Abstract
Background and Purpose
Chronic neck pain is prevalent in the workplace. Research suggests that psychosocial stress may contribute to the development of neck pain by causing excessive or prolonged muscle activity in some individuals. The purpose of this case report is to describe the rationale, development, and implementation of stress management as an adjunct to standard physical therapist management of chronic neck pain in a female office worker who responded to psychosocial stress with elevated muscle activity prior to treatment.
Case Description
A 44-year-old female office employee with an 8-year history of chronic neck pain participated in this case report. The patient was selected from a group of research participants who demonstrated elevated electromyographic (EMG) activity of the trapezius muscle in response to simulated occupational stressors. The multidisciplinary intervention consisted of 8 physical therapy sessions, supplemented by 8 stress management sessions that included EMG biofeedback and psychotherapy to facilitate muscle relaxation.
Outcomes
Neck disability decreased by 50%, trait anxiety decreased by 21%, and the duration of trapezius muscle rest in the workplace increased by 56% immediately after the 8-week intervention. These improvements were maintained 6 months after treatment, and the patient reported a complete absence of neck disability at the 2-year follow-up assessment.
Discussion
A sustained reduction in neck disability was observed for a patient with chronic neck pain after participating in a multidisciplinary intervention that combined physical therapy and stress management approaches to facilitate muscle relaxation in the workplace. Future clinical trials are needed to assess whether stress management is a useful adjunct therapy for patients with chronic neck pain who show elevated muscle activity in response to psychosocial stress.
Musculoskeletal disorders (MSDs) are common in the workplace, with a lifetime prevalence of neck pain as high as 78% among office workers.1 Neck pain is classified as chronic when symptoms are present for 3 or more months, with either recurrent (multiple episodes separated by periods of recovery) or persistent (no periods of recovery) pain.2 Strong evidence suggests that biomechanical factors, including repetitive movements, prolonged computer use, and poor workstation design, are associated with the development of neck pain.3 In addition to biomechanical factors, psychosocial stress in the workplace may contribute to neck pain in some individuals.4 For example, activation of trapezius muscle motor units has been observed during mentally stressful tasks performed in the absence of physical demands,5 and the combination of mental and physical stress has been shown to increase trapezius muscle activity more than the summed effect of each stressor alone.6 Thus, chronic exposure to psychosocial stressors in the workplace may contribute to the sustained activation of trapezius muscle motor units, placing this muscle at greater risk of overuse injury.
Electromyography (EMG)-assisted biofeedback involves monitoring muscles with surface EMG and using feedback of the EMG signal to assist patients in altering their muscle activity. Biofeedback has been used in clinical trials to reduce overuse syndromes of the cervical musculature by alerting patients when their muscle exceeds a given threshold of activity7 or when the muscle has insufficient periods of rest throughout the workday.8–10 One recent study demonstrated no difference in the efficacy of EMG biofeedback compared with ergonomic counseling for the management of neck pain.8 However, the investigators noted clinically meaningful improvement in approximately half of patients treated with biofeedback and suggested that future studies would benefit from methods to identify the subgroup of patients for whom biofeedback is most appropriately prescribed. To our knowledge, none of the available studies on stress-management or biofeedback interventions for chronic neck pain have attempted to screen patients for heightened levels of anxiety or muscle activity prior to targeting these impairments for intervention.
Common physical therapy interventions for neck pain include therapeutic exercise, manual techniques, aerobic conditioning, ergonomic counseling, and physical modalities. With the exception of modalities, evidence generally supports the short-term efficacy of these conservative interventions,11–14 yet the majority of patients with neck pain experience poor long-term outcomes and a high recurrence rate with the current standard of care.15 This finding is especially true among office workers, for whom the 12-month recurrence rate for neck pain can reach 60% to 80%.16
There is growing recognition within the physical therapy profession that the evaluation and management of chronic pain require an integrated approach that considers both biomedical and psychosocial barriers to functional recovery.17,18 Psychologically informed physical therapist practice has recently been advocated for patients with chronic pain. This approach requires the development of validated screening tools for psychosocial impairments that can be implemented by physical therapists.18 The purpose of this case report is to describe the development and implementation of a novel approach using stress management, including biofeedback and psychotherapy techniques, as an adjunct to standard physical therapist management of chronic neck pain in a female office worker who responded to psychosocial stress with elevated muscle activity prior to treatment.
