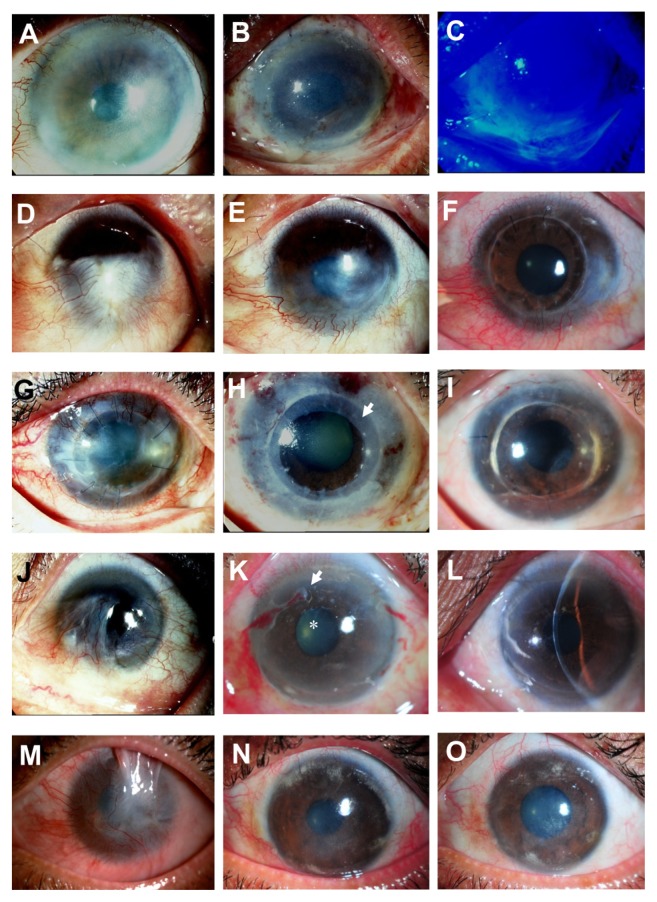
Figure 3.
Representative slit-lamp photographs show a comparison of the eyes before (left column) and after (middle and right column) cultivated limbal epithelial transplantation (CLET) in the clinical success group. Patient 3 (A) undergoes auto-CLET and 1 day postoperatively the entire corneal surface is covered with transplanted cultivated corneal epithelium (B) confirmed by fluorescein staining, with no conjunctival cell contamination (C). Patient 6, who has a chemical burn (D), undergoes auto-CLET, with resultant decreased corneal neovascularization postoperatively at 10 months after CLET (E). Penetrating keratoplasty is performed for optical reasons 16 months after CLET and the corneal graft remains clear 18 months after keratoplasty (F). Patient 7 underwent a previous penetrating keratoplasty to treat cytomegalovirus keratitis (G) with severe inflammation. Two days after auto- CLET with a 360-degree annular ring of CLET (arrow), the central area is spared (H). The corneal graft has recovered and become clear with no conjunctivalization up to 34 months after CLET (I). Patient 13, with idiopathic near-total limbal stem cell deficiency bilaterally (J), undergoes allo-CLET. The corneal epithelium becomes transparent 2 weeks postoperatively (K, arrow), dissolving amniotic membrane carrier of CLET; (star), disappeared amniotic membrane) without conjunctivalization up to 19 months (L). The visual acuity has improved from 20/800 to 20/40. Patient 16, with total limbal stem cell deficiency with upper lid symblepharon and chronic inflammation secondary to chemical burn (M), is markedly improved after allo-CLET. The clinical appearance at 4 (N) and 14 (O) months postoperatively, and the visual acuity has improved to 20/200 for counting fingers half a foot away.
Note: The visual acuity remains stable up to the last follow-up examination at 14 months.