Abstract
Purpose
The current study describes how the excess mortality risk associated with depression translates into specific causes of death occurring during a 40-year follow-up period, with focus on deaths related to injuries, cardiovascular diseases, and cancer.
Methods
Data comes from a cross-sectional survey (Community Mental Health Epidemiology Study) conducted in the early 1970s in Washington County, Maryland. Random sampling for the survey resulted in 2762 interviews. For the current analyses, baseline depressed mood was linked to current participant vital status through the use of death certificate records.
Results
The relative subdistribution hazards for cardiovascular deaths (3.08 (1.74–5.45)) and fatal injuries (4.63 (1.76–12.18)) were significant over the entire 40-year period for young adults (18–39 years old at baseline). The relative subdistribution hazard for cardiovascular deaths during the first 15 years of follow-up was pronounced in elderly (≥ 65 years) males (2.99 (1.67–5.37)). There were no significant associations between depressed mood and cancer deaths.
Conclusions
Individuals in the general community with depressed mood may be at increased risk of deaths due to cardiovascular disease and injury, even several decades after exposure assessment. Young adults with depressed mood appear to be particularly vulnerable to these associations.
MeSH Headings: Depression, depressive symptoms, death, mortality, cardiovascular diseases, wounds and injury
Introduction
The association between depression and elevated total mortality risk in the general community is becoming established. A 2002 meta-analysis of 25 community studies placed the overall relative risk estimate at 1.81 (95% CI: 1.58–2.07) (1). Few studies in the general community have simultaneously addressed total mortality assessments with broad cause of death assessments.
Prior studies have often focused on the association between depression and the development of specific diseases and survival from that same disease. A consistent finding in prior literature has been the association between depression and the development and progression of cardiovascular disease in otherwise healthy individuals (2–6). Some studies have also indicated an association between depression and increased cardiovascular mortality in populations with pre-existing disease (7).
The association between depression and the development of cancer is less established. Findings have indicated an increased risk (8) in the absence of smoking, increased risk only in the presence of smoking (9, 10) or lack of any major evidence (11–13). Some studies have linked depressive symptoms to survival from liver cancer (14), breast cancer (15) and multiple tissue sites (16, 17). Broader assessments of depressive symptoms and psychological coping mechanisms have found no association with survival from cancer (18).
Findings are mixed, but potential associations with fatal injuries beyond the association with suicide may exist. Participants with depression in general community populations have been found to be at increased risk of falls (19, 20), becoming a homicide victim (21), motor vehicle accidents (22), and non-suicidal self-injurious behavior (23, 24). More extensive injury research has been performed in older adult populations where evidence of an association is more lacking. Findings have suggested that depression in unrelated to fracture risks (25), motor vehicle collisions (26), or injury severity (27) in older adults.
Studies also suggest that the major causes of death are similar between individuals with and without depression. Cardiovascular disease, respiratory disease, and cancer formed the majority of deaths in a Dutch population comprised of older adults aged 55–85 years, regardless of depression status (28). Similar findings were reported in a study of participants 25 years and older in the United States (29). Although injury deaths were reported in these prior studies, they constituted only a small proportion of the total mortality in both exposure groups.
The association between depression and excess risk of death does not appear to be readily explained by one cause of death. General community studies have indicated depression may be simultaneously linked to excess risk of death across a variety of causes. A study of the elderly in Japan over a 15-year follow-up period found associations between baseline depression and excess mortality risk due to cerebrovascular diseases, cancer, respiratory disorders, and suicide (30). A study of middle-aged adults in the Netherlands also found associations with multiple causes of death including cardiovascular disease, cancer, and accidents during an approximate 5-year follow-up interval (31).
Given studies involving older adults predominate the field, whether depression in young adulthood can be linked to specific causes of death throughout the life span remains underexplored. The current study examines causes of death associated with depressed mood in a general community study from Washington County, Maryland, involving a 40-year follow-up period. The four-decade period allows tracking of cause-specific mortality risk through the entire adult life course for young adults at baseline. The current study examines whether expanding the public health burden of depression is warranted given its potential impact on the mortality experience of young adults in the general community.
Methods
Study population overview
Data for this study comes from the revival of a cross-sectional survey (Community Mental Health Epidemiology Study (CMHE)) conducted in the early 1970s in Washington County, Maryland (32). The purpose of the CMHE was to characterize mood symptomatology in the general population. Interviewing began in December 1971 and continued until July 1974.