Patient History and Review of Systems
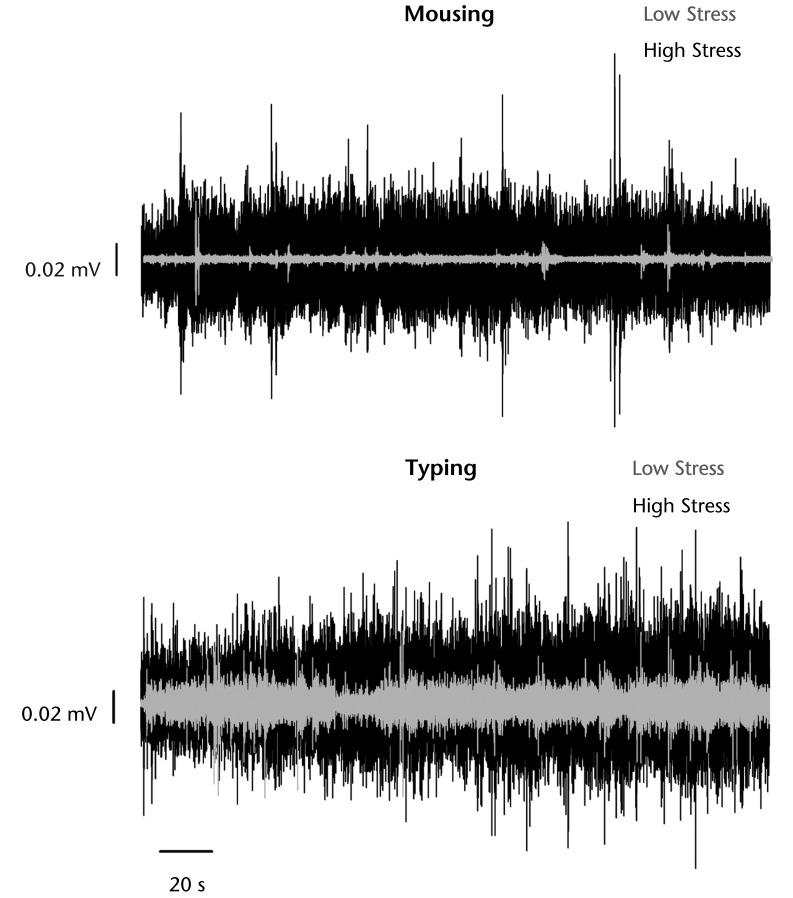
The patient in this case was selected from participants in an ongoing study of trapezius muscle activity during simulated occupational tasks performed under low and high stress conditions. The tasks were designed to simulate common psychomotor activities performed during computer office work, namely typing and mousing in the presence of high cognitive demands. During the low stress condition, participants were informed that the trial was just for practice and that their performance would not be monitored. The high stress condition was administered by an authoritative tester and was performed with time and accuracy constraints, video surveillance, verbal feedback regarding mistakes, and a monetary incentive for high scores. Both conditions were presented in a single session lasting approximately 25 minutes, with a 5-minute rest break separating the low and high stress conditions performed for 10 minutes each in consecutive order. The typing task required participants to type a standardized text presented on a computer screen at eye level, whereas the mousing task required them to solve complex arithmetic problems while memorizing lists of 2 to 8 words in sequential order. One participant exhibited a particularly large increase in muscle activity during the high stress condition (Fig. 1) and was invited to participate in an 8-week multidisciplinary intervention for chronic neck pain. The patient provided written informed consent prior to the intervention, in accordance with procedures approved by the Colorado Multiple Institutional Review Board.
Figure 1.
Stress-evoked muscle activity during simulated occupational stressors. Raw electromyographic recordings of the dominant upper trapezius muscle are shown for computer mousing and typing tasks performed under low stress (gray) and high stress (black) conditions. During the low stress condition, the patient was told that the trial was just for practice and that her performance would not be monitored. The high stress condition was administered by an authoritative tester and was performed with time and accuracy constraints, video surveillance, verbal feedback to correct mistakes, and a monetary incentive for high scores. Self-reported state anxiety increased from the low stress to the high stress condition (Speilberger State-Trait Anxiety Inventory state anxiety [STAI-S] score: low=24 points; high=33 points), whereas the magnitude of neck pain changed minimally across stress conditions (10-cm visual analog scale: low=3.8 cm; high=3.9 cm). Despite performing identical mousing and typing tasks across the 2 stress conditions, trapezius muscle activity increased markedly during exposure to the psychosocial stressor.
The patient was a 44-year-old woman who reported an 8-year history of chronic, recurrent neck pain. She described bilateral pain affecting the neck, upper trapezius muscle, mid-scapular, and upper-extremity regions. Symptoms were described as intermittent and aching pain, with occasional numbness and tingling in the neck, shoulders, and arms bilaterally. The patient rated the magnitude of her current pain as 2 to 3 out of 10 at best and as 10 at worst on a numeric pain rating scale. She was employed full-time in an office setting that required prolonged use of the computer keyboard and mouse. Prior treatments for her symptoms, including acupuncture, massage, and physical therapy, provided only temporary relief.
Examination
Based on initial findings from the EMG screening, the patient was considered a possible candidate for multimodal intervention combining physical therapy and stress management techniques. A brief screen described by other authors19 revealed no signs of neurologic impairment and was followed by a standardized history and physical examination for nonspecific mechanical neck pain adapted from Cleland et al20 and Shahidi et al.21 Cervical active range of motion (AROM) was assessed in a sitting position with an inclinometer and a long-arm goniometer.20 Glenohumeral AROM also was assessed in a sitting position with a long-arm goniometer to identify any restrictions of upper-extremity movement. To determine the contribution of joint mobility to deficits in AROM, passive intervertebral motion was assessed for areas of relative hypomobility or hypermobility and symptom reproduction in the cervical and thoracic spine.20
Manual palpation was used to identify localized regions of tenderness within muscles of the head and neck region, and pressure pain threshold (PPT) was used to quantify mechanical hyperalgesia of the upper trapezius muscle. Pressure pain threshold refers to the minimum pressure that is perceived as slightly painful when applied over the muscle belly with a handheld algometer. Upper trapezius PPT values are highly reliable, with a minimal detectable change of 47 kPa among patients with neck pain.22
A visual assessment of head, shoulder, and spine posture20 was conducted with the patient in sitting and standing positions, and impairments that may contribute to abnormal postures were assessed using standardized cervicoscapular length and strength tests.20,21 The craniocervical flexion test (CCFT) was used to assess motor control and endurance of the deep neck flexors, as scored on a 0- to 100-point performance index.23 Functional posture and movement also were assessed during a standardized ergonomic evaluation performed at the patient's work site according to recommendations published by the Occupational Safety and Health Administration (OSHA).24
Clinical Impression
Primary impairments identified during the physical examination are summarized in Table 1. All tests for neurologic impairment were negative. The patient exhibited deficits in cervical range of motion, muscle strength, and muscle length that were comparable or greater in magnitude than those previously documented among patients with chronic neck pain.21–22 Notably, impairments in shoulder range of motion, scapular strength, and pressure pain threshold were greater for the dominant (right) compared to the non-dominant upper extremity. These physical impairments were accompanied by postural deficits and a poorly designed workstation that likely increased biomechanical loading of the cervical spine and supporting musculature. Together, these findings suggested that excessive biomechanical demands contributed to cumulative trauma injury of the neck musculature, particularly the dominant upper trapezius muscle. Elevated trapezius muscle activity in response to simulated stressors during the EMG screening further suggested that psychosocial stress in the workplace may have contributed to cumulative muscle trauma. Given the patient's 8-year history of recurrent symptoms, the long-term prognosis was considered to be poor for conventional treatment approaches. Therefore, a multidisciplinary intervention was designed to address both biomechanical and psychosocial stressors, with the goal of achieving sustained reductions in neck pain and disability.
