Abstract
Purpose
Performing total knee replacement, accurate alignment and neutral rotation of the femoral component are widely believed to be crucial for the ultimate success. Contrary to absolute bone referenced alignment, using a ligament balancing technique does not automatically rotate the femoral component parallel to the transepicondylar axis. In this context we established the hypothesis that rotational alignment of the femoral component parallel to the transepicondylar axis (0° ± 3°) results in better outcome than alignment outside of this range.
Methods
We analysed 204 primary cemented mobile bearing total knee replacements five years postoperatively. Femoral component rotation was measured on axial radiographs using the condylar twist angle (CTA). Knee society score, range of motion as well as subjective rating documented outcome.
Results
In 96 knees the femoral component rotation was within the range 0 ± 3° (neutral rotation group), and in 108 knees the five-year postoperative rotational alignment of the femoral component was outside of this range (outlier group). Postoperative CTA showed a mean of 2.8° (±3.4°) internal rotation (IR) with a range between 6° external rotation (ER) and 15° IR (CI 95). No difference with regard to subjective and objective outcome could be detected.
Conclusion
The present work shows that there is a large given natural variability in optimal rotational orientation, in this study between 6° ER and 15° IR, with numerous co-factors determining correct positioning of the femoral component. Further studies substantiating pre- and postoperative determinants are required to complete the understanding of resulting biomechanics in primary TKA.
Introduction
Successful outcome after total knee arthroplasty (TKA) is strongly dependent on accurate component alignment and soft-tissue balancing [1].
Postoperative performance can be altered due to inadequate patellofemoral and tibiofemoral kinematics caused by malpositioning of components. Femoral component malrotation has been associated with numerous adverse complication and sequelae such as abnormal knee-kinematics causing increased shear forces and polyethylene-wear [2], instability [3, 4], stiffness [5], patella maltracking [3, 6] and poor outcome [7].
To establish neutral rotation of the femoral component intra-operatively, several methods are applicable. Measured resection methods reference the posterior femoral condyles [8, 9], the transepicondylar axis [10], or the antero-posterior axis (Whiteside-Line) [11]. The targeted rotational alignment of the femoral component is parallel to the transepicondylar axis [12] or slightly externally rotated [13]. In contrast, using the tension gap technique, the resection of the distal femur is dependent on the perpendicular tibial cut and ligamentous balancing in flexion to achieve a symmetrical flexion/extension gap [14]. The rotational alignment is therefore solely dependent on the ligamentous tension and the balancing of the flexion/extension gap, which might lead to aberrating values from neutral rotation of the femoral component [15, 16].
The issue of femoral component rotation continues to challenge surgeons and it remains unclear to what extent deviation in rotation is tolerable without poor functional outcome. Current knowledge about the importance of femoral rotational alignment remains controversial and clinical studies analysing the outcome and importance of rotational alignment are contended [15, 17]. We therefore hypothesized that a postoperative rotational alignment parallel to the transepicondylar axis within a range of 0° ± 3° of external/internal rotation would result in better subjective and objective outcome five years after TKA compared to more externally or more internally rotated components.
Patients and methods
After institutional review board approval had been obtained, we performed a clinical and radiographic retrospective study to evaluate the impact of rotational alignment on subjective and objective five-year outcome following mobile bearing cemented primary total knee arthroplasty. All procedures had been performed in our institution by experienced surgeons (including T.D.). Inclusion criteria were the following: (1) all consecutive primary total knee arthroplasties operated between June 1st and December 31, 2002 with a scheduled five-year follow-up in 2007, (2) use of the Innex UCOR mobile bearing (finalized design of 2002; Zimmer, Switzerland), (3) use of cemented fixation of all components. Exclusion criteria were: (1) primary patella resurfacing and (2) revision surgery during follow-up period not related to a possible femoral malrotation.
A total of 219 primary cemented total knee arthroplasty fulfilled these criteria.
