-5. [DOI] [PubMed] [Google Scholar]