Table 1.
Impairment Findings From the Physical Examinationa
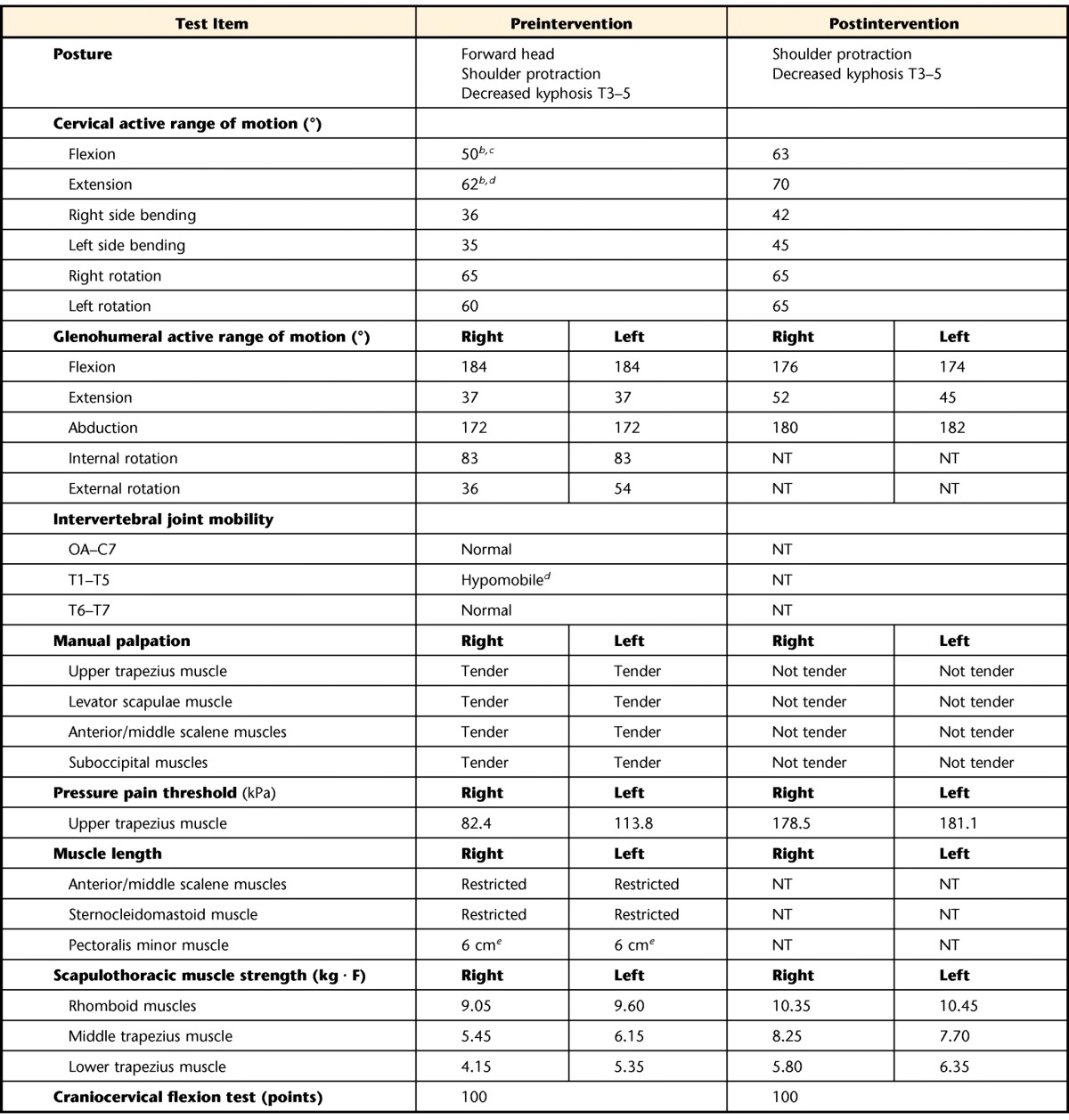
aOA=occipitoatlantal joint, C=cervical vertebrae, T=thoracic vertebrae, NT=not tested.
b Pain increased during active motion.
c Pain alleviated with passive shoulder elevation during motion.
d Pain increased during passive motion.
e Distance from posterior acromion to examination table with patient positioned supine.
Outcome Measures
Primary outcomes included self-reported changes in trait anxiety and neck disability and quantitative changes in trapezius muscle activity throughout the workday. Short-term outcomes were assessed prior to the physical examination, immediately after the 8-week intervention, and at 3- and 6-month follow-up assessments. Long-term changes in neck disability also were assessed 1 and 2 years after the intervention. Due to a change in the patient's employment setting prior to the 1-year assessment, only Neck Disability Index (NDI) scores are reported for long-term outcomes.
Psychological and Physical Health
Self-reported changes in psychological health were assessed using the trait portion of the Speilberger State-Trait Anxiety Inventory (STAI-T). Scores on this 20-item questionnaire range from 20 to 80 points, with higher scores indicating greater levels of enduring anxiety and a cutoff score of 32 points associated with significant generalized trait anxiety.25 Self-reported changes in physical health were assessed with the NDI, a 10-item questionnaire with scores ranging from 0 (no disability) to 50 (severe disability) points, with a minimal detectable change of 10 points documented for patients with mechanical neck pain of unspecified chronicity.26
Work-Site EMG Recordings
A portable data logger was used to monitor activity of the dominant upper trapezius muscle on 1 to 2 randomly selected workdays before and after the intervention. The patient was instructed to wear the monitor for 5 to 8 hours as she performed her usual activities in the workplace. To examine changes in the relative magnitude of muscle activity across time, work-site EMG recordings were expressed as a percentage of a submaximal reference voluntary contraction (RVC) performed at the beginning of each test day.