Four patients (five knees) had died before the five-year follow-up examination of unrelated causes. Four patients were lost to follow-up and six patients underwent revision surgery; three patients were revised due to deep infections treated by one-step exchange in one case and by two-step exchange of implants in two cases. A 78-year-old female had secondary patella resurfacing to resolve persisting anterior knee pain (the rotation of the femoral component was within neutral range). In a 79-year-old female the femoral component was oversized (femoral component rotation was within neutral range) and a revision LCCK prosthesis was implanted with satisfying outcome. A 44-year-old male was revised four years postoperatively due to arthrofibrosis. Internal rotation of the femoral component of 10° was measured by CT-scan. In a first session, arthrolysis, PE-Inlay exchange and patella resurfacing was performed with unsatisfying result. In a second step the implants were removed and sonication of implants revealed chronic infection with Propionibacterium spp. After treatment for infection a LCCK revision prosthesis was successfully implanted.
In order to assess the rotational alignment of the femoral component, we used an axial radiography of the distal femur. The subject was placed on a wooden table (90 cm wide, 70 cm high, 55 cm long) on wheels. Patients sat on the table with the lower legs hanging freely with the axis of the tibia perpendicular to the floor and the axis of the femur perpendicular to the film cassette (adapted from Kanekasu 2005 [18]). The X-ray tube was positioned at one metre distance from the cassette and the beam pointed 10° upwards, with the central x-ray at the centre of the patella.
The data collection and radiographic evaluation based on the five-year follow up were performed by two independent observers (A.R. and T.G.), blinded to the clinical history and outcome of each patient.
The mechanical femoro-tibial axis was measured pre- and postoperatively using full-leg-length radiographs. The femoral component rotation was measured using the condylar twist angle (CTA). The CTA is defined as the span between the clinical transepicondylar axis—axis between the medial and lateral epicondyles—and the posterior condylar line [10].
Follow up was performed with the use of comprehensive data available from the joint replacement registry at our institution. This includes patient demographic data, date of evaluation (one-, two-, five-, ten- or 15-year follow-up), complications, reoperations, the Knee Society Score (KSS), clinical examination including ROM and stability in all planes, which is established pre-operatively and at every follow-up, as well as the subjective rating and radiographic evaluation and documentation of X-rays according to the methodology described by the American Knee Society [19]. Patient demographic data are expressed in Table 1.
Table 1.
Patient demographics
| Patient demographics | Value |
|---|---|
| Sex (female, male) | 126, 77 |
| Age, mean (range) | 71.7 (42–90) |
| BMI, mean (range) | 28.2 (16.9–46.5) |
| Etiology, total (%) | |
| Osteoarthritis | 179 (89) |
| Rheumatoid arthritis | 12 (5) |
| Posttraumatic | 13 (6) |
| Prosthesis, n (left, right, bilateral) | 119, 85, 11 |
BMI body mass index
Data based on 204 knees in 193 patients
Statistical evaluation was done using SPSS 15 (version 2007). All data were checked for normal distribution by means of Lilliefors test (an adaptation of Kolmogorov-Smirnov) and Wilk-Shapiro test. Correlations of the above-mentioned parameters were evaluated using Pearson’s test; distribution and null hypothesis were tested with Mann-Whitney. All tests were two-sided and statistical significance was set at a p-value ≤0.01. Intra-observer variability was performed to test repeatability and inter-observer variability was performed to test reproducibility for evaluation of radiographs.
Post hoc-power analysis was conducted to estimate the minimum sample size needed to observe a significant difference between the neutral rotation group and the outliers group. With regard to the KSS as primary endpoint, the effect size is very small (0.06), meaning that the difference between the mean value of the neutral rotation group and the outliers group is only 0.59 points. Given an alpha of 0.37 the power of the study will be 40 % assuming that a difference of 0.6 points will be detectable for patients and is of clinical importance. When the clinically important treatment effect in relation to KSS is set at a difference of 2 points, the power of this study increases to 83 % [20] and would be sufficient.
Results
A total of 204 knees were available for further analysis (see Table 1).