Sampling for the CMHE occurred through a 98% complete household roster from a private county census conducted in 1963 (33). Households were randomly selected from the listing and samples were stratified by geographic location and socioeconomic status. One individual in each selected household ≥18 years was then randomly selected for interview. The sampling resulted in 2762 interviews forming a 78% response rate.
Exposure measurement: depressed mood
The CMHE contained the first use of the CES-D Scale (32, 34). A score ≥16 was used in this analysis to indicate the presence of depressed mood. This cut-off point was developed from CMHE data (32).
Outcome measurement: mortality linkage
Baseline depressive symptoms from the cross-sectional CMHE study were linked to mortality status over 40 years through the use of three main mortality sources. First, Washington County death certificates were searched for deaths occurring 1972–2011. Second, participants who were not found deceased using county records were then submitted to the National Death Index. NDI records were searched for deaths occurring 1979–2008 (all available NDI dates). Third, the Social Security Death Index (SSDI) was used to locate evidence of death for recent participant deaths (deaths occurring March 2011–August 2011). Participants for whom no death record was located using the three sources were then assumed to be alive as of August 1, 2011. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved the mortality linkage and related analyses.
Outcome measurement: cause of death determination
All cause of death information came from the underlying cause of death listed on the death certificate. Complete cause of death information was available on 1477 (95.5%) of all participants determined to be deceased. Cause of death information was available as a single International Classification of Disease (ICD) code for the underlying cause of death. The obtained ICD codes were from the Eighth (35), Ninth (36), and Tenth (37) Revisions of the ICD.
Broad categories were created to reflect related causes of death (i.e. cardiovascular disease (diseases of the heart, cerebrovascular diseases, essential hypertension and hypertensive renal diseases), cancer (any malignant neoplasm), and fatal injuries (accidents (unintentional injuries), intentional self-harm (suicide), and assault (homicide)) based on U.S. National Vital Statistics Reports (38). All other causes of death besides cardiovascular, cancer, and fatal injuries were categorized as “other causes of death”.
Covariate assessment
Baseline age in years and sex were the main covariates of interest for this study. Baseline smoking status (ever versus never), years of education (categorized as at least high school or less than high school), and healthy body weight (measured by body mass index categories with 18.5–24.9 representing the healthy BMI range using baseline self-reported weight and height) were also included in regression models.
Analysis
Cause-specific Cox Proportional Hazards models were created using each major cause of death category as the outcome. Due to the presence of competing risks in this analysis, an alternative measure of risk was also used: the subdistribution cumulative incidence function (39). Other causes of death not associated with the cause of death category of interest were identified as competing risks for this study. The calculated functions were also used to create stacked cumulative incidence plots. The plots display how the total probability of one is allocated between all competing risks, including the possibility of surviving through the end of follow-up.
All models used follow-up time (time since interview) as the time axis. The hazards were determined to lack proportionality across the full 40 year follow-up time period based on the examination of Schoenfeld residuals and log-log plots. Follow-up time was stratified into three periods: 0–14.99 years, 15–29.99 years, and 30–40 years. The sample was stratified by sex and three main baseline age ranges: young adult (18–39 years), middle-aged (40–64), and elderly (≥65) according to hypotheses related to sex and age interactions. Sensitivity analyses were conducted by removing participants who died during the first 5 years of follow-up time from the at-risk population to exclude individuals who may have been physically ill at baseline. All analyses were performed in Stata v.11 (40).
Results
Table 1 displays the main characteristics and cause of death information for the population. The study population comprised the entire adult age span (18–95 years) with middle-aged adults (40–64 years) forming the largest age group (43.1%). The study population was almost exclusively white, Caucasian race (97.8%).
Table 1.