Surface EMG activity was recorded with a bipolar Ag-AgCl bar electrode (22-mm inter-electrode distance) positioned 2 cm lateral to the midpoint of the line between C7 and the acromion. A custom-designed, portable EMG instrumentation system was used to filter (10–4,000 Hz) and amplify (×1,000–2,000 gain) the signal, which then was root mean square (RMS) processed in real time (100-millisecond time constant) and stored at 100 Hz. The RMS recordings were imported into a custom-designed signal processing package to calculate occupational exposure measures as previously described.27,28 Static muscle activity was quantified as the EMG amplitude above which the muscle was active for 90% of the recording time.23 Muscular rest28 was estimated as the percentage of the total recording time that RMS values remained below a threshold set 2 standard deviations higher than the average RMS recorded at rest. Lower values of static muscle activity indicate that the muscle is active at lower contraction intensities throughout the workday, whereas higher values of muscular rest correspond to greater periods of relaxation throughout the workday. Ambulatory EMG measures have been shown to be reliable, even when repeated across several months.29
Intervention
The multidisciplinary intervention consisted of 4 weeks of physical therapy with two 60-minute sessions per week, followed by 4 weeks of stress management with one 60-minute session of EMG biofeedback and one 60-minute session of psychotherapy per week. The patient completed all scheduled clinic sessions; however, adherence to her prescribed home program was not monitored.
Physical Therapy
The physical therapy intervention consisted of therapeutic exercise, manual techniques, functional movement training, and ergonomic counseling as summarized below. Specific treatment techniques have been described elsewhere; therefore, interested readers are referred to previous literature for detailed descriptions of each intervention.
Manual Therapy
Manual therapy techniques included soft tissue massage, assisted stretching, and cervicothoracic joint mobilizations. Muscles that were tender or restricted in length were targeted for soft tissue massage and assisted stretching. Limited cervical range of motion and hypomobility of intervertebral motion in the thoracic spine were addressed with manual cervical traction and grade II through IV posterior-anterior mobilizations. Systematic reviews support the use of mobilization as part of a multimodal approach for the treatment of neck disorders,14 but report inconclusive evidence regarding the efficacy of massage used alone or in combination with other methods.30
Therapeutic Exercise
Therapeutic exercises were designed to reduce impairments contributing to forward shoulder and head posture, and included strengthening of cervicoscapular musculature through a combination of prescribed scapular exercises31 and performance of scapular retraction and craniocervical flexion during functional activities such as sitting and reaching. The patient also was instructed in a stretching program to be performed daily in the home or workplace.32 Finally, she was encouraged to incorporate regular aerobic activity into her weekly routine to improve overall physical conditioning. The patient was advised to continue her therapeutic exercise program after discharge from physical therapy to help prevent symptom flares. Strong evidence supports the efficacy of therapeutic exercise and physical conditioning for the management of chronic neck pain.11,12,14
Functional Movement Training and Ergonomic Counseling
There is limited evidence to support the efficacy of ergonomic modifications and functional movement training in the management of chronic neck pain. However, instruction in proper ergonomics during work and leisure activities was included in the physical therapy intervention based on known ergonomic risk factors for neck pain3 and evidence that therapeutic exercise alone does not necessarily improve patterns of muscle activation during functional activities.33 The patient was observed performing functional tasks that increased her neck pain and was instructed in alternative posture and movement strategies to alleviate her pain during these tasks. Once a pain-relieving strategy was identified, the patient practiced this motor pattern in the clinic and was encouraged to incorporate the new motor strategy into her daily activities. Additionally, the patient's workstation was modified in accordance with OSHA guidelines.24
Stress Management Intervention
The stress management intervention consisted of EMG biofeedback training provided by a physical therapist and psychotherapy provided by a clinical psychologist. The stress management intervention used in this case has not been previously described; therefore, specific tasks included in each treatment session are summarized in Table 2.
Table 2.
Stress Management Intervention
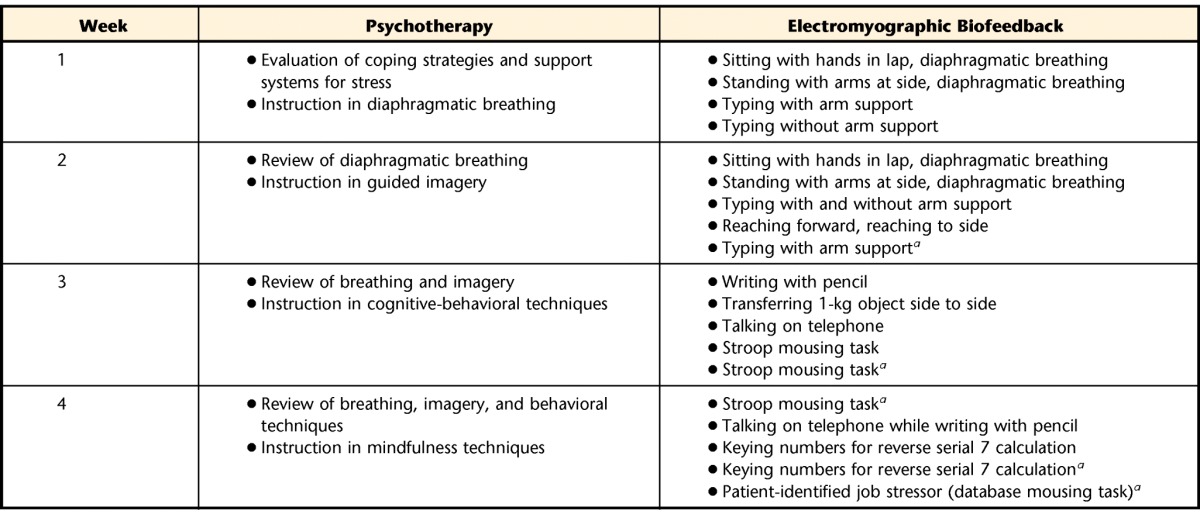
a Simulated occupational tasks performed with time and accuracy constraints.