In 96 knees the five-year postoperative rotational alignment of the femoral component was within the range 0 ± 3° (neutral rotation group) and in 108 knees the five-year postoperative rotational alignment of the femoral component was outside of this range (outlier group). The postoperative CTA of all knees showed a mean of 2.8° (±3.4°) internal rotation (IR) with a range between 6° external rotation (ER) and 15° IR (Fig. 1). The inter- and intra-class correlation was CI 95.
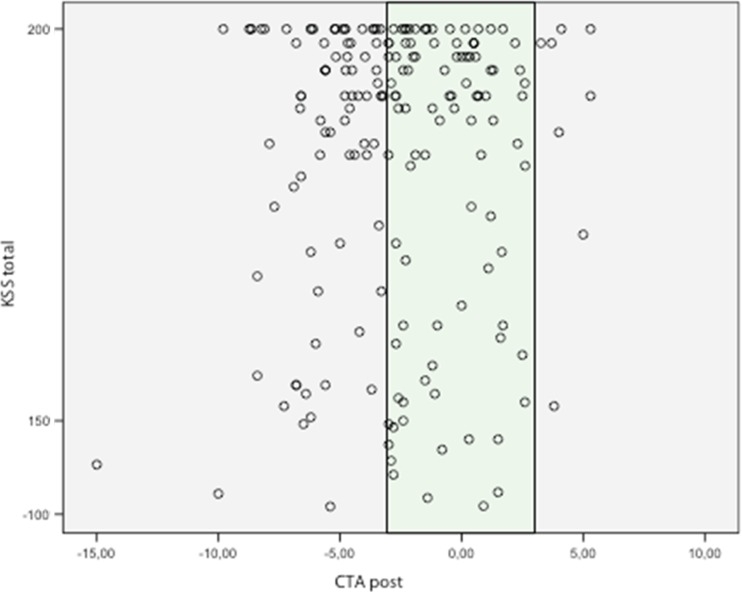
Fig. 1.
Relationship between Knee Society score and the rotation of the femoral component at the five-year follow up (CTA post). Negative values of CTA represent internal rotation (IR), positive values external rotation (ER). The single point marks the value of CTA on the X-axis, the neutral rotation group is marked in green. Presented values for femoral component rotation are consensus decisions
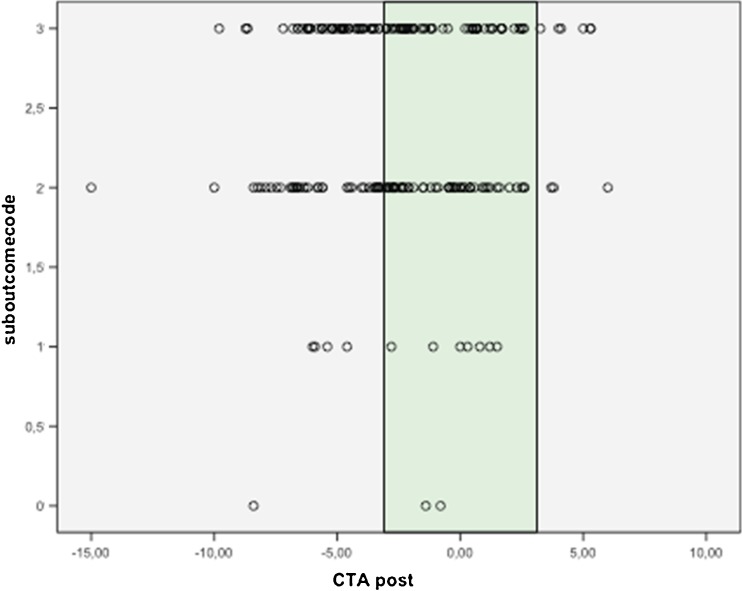
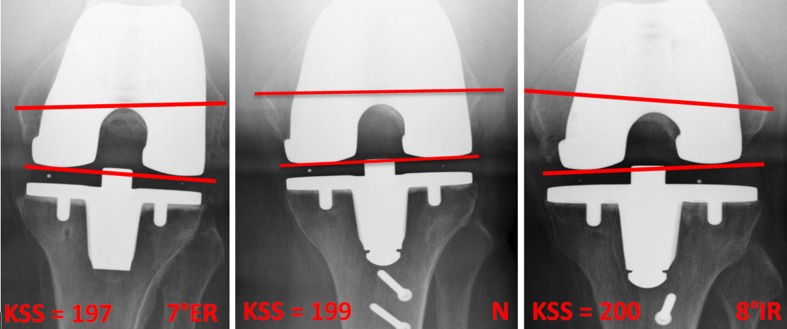
No statistically significant difference in terms of age, BMI and primary diagnostics could be detected between the two groups. There was no normal distribution of values (confirmed by Wilk-Shapiro test and Lilliefors test) and no statistically significant difference could be seen in relation to KSS (knee score [KS] and function score [FS]), range of motion, subjective rating, tibial PE wear, radiolucency and medio-lateral and antero-posterior stability (see Figs. 1, 2 and 3).