Baseline characteristics and main causes of death for all participants, stratified by baseline depressed mood status
| Total 2,762 |
Depressed mood1 n=467 (16.9%) |
No depressed mood n=2,279 (82.5%) |
Comparison: P value |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | Category | |||||||
| n | % | n | % | n | % | |||
| Age | Mean (SD) | 46.69 (17.37) | 42.56 (17.38) | 47.45 (17.25) | <.001 | |||
| Age group | 18–39 | 1,101 | 39.9 | 231 | 49.5 | 869 | 38.1 | <.001 |
| 40–64 | 1,190 | 43.1 | 178 | 38.1 | 1,003 | 44.0 | ||
| ≥ 65 | 471 | 17.1 | 58 | 12.4 | 407 | 17.9 | ||
| Sex | Female | 1,607 | 58.3 | 329 | 70.5 | 1,267 | 55.6 | <.001 |
| Male | 1,154 | 41.8 | 137 | 29.3 | 1,012 | 44.4 | ||
| Deaths | All cause | 1547 | 56.0 | 244 | 52.3 | 1290 | 56.6 | .08 |
| Cardiovascular2 | 726 | 26.3 | 112 | 24.0 | 355 | 26.7 | .23 | |
| Cancer3 | 327 | 11.8 | 50 | 10.7 | 273 | 12.0 | .44 | |
| Injury4 | 56 | 2.0 | 10 | 2.1 | 45 | 2.0 | .82 | |
| All other causes | 438 | 15.9 | 72 | 15.4 | 364 | 16.0 | .77 | |
Depressed mood measured as Center for Epidemiologic Studies Depression scale (CES-D) score ≥16; CES-D score missing for 16 (.58%) participants
Cardiovascular= Diseases of the heart, cerebrovascular diseases, essential hypertensive renal disease
Cancer= Any malignant neoplasm
Injury= Unintentional injuries, suicides, and homicides
A total of 467 (16.9%) participants had depressed mood at baseline (CES-D score ≥16). Participants with depressed mood were mainly female and younger than participants without depressed mood. Prevalence of depressed mood decreased with age. Only 12.5% of elderly participants displayed elevated symptoms compared to 21.0% of young adults and 15.1% of middle-aged adults.
The majority of the cohort (56.0%, n=1546) was determined deceased by the end of follow-up. There were no statistically significant differences for major causes of death between participants with and without depressed mood. Cardiovascular disease and cancer were the leading causes of death for both populations. Few participants died from fatal injuries in either group. Twelve suicide deaths occurred in this study population and all were in male participants. Ten suicide deaths occurred among participants without elevated depressive symptoms at baseline.
Relative hazards for specific causes of death for all participants are shown in Table 2. The cardiovascular risk estimate (1.30 (1.05–1.60) – subdistribution hazard ratio) was statistically significant. Removal of deaths occurring in the first 5 years of follow-up time had no major impact on the risk estimate (1.36 (1.08–1.71)). The association between depressed mood and fatal injuries was pronounced during the first 15 years of follow-up (2.50 (1.03–6.02)) and then null afterwards. All associations with cancer deaths were consistently null.
Table 2.
Hazard ratios for the association between depressed mood and cause-specific mortality, stratified by cause of death and follow-up time period in years for all participants
| Follow- up time |
Cause of death |
Number of deaths (% of all-cause deaths) |
Subdistribution hazard ratio: Age/sex adjustment4 |
Cause-specific hazard ratio: Age/sex adjustment4 |
||||
|---|---|---|---|---|---|---|---|---|
| Total | Depressed mood |
No depressed mood |
Point estimate |
95% CI | Point estimate |
95% CI | ||
| 0–15 | CVD1 | 333(56.5) | 51(52.6) | 282(58.1) | 1.54 | 1.15–2.00 | 1.56 | 1.15–2.11 |
| Injury2 | 24(4.1) | 7(7.2) | 17(3.5) | 2.50 | 1.03–6.02 | 2.67 | 1.08–6.58 | |
| Cancer3 | 124(21.1) | 16(16.5) | 108(22.3) | 1.18 | .69–1.79 | 1.08 | .63–1.84 | |
| 15–30 | CVD | 285(43.7) | 45(45.9) | 240(43.8) | 1.37 | .99–1.91 | 1.40 | 1.01–1.94 |
| Injury | 23(3.5) | 2(2.0) | 21(3.8) | .78 | .19–3.16 | .80 | .18–3.47 | |
| Cancer | 142(21.8) | 22(22.4) | 120(21.9) | 1.11 | .69–1.79 | 1.17 | .74–1.85 | |
| 30–40 | CVD | 101(33.1) | 16(32.7) | 85(33.2) | 1.22 | .71–2.09 | 1.34 | .77–2.31 |
| Injury | 8(2.6) | 1(2.0) | 7(2.7) | 1.44 | .23–8.87 | .87 | .11–7.29 | |
| Cancer | 57(18.7) | 12(24.5) | 45(12.6) | 1.10 | .34–3.57 | 1.64 | .85–3.15 | |
| All years | CVD | 720(46.6) | 112(45.9) | 608(47.2) | 1.30 | 1.05–1.60 | 1.46 | 1.19–1.80 |
| Injury | 55(3.6) | 10(4.1) | 45(3.5) | 1.34 | .68–2.63 | 1.55 | .77–3.11 | |
| Cancer | 323(20.9) | 50(20.5) | 273(21.2) | .79 | .39–1.58 | 1.22 | .90–1.66 | |
Cardiovascular= Diseases of the heart, cerebrovascular diseases, essential hypertensive renal disease
I Injury= Unintentional injuries, suicides, and homicides
Cancer= Any malignant neoplasm
Full adjustment (age, sex, smoking, education, and body weight) did not alter significant findings
Relative hazards for participants aged 18–39 years at baseline are displayed in Table 3. The relative hazards for cardiovascular deaths (3.08 (1.74–5.45)) and fatal injuries (4.63 (1.76–12.18) were significant over the entire 40-year period. Removal of deaths occurring in the first 5 years of follow-up strengthened the association with fatal injuries (5.22 (1.89–14.45)). The risk estimate for cardiovascular deaths did not change.