EMG Biofeedback Training
Biofeedback training was prescribed based on findings of stress-evoked trapezius muscle activity during simulated work tasks (Fig. 1), suggesting that excessive muscle activity in response to occupational stressors may have contributed to the development or maintenance of trapezius muscle myalgia in this patient.
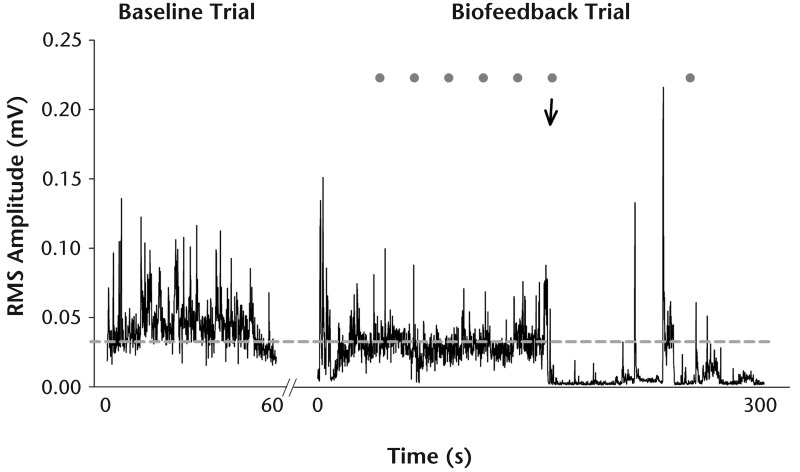
Electromyographic activity of the dominant trapezius muscle was recorded (13- to 1,000-Hz band-pass filter, 2,000-Hz sampling rate) with the muscle at rest and during a submaximal RVC at the beginning of each session. The patient then practiced 2 to 3 simulated work tasks with and without biofeedback. Tasks were designed to simulate activities that the patient frequently performed at her job and included motor and cognitive demands that progressively increased in difficulty across sessions (Tab. 2). The patient first performed each task using her preferred motor strategy without biofeedback. The mean amplitude of the RMS-processed (125-millisecond window) EMG signal recorded during this trial was considered the baseline level of muscle activity, and the EMG threshold for biofeedback training was set at 80% of the baseline muscle activity. The patient then was provided with auditory biofeedback cues, along with verbal and manual cues from the physical therapist, to assist with reducing trapezius muscle activity as she repeated two 5-minute trials of each task with biofeedback (Fig. 2).
Figure 2.
Representative recording of trapezius muscle activity during biofeedback intervention. Activity of the dominant upper trapezius muscle was monitored with surface electromyography (EMG) while the patient performed a Stroop mousing task (Tab. 2, session 3). The feedback threshold (dashed gray line) initially was set for this particular task at 80% of the mean muscle activity recorded during a 60-second baseline trial (left), which the patient performed using her preferred motor strategy without biofeedback. During the subsequent biofeedback trial (right), auditory cues (gray circles) were provided to remind the patient to relax whenever the amplitude of the EMG signal exceeded the feedback threshold in more than 20% of the samples recorded during the preceding 20-second monitoring window. Verbal and manual cues from the physical therapist also were provided to help the patient achieve and maintain a relaxed posture. After the patient failed to relax her muscles in response to auditory cues during the first half of the mousing trial, verbal instructions (arrow) were provided to “relax your shoulders and lean back against the chair.” This instruction allowed the patient to perform the required task while keeping her trapezius muscle relaxed for the remainder of the trial. RMS=root mean square.
Auditory feedback cues were provided at 20-second intervals whenever the RMS signal exceeded the feedback threshold in more than 20% of recorded samples for the preceding interval. When the patient was able to maintain her muscle activity below the feedback threshold for 2 consecutive intervals, the threshold was automatically decreased by 0.5% RVC. Electromyographic activity also was monitored during 2- to 3-minute rest breaks between tasks, and auditory cues were provided whenever muscle activity exceeded 10% of the resting EMG threshold, indicating insufficient muscle rest. After practicing each task with auditory feedback, the therapist discussed successful strategies for reducing muscle activity with the patient while viewing the EMG recordings together. The patient was sent an automated electronic reminder to “lean back, relax, breathe” every 30 minutes throughout her work day to help her apply these relaxation strategies in the workplace.