Fig. 2.
Subjective outcome versus rotational alignment of the femoral component, internal rotation (IR) represented by negative values, external rotation (ER) by positive values, the neutral rotation group is marked in green. Subjective outcome: 3—excellent, 2—good, 1—satisfactory, 0—poor
Fig. 3.
Axial radiographs at the five-year follow-up: on the left 7° external rotation (ER) of the femoral component, in the middle a femoral component with rotation parallel to the transepicondylar axis and on the right a patient with 8° internal rotation (IR) of the femoral component. All patients had excellent subjective and objective outcome
Discussion
Rotational alignment parallel to the TEA has been used as gold standard in postoperative evaluation [15], and it is well documented that a few degrees of deviation from the transepicondylar axis might lead to patellar maltracking or dislocation [21], knee instability [3], higher contact forces, pain [13], or arthrofibrosis [5, 22].
In contrast to the osseous landmark orientation technique, the tibia first technique is based on the principle of ligament balancing to achieve a symmetrical flexion and extension gap. To date, neither clinical nor biomechanical disadvantages could be shown as resulting from this technique [23, 24], though rotational alignment of the femoral component will not necessarily be parallel to the TEA [15, 16, 25].
Our results show a wide range of femoral component rotation between 6° ER and 15° IR, with only 49 % of femoral components being aligned parallel to the TEA ±3°. Similar results have previously been published. Siston et al. [26] performed a cadaver study using different techniques of knee replacement to measure accuracy of femoral component rotation. They found a wide range of rotational alignment of the femoral components between 13° of IR and 16° of ER, in all techniques used, including the “surgeons preferred technique” [26]. Matziolis et al. [15] stated that a perfectly balanced TKA will not lead to parallel alignment of the femoral component to the TEA, reporting a range between 7° IR and 6° ER of the component in the postoperative evaluation. Heesterbeck et al. could confirm that FCR is variable owing to patient variability and variation in ligament releases with a resection of −4° to 13° reference from the posterior condyles [16].
Longstaff et al. [27] found better function and faster rehabilitation with “good” alignment after TKA, as means of a global alignment score including FCR. In relation to the femoral component rotation we cannot confirm better function with “good” alignment. This may either be due to the fact that other than the authors we used the ligament balancing technique. Moreover, the use of mobile-bearings can, up to a limited degree, adapt and compensate for the rotational alignment between femoral and tibial components [28, 29]. Still, the range of possible compensation is limited and will not reduce patella-maltracking [30] or allow for higher range of motion [31].
Our hypothesis that subjective and objective outcome five years after cemented total knee arthroplasty would be better in patients with neutral rotational alignment of the femoral component than in patients with femoral component rotation outside of the given range could not be confirmed. In this retrospective clinical series, a femoral component rotation parallel to the transepicondylar axis ±3° did not result in better objective and subjective outcome at the five years follow up for 204 cemented mobile bearing knee arthroplasties compared to the outliers group.
So far there exists only little clinical mid- and long-term information with regard to the relationship between the rotational alignment of the femoral component and the subjective outcome, especially when analysing an overall collective and not only specific subgroups, e.g. poor outcome [22]. Our results do not support the hypothesis that a deviation from the TEA is equivalent to a mal-positioning of the femoral component. Today almost 50 % of revision surgery in painful knee arthroplasty is in some way linked to malpositioning/malrotation of components [27]. Therefore, the presented results might have an impact on indications for revision surgery in relation to femoral component malalignment.
