Figure 2.
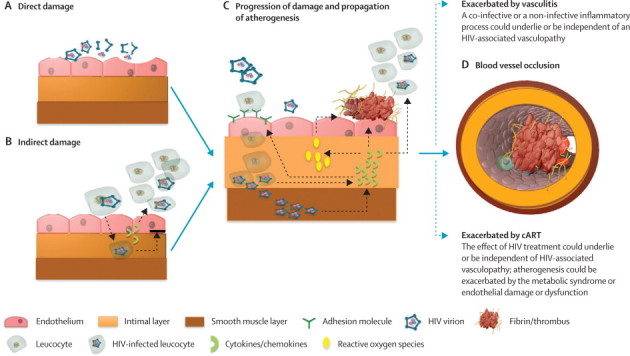
Hypotheses on the mechanism of HIV-associated vasculopathy
Mechanisms are specific to atheroma and potentially applicable to the other forms of HIV-associated vasculopathy. (A) Direct damage can occur through continuous exposure of the endothelium to HIV virion or viral particles (eg, GP120 or TAT) leading to endothelial dysfunction. (B) Indirect damage can arise from circulating infected monocytes freely transmigrating the endothelium as part of a normal surveillance, with an impaired reverse transmigration, thus increasing the subendothelial population of HIV infected monocytes. The release of chemokines such as CCL2 from infected leucocytes attracts more leucocytes. (C) Several events lead to the progression of damage and propagation of atherogenesis: upregulation of cell adhesion molecules (eg, selectins), leading to increased adhesion of infected or non-infected leucocytes; release of HIV virions into the arterial smooth muscle and continued active replication of the virus in smooth muscle cells; inflammatory cytokine release from HIV-infected cells, leading to further recruitment and adhesion of leucocytes, increased production of reactive oxygen species, and derangement of the coagulation system, favouring a prothrombotic state. Underlying this continuing process is the remodelling of the vessel wall, involving intimal hyperplasia and fragmentation of the elastic lamina. (D) Thrombotic occlusion of the vessel wall lumen is one of the outcomes of this process.