Psychotherapy
The goal of the psychotherapy intervention was to help the patient develop active coping skills for managing stress in the workplace. Psychotherapy sessions were administered by a clinical psychologist, who provided training in diaphragmatic breathing, guided imagery, cognitive behavioral therapy, and mindfulness techniques.34
Sources of perceived stress, outlets for stress relief, and available support systems were assessed during the first psychotherapy session. The patient then was instructed in diaphragmatic breathing and encouraged to incorporate this technique into her daily routine. Diaphragmatic breathing was reviewed in the second session, followed by an introduction to guided imagery. A videotape was provided for the patient to practice guided imagery at home. In the third session, the patient was introduced to cognitive-behavioral therapy, with instruction in methods to identify and balance 3 aspects of perception: facts, interpretation, and reaction to life events. The final session introduced mindfulness techniques that promote active observation of thoughts and events before reacting. Positive effects of psychotherapy have been observed among patients with chronic neck pain when cognitive-behavioral interventions were combined with physical conditioning.11
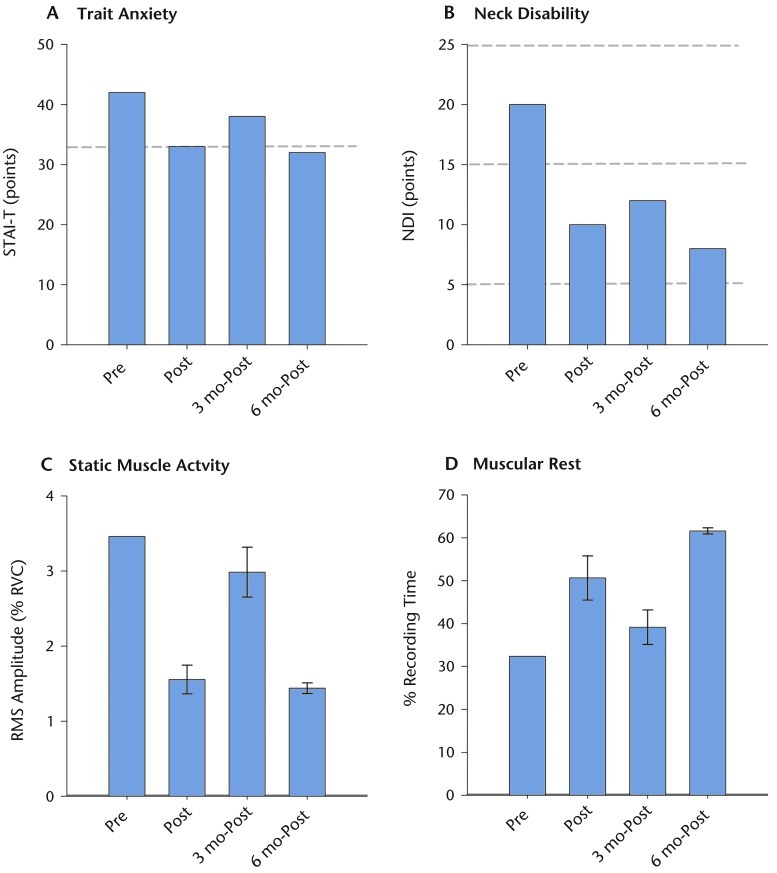
Outcome
The patient experienced improvements in all measured outcomes, with a long-term resolution of neck pain and disability. Trait anxiety (STAI-T scores) decreased by 21% immediately after the 8-week multidisciplinary intervention, and this reduction was maintained up to 6 months after treatment (Fig. 3A). Similarly, neck-related disability (NDI scores) decreased by 50% immediately after the 8-week intervention and remained decreased 6 months later. Long-term outcome assessments revealed a sustained reduction in the NDI score at 12 months (NDI score=8 points) and a complete absence of neck-related disability (NDI score=0 points) 2 years after treatment. Clinically meaningful improvements in physical impairment measures also were observed following the 8-week intervention (Tab. 1).
Figure 3.
Outcomes measured before and up to 6 months after treatment. Trait anxiety (A), neck disability (B), static muscle activity (C), and muscular rest (D) were assessed before (Pre), immediately after (Post), and 3 months (3 mo-Post) and 6 months (6 mo-Post) after the 8-week multidisciplinary intervention. Dashed gray lines indicate published cutoff scores for generalized trait anxiety on the Speilberger Trait Anxiety Inventory (STAI-T; A) and mild (5–15 points) to moderate (16–25 points) disability categories on the Neck Disability Index (NDI; B). The patient reported clinically significant improvements in trait anxiety and neck disability immediately after treatment that were maintained up to 6 months. Long-term improvements in neck disability were reported up to 2 years after treatment (NDI score=0 points; data not shown). The pattern of changes in static muscle activity and muscular rest recorded in the dominant upper trapezius muscle across time was similar to that observed for trait anxiety and neck disability, where lower values of static muscle activity and higher values of muscular rest indicate an overall reduction of muscle activity in the workplace following treatment. Error bars represent standard deviation of measurements obtained during 2 days of workplace monitoring. RMS=root mean square.
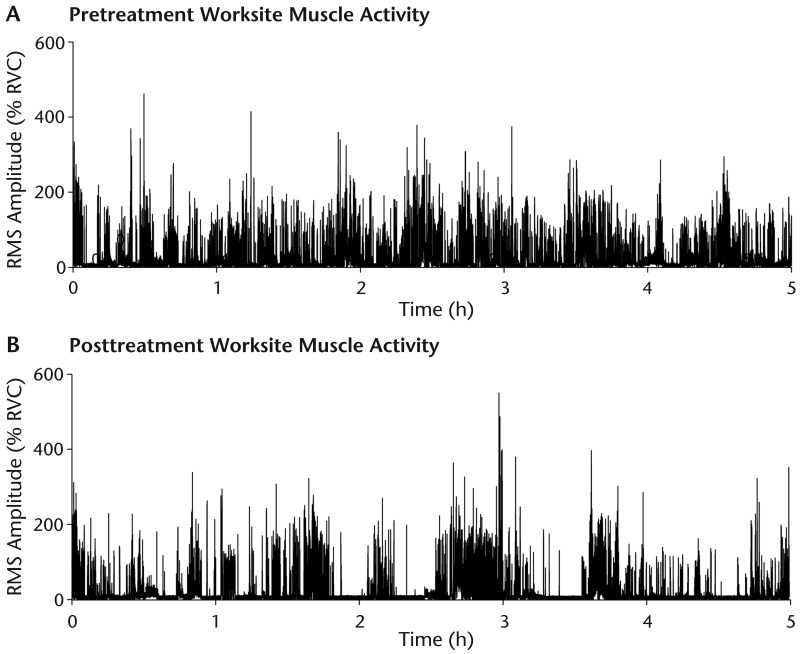
Work-site EMG recordings representative of the average change in muscle activity across recording days before and after the 8-week intervention are illustrated in Figure 4. Static muscle activity was 3.5% RVC prior to treatment and decreased to 1.7% RVC immediately after treatment (Fig. 3C). Similarly, the muscle remained at rest for 32% of the workday before treatment, which increased to 54% immediately after treatment (Fig. 3D). This trend toward an overall reduction in trapezius muscle activity was not maintained at the 3-month assessment, as values of static muscle activity and muscular rest approached those observed prior to treatment. Interestingly, the patient also reported an increase in trait anxiety and neck-related disability at the 3-month assessment compared with immediately after treatment. At the 6-month assessment, trapezius muscle activity improved to posttreatment values along with self-report measures of physical and psychological health.
Figure 4.