The present study has several limitations. This is a retrospective study, patients are included five years after surgery, and the natural rotational orientation of the femur was not measured pre-operatively. In fact one patient of our study group underwent revision surgery for arthrofibrosis with a 10° IR of the femoral component postoperatively, which might have been one of the reasons for failure. In this case, too, we lack pre-operative femoral rotation measurements.
Also, we did not provide information about pre- and postoperative leg axis alignment. Further investigations are in process to study the relationship of pre-operative anatomy and rotational alignment of the femoral component.
A potential source of bias is the fact that eight patients had died or were lost to follow-up before final radiographic evaluation.
The radiographic measurements were performed independently by two blinded orthopaedic surgeons but were not revised by a specialized radiologist, which might be considered to be another drawback of the present study.
Furthermore, the follow-up of five years might not be long enough to be able to assess the long-term outcome and the difference in possible earlier PE-wear or loosening of components due to overstraining of the TKA. Additionally, this study focused on a static analysis on plain radiographs, without taking into account the dynamic alignment and forces acting on the knee joint after replacement. Despite these limitations, this study is to our knowledge the largest investigation of postoperative rotational alignment in relation to a five-year subjective and objective outcome. Effectively with regard to the Knee Society Score at the five-year follow up this study was adequately powered to detect a significant difference of 2 points KSS with 83 % power.
It is important to not overemphasize the findings of the present study. This study only took into account two groups of knees, the neutral rotation group and the outliers group, with either more external or more internal rotation of the femoral component. The uniform statement that femoral component rotation is not important is not permissible! Our retrospective study simply demonstrated that femoral component rotation outside the given range of 0° ± 3° must not have a disadvantage on subjective and objective patients’ outcome five years after surgery. There might be many more variables that have to be taken into account when analyzing the “well-positioned and well-aligned” total knee arthroplasty. As dynamic loading of the knee joint is a very complex, multidimensional process [32, 33], load distribution and contact/shear forces might not be the same for all patients and therefore also alignment may be more individual and specific for every patient. In accordance with Parrate et al. [34], we agree that for many patients the target value for postoperative alignment in the frontal plane and the axial plane may fall within the range 0° ± 3° of femoral component rotation. However, for any individual patient those values may vary due to various anatomical, physiological or possibly neurological reasons, with the individual target values lying outside of the postulated range. This makes it obviously difficult to define “correct” FCR when using the ligament balancing technique.
However, until additional and prospective data can be generated to more accurately determine the ideal postoperative rotational alignment of the femoral component for an individual patient, the chosen technique for implantation of TKA, either the measured resection technique aligning the component parallel to the TEA or the ligament balancing technique can be considered as valid standards.
Footnotes
Level of evidence
Level IV, retrospective study
References
- 1.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173–180. [PubMed] [Google Scholar]
- 2.Liau JJ, Cheng CK, Huang CH, Lo WH. The effect of malalignment on stresses in polyethylene component of total knee prosthesis—a finite element analysis. Clin Biomech. 2002;140:149. doi: 10.1016/s0268-0033(01)00109-7. [DOI] [PubMed] [Google Scholar]
- 3.Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;287:170–177. [PubMed] [Google Scholar]
- 4.Ziehlmann MS, Stacoff A, Roméro J, Krames-de-Quervain I, Stüssi E. Biomechanical background and clinical observations of rotational malalignment in TKA: literature review and consequences. Clin Biomech. 2005;20:661–668. doi: 10.1016/j.clinbiomech.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U. Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int Orthop. 2006;30:420–425. doi: 10.1007/s00264-006-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;366:155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Hanada H, Whiteside LA, Steiger J, Dyer P, Naito M. Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop Relat Res. 2007;462:137–142. doi: 10.1097/BLO.0b013e3180dc92e7. [DOI] [PubMed] [Google Scholar]