Habitual patterns of trapezius muscle activity in the workplace. Representative activity of the dominant upper trapezius muscle is shown for 5-hour recordings obtained during a typical workday before (A) and immediately after (B) the 8-week multidisciplinary intervention. The root mean square (RMS) amplitude of the electromyographic signal was normalized to a submaximal reference voluntary contraction and plotted as a function of time. Habitual activity of the trapezius muscle during daily work activities was visibly reduced following the intervention.
Discussion
Patients with neck pain often experience high rates of recurrence and poor long-term outcomes with conventional treatments.15,16 These findings may be attributed to the treatment of neck pain as a homogenous disorder, which likely results in suboptimal treatment for many individuals. Investigations of adjunct therapies for patients affected by chronic neck pain are needed, particularly for individuals whose symptoms are worsened by psychosocial stress. We sought to address these limitations by describing a novel screening method used to select specific components of a multimodal intervention not previously tested in patients with stress-related neck pain.
Several recent clinical trials of EMG biofeedback for the management of chronic neck pain have been conducted, with mixed results. One study showed that 6 weeks of biofeedback training produced greater reductions in cervical muscle activity, pain, and disability than either active exercise or physical modalities.7 In contrast, other clinical trials have demonstrated that reductions in neck pain and disability following 4 weeks of biofeedback training were no greater than those observed with ergonomic counseling,8 strengthening exercises,10 or conventional medical care.9 Despite finding no significant differences between treatment groups, Voerman et al8 found clinically meaningful improvements in approximately half of the patients treated with biofeedback and suggested that biofeedback may only be effective for a subgroup of patients with chronic neck pain.
This case report describes a novel EMG screening procedure that may help clinicians identify which patients respond to psychosocial stressors with elevated muscle activity. It seems plausible that this subgroup of individuals may benefit most from biofeedback interventions designed to reduce excessive muscle activity in the workplace. Although the patient in this case report was identified in a laboratory setting and the biofeedback intervention used custom-designed software that is not currently available in the clinic, the EMG screening and biofeedback protocols can easily be adapted for clinical applications using commercially available biofeedback units.7 Screening of EMG responses to simulated stressors in the clinic may allow physical therapists to better identify patients who are most likely to benefit from biofeedback, stress management, or other psychologically informed approaches to the management of chronic musculoskeletal pain. Future clinical trials comparing the response to such treatments among patient subgroups identified by EMG screening are needed to determine the efficacy of this approach.
The patient in this case report experienced improvements in neck disability, trait anxiety, and trapezius muscle activity in the workplace following an 8-week multidisciplinary intervention that combined physical therapy, biofeedback, and psychotherapy. Importantly, these improvements were maintained up to a year after treatment, with a complete resolution of neck disability 2 years later. Positive long-term outcomes were observed despite an 8-year history of chronic neck pain that was previously unresponsive to a variety of conservative interventions. We speculate that screening for stress-evoked muscle activity prior to implementing stress management techniques as an adjunct to physical therapy may have contributed to these outcomes. In contrast to previous clinical trials that delivered biofeedback in the workplace,7–10 our biofeedback intervention was administered during simulated work tasks performed in a clinical setting with verbal and manual coaching from a physical therapist to optimize muscle relaxation. Psychotherapy sessions also were included to teach the patient behavioral strategies to help manage her stress in the absence of real-time biofeedback. Our multidisciplinary approach identified both psychosocial and biomechanical stressors in the workplace and emphasized lifestyle modifications that required the patient to incorporate skills learned in the clinic into her daily work routine. These elements of the intervention may have contributed to larger and more sustained improvements than previously reported for similar patient populations.
It is important to recognize that a single patient case cannot establish cause-and-effect relationships between the intervention provided and the outcomes observed. Neck pain is an episodic disorder,2 and the patient may have experienced recurrent episodes that were not detected between standardized assessments. It is possible that the patient's symptoms might have improved over time without treatment or that improvements resulted from concurrent treatments that were not reported by the patient. It also is possible that changing employment settings a year after treatment may have contributed to the positive long-term outcomes observed in this case. Finally, cumulative muscle trauma, whether caused by biomechanical or psychosocial stress, is only one of many complex factors that may contribute to the development of chronic pain.
Although a primary goal of the stress management intervention was to reduce stress-evoked muscle activity to minimize cumulative loads on the trapezius muscle, this intervention also was intended to address the higher-order cognitive processes known to affect pain perception.35 It is not possible to determine which impairments, if any, were affected by particular components of the multimodal intervention described in this case report. Future research is necessary to determine whether stress management is an effective adjunct to standard physical therapist management of chronic neck pain, determine the mechanisms responsible for this effect, and determine the most valid screening tools for identifying patients who respond best to biopsychosocial interventions.
Footnotes
Dr Bruflat, Ms Balter, and Dr Maluf provided concept/idea/project design and project management. Dr Bruflat, Ms Balter, Dr Fethke, and Dr Maluf provided writing and data analysis. Dr Bruflat, Ms Balter, Dr McGuire, and Dr Maluf provided data collection. Dr Maluf provided fund procurement and institutional liaisons. Dr McGuire and Dr Maluf provided the patient and facilities/equipment. Dr Bruflat, Dr Fethke, and Dr Maluf provided consultation (including review of manuscript before submission).
This work was supported by a Career Development Award from the Colorado Clinical and Translational Science Institute (NIH KL2RR025779) and NIH R01AR056704 to Dr Maluf.
References
- 1. De Loose V, Burnotte F, Cagnie B, et al. Prevalence and risk factors of neck pain in military office workers. Mil Med. 2008;173:474–479 [DOI] [PubMed] [Google Scholar]
- 2. Guzman J, Hurwitz EL, Carroll LJ, et al. ; for the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. A new conceptual model of neck pain: linking onset, course, and care. Spine. 2008;33 (suppl 4): S14–S23 [DOI] [PubMed] [Google Scholar]
- 3. Cote P, van der Velde G, Cassidy JD, et al. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33 (suppl 4): S60–S74 [DOI] [PubMed] [Google Scholar]
- 4. Bongers PM, Ijmker S, van den Heuvel S, Blatter BM. Epidemiology of work related neck and upper limb problems: psychosocial and personal risk factors (part I) and effective interventions from a bio behavioural perspective (part II). J Occup Rehabil. 2006;16:279–302 [DOI] [PubMed] [Google Scholar]
- 5. Stephenson JL, Christou EA, Maluf KS. Discharge rate modulation of trapezius motor units differs for voluntary contractions and instructed muscle rest. Exp Brain Res. 2011;208:203–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lundberg U, Kadefors R, Melin B, et al. Psychophysiological stress and EMG activity of the trapezius muscle. Int J Behav Med. 1994;1:354–370 [DOI] [PubMed] [Google Scholar]
- 7. Ma C, Szeto GP, Yan T, et al. Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: a randomized controlled trial. Arch Phys Med Rehabil. 2011;92:849–858 [DOI] [PubMed] [Google Scholar]
- 8. Voerman GE, Sandsjo L, Vollenbroek-Hutten MM, et al. Effects of ambulant myofeedback training and ergonomic counselling in female computer workers with work-related neck-shoulder complaints: a randomized controlled trial. J Occup Rehabil. 2007;17:137–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sandsjo L, Larsman P, Huis in 't Veld RM, Vollenbroek-Hutten MM. Clinical evaluation of a myofeedback-based teletreatment service applied in the workplace: a randomized controlled trial. J Telemed Telecare. 2010;16:329–335 [DOI] [PubMed] [Google Scholar]
- 10. Dellve L, Ahlstrom L, Jonsson A, et al. Myofeedback training and intensive muscular strength training to decrease pain and improve work ability among female workers on long-term sick leave with neck pain: a randomized controlled trial. Int Arch Occup Environ Health. 2011;84:335–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schonstein E, Kenny D, Keating J, et al. Physical conditioning programs for workers with back and neck pain: a cochrane systematic review. Spine. 2003;28:E391–E395 [DOI] [PubMed] [Google Scholar]
- 12. Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther. 2003;8:10–20 [DOI] [PubMed] [Google Scholar]
- 13. Gross AR, Goldsmith C, Hoving JL, et al. Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007;34:1083–1102 [PubMed] [Google Scholar]
- 14. Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: noninvasive interventions—results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33 (suppl 4): S123–S152 [DOI] [PubMed] [Google Scholar]
- 15. Cote P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267–273 [DOI] [PubMed] [Google Scholar]
- 16. Carroll LJ, Hogg-Johnson S, Cote P, et al. Course and prognostic factors for neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33 (suppl 4): S93–S100 [DOI] [PubMed] [Google Scholar]
- 17. Craik RL. A convincing case—for the psychologically informed physical therapist [editorial]. Phys Ther. 2011;91:606–608 [DOI] [PubMed] [Google Scholar]
- 18. Main CJ, George SZ. Psychologically informed practice for management of low back pain: future directions in practice and research. Phys Ther. 2011;91:820–824 [DOI] [PubMed] [Google Scholar]
- 19. Wainner RS, Fritz JM, Irrgang JJ, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62 [DOI] [PubMed] [Google Scholar]
- 20. Cleland JA, Childs JD, Fritz JM, Whitman JM. Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil. 2006;87:1388–1395 [DOI] [PubMed] [Google Scholar]
- 21. Shahidi B, Johnson CL, Maluf KS. Reliability and discriminant validity of cervicothoracic impairment measures in individuals with and without chronic neck pain. J Orthop Sports Phys Ther. 2012;42:A72–A73 [Google Scholar]
- 22. Walton DM, Macdermid JC, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41:644–650 [DOI] [PubMed] [Google Scholar]
- 23. Jull GA, O'Leary SP, Falla DL. Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. J Manipulative Physiol Ther. 2008;31:525–533 [DOI] [PubMed] [Google Scholar]
- 24. Occupational Safety and Health Administration website Computer Workstation eTool. Available at: http://www.osha.gov/SLTC/etools/computerworkstations/index.html. Accessed December 9, 2008
- 25. Spielberger CD. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983 [Google Scholar]
- 26. Young BA, Walker MJ, Strunce JB, et al. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009;9:802–808 [DOI] [PubMed] [Google Scholar]
- 27. Jonsson B. Measurement and evaluation of local muscular strain in the shoulder during constrained work. J Hum Ergol. 1982;11:73–88 [PubMed] [Google Scholar]
- 28. Nordander C, Hansson GA, Asterland P, et al. Muscular rest: a measure of physical exposure. In: Proceedings of the 13th Triennial Congress of the International Ergonomic Association. Toronto, Ontario, Canada: International Ergonomic Association; 1997;4:207–209 [Google Scholar]
- 29. Mork PJ, Westgaard RH. Long-term electromyographic activity in upper trapezius and low back muscles of women with moderate physical activity. J Appl Physiol. 2005;99:570–578 [DOI] [PubMed] [Google Scholar]
- 30. Ezzo J, Haraldsson BG, Gross AR, et al. Massage for mechanical neck disorders: a systematic review. Spine. 2007;32:353–362 [DOI] [PubMed] [Google Scholar]
- 31. Lynch SS, Thigpen CA, Mihalik JP, et al. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med. 2010;44:376–381 [DOI] [PubMed] [Google Scholar]
- 32. Lee K, Swanson N, Sauter S, et al. A review of physical exercises recommended for VDT operators. Appl Ergon. 1992;23:387–408 [DOI] [PubMed] [Google Scholar]
- 33. Falla D, Jull G, Hodges P. Training the cervical muscles with prescribed motor tasks does not change muscle activation during a functional activity. Man Ther. 2008;13:507–512 [DOI] [PubMed] [Google Scholar]
- 34. Veehof MM, Oskam MJ, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain. 2011;152:533–542 [DOI] [PubMed] [Google Scholar]
- 35. Linton SJ, Shaw WS. Impact of psychological factors in the experience of pain. Phys Ther. 2011;91:700–711 [DOI] [PubMed] [Google Scholar]