- 8.Hungerford D, Krackow K. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985;192:23–33. [PubMed] [Google Scholar]
- 9.Laskin R. Flexion gap configuration in total knee arthroplasty. J Arthroplast. 1995;10:657–660. doi: 10.1016/S0883-5403(05)80211-6. [DOI] [PubMed] [Google Scholar]
- 10.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 40–47 [PubMed]
- 11.Arima J, Whiteside LA, Mccarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am. 1995;77:1331–1334. doi: 10.2106/00004623-199509000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Churchill D, Incavo SJ, Christopher J, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;256:111. doi: 10.1097/00003086-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Miller MC, Berger R, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Büchel F. Surgical technique of the LCS. In: Hamelynck KJ, Stiehl JB, editors. LCS-mobile bearing knee arthroplasty. New York: Springer; 2002. pp. 121–135. [Google Scholar]
- 15.Matziolis G, Boenicke H, Pfiel S, Wassilew G, Perka C. The gap technique does not rotate the femur parallel to the epicondylar axis. Arch Orthop Trauma Surg. 2011;131:163–166. doi: 10.1007/s00402-010-1113-4. [DOI] [PubMed] [Google Scholar]
- 16.Heesterbeek PJC, Jacobs WCH, Wymenga AB. Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res. 2009;467:1015–1022. doi: 10.1007/s11999-008-0539-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee DS, Song EK, Seon JK, Park SJ. Effect of balanced gap total knee arthroplasty on intraoperative laxities and femoral component rotation. J Arthroplast. 2011;26(5):699–704. doi: 10.1016/j.arth.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Kanekasu K, Kondo M, Kadoya Y (2005) Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 434:193–197 [DOI] [PubMed]
- 19.Edwald F. The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 20.Petrie A. Statistical power in testing a hypothesis. J Bone Joint Surg Br. 2010;92:1192–1194. doi: 10.1302/0301-620X.92B9.25069. [DOI] [PubMed] [Google Scholar]
- 21.Berger R, Crossett L, Jacobs J, Rubash H. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat. 1998;11:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Boldt JG, Stiehl JB, Munzihger U, Beyerland D, Keblish PA. Femoral component rotation in mobile-bearing total K arthroplasty. Knee. 2006;13:284–289. doi: 10.1016/j.knee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Dennis D. Measured resection: an outdated technique on total knee arthroplasty. Orthopedics. 2008;31:940–943. doi: 10.3928/01477447-20080901-08. [DOI] [PubMed] [Google Scholar]
- 24.Chiavetta J, Fehring T, Odum S, Griffin W, Bohannon Mason J. Importance of balanced-gap technique in rotation platform knees. Orthopedics. 2006;29:45–48. [PubMed] [Google Scholar]
- 25.Fehring T. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2002;380:72–79. doi: 10.1097/00003086-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87:2276–2280. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 27.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplast. 2009;24:570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Dennis D, Komistek R, Mahfouz M. Mobile-bearing total knee arthroplasty; do the polyethylene bearings rotate? Clin Orthop Relat Res. 2005;11:88–95. doi: 10.1097/01.blo.0000185464.23505.6e. [DOI] [PubMed] [Google Scholar]
- 29.Fehring T. Ligamentous balancing in rotating-platform knees. Orthop Traum Surg Res. 2006;29:56–59. [PubMed] [Google Scholar]
- 30.Colwell C, Jr, Chen P, D’Lima D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech. 2010;26:52–57. doi: 10.1016/j.clinbiomech.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Ball ST, Sanchez HB, Mahoney OM, Schmalried TP. Fixed versus rotating platform total knee arthroplasty: a prospective, randomized, single-blind study. J Arthroplast. 2011;26(4):531–536. doi: 10.1016/j.arth.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 32.Schache AG, Baker R, Lamoreux LW. Defining the knee joint flexion-extension axis for purposes of quantitative gait analysis: an evaluation of methods. Gait Posture. 2006;24:100–109. doi: 10.1016/j.gaitpost.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Lovejoy CO. The natural history of human gait and posture. Part 3. The knee. Gait Posture. 2007;25:325–341. doi: 10.1016/j.gaitpost.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 34.Parratte S, Pagano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]