Table 3.
Hazard ratios for the association between depressed mood and cause-specific mortality, stratified by cause of death and follow-up time period in years for participants 18–39 years
| Follow- up time |
Cause of death |
Number of deaths (% of all-cause deaths) |
Subdistribution hazard ratio: Age/sex adjustment4 |
Cause-specific hazard ratio: Age/sex adjustment4 |
||||
|---|---|---|---|---|---|---|---|---|
| Total | Depressed mood |
No depressed mood |
Point estimate |
95% CI | Point estimate |
95% CI | ||
| 0–15 | CVD1 | 8(26.1) | 4(36.4) | 4(21.1) | 5.38 | 1.66–17.47 | 5.60 | 1.37–22.86 |
| Injury2 | 8(26.7) | 5(45.5) | 3(15.8) | 8.65 | 2.05–36.45 | 8.66 | 2.01–37.43 | |
| Cancer3 | 6(20.0) | 2(18.2) | 4(21.1) | 2.02 | .36–11.26 | 2.07 | .37–11.71 | |
| 15–30 | CVD | 22(29.7) | 7(36.8) | 15(27.3) | 2.53 | 1.05–6.11 | 2.53 | 1.02–6.28 |
| Injury | 2(2.7) | 1(5.3) | 1(1.8) | Not calculated5 | Not calculated5 | |||
| Cancer | 29(39.2) | 7(36.8) | 22(40.0) | 1.46 | .59–3.60 | 1.46 | .62–3.45 | |
| 30–40 | CVD | 20(25.3) | 7(31.8) | 13(22.8) | 3.28 | 1.79–8.35 | 3.37 | 1.32–8.59 |
| Injury | 5(6.3) | 1(4.5) | 4(7.6) | 1.44 | .23–8.87 | 1.54 | .17–14.37 | |
| Cancer | 22(27.8) | 4(18.2) | 18(31.6) | 1.10 | .34–3.57 | 1.17 | .39–3.52 | |
| All years | CVD | 50(27.3) | 18(34.6) | 32(24.4) | 3.08 | 1.74–5.45 | 3.26 | 1.81–5.86 |
| Injury | 15(8.2) | 7(13.5) | 8(6.1) | 4.63 | 1.76–12.18 | 4.80 | 1.70–13.57 | |
| Cancer | 57(31.1) | 13(25.0) | 44(33.6) | 1.30 | .67–2.53 | 1.41 | .75–2.64 | |
Cardiovascular= Diseases of the heart, cerebrovascular diseases, essential hypertensive renal disease
Injury= Unintentional injuries, suicides, and homicides
Cancer= Any malignant neoplasm
Full adjustment (age, sex, smoking, education, and body weight) did not alter significant findings
Estimates not calculated due to insufficient number of deaths
The association between depressed mood and fatal injuries was confined to the first 15 years of follow-up (8.65 (2.05–36.45)). The high risk of fatal injuries within the early follow-up time period was linked to deaths among males with depressed mood. Three deaths total occurred in this group; all were related to fatal injuries: motor vehicle accident, suicide, and homicide.
The association between depressed mood and elevated cardiovascular death risk was linked to deaths in females. Relative hazards could not be calculated for young adult females during the immediate follow-up time period since no cardiovascular deaths occurred in females without depressed mood; 4 cardiovascular deaths occurred in females with depressed mood out of 8 deaths total. During the last 10 years of follow-up, 50.0% of deaths among females with depressed mood were cardiovascular-related versus 13.6% of deaths in females without depressed mood. This resulted in a relative subdistribution relative hazard of 6.18 (1.39–27.46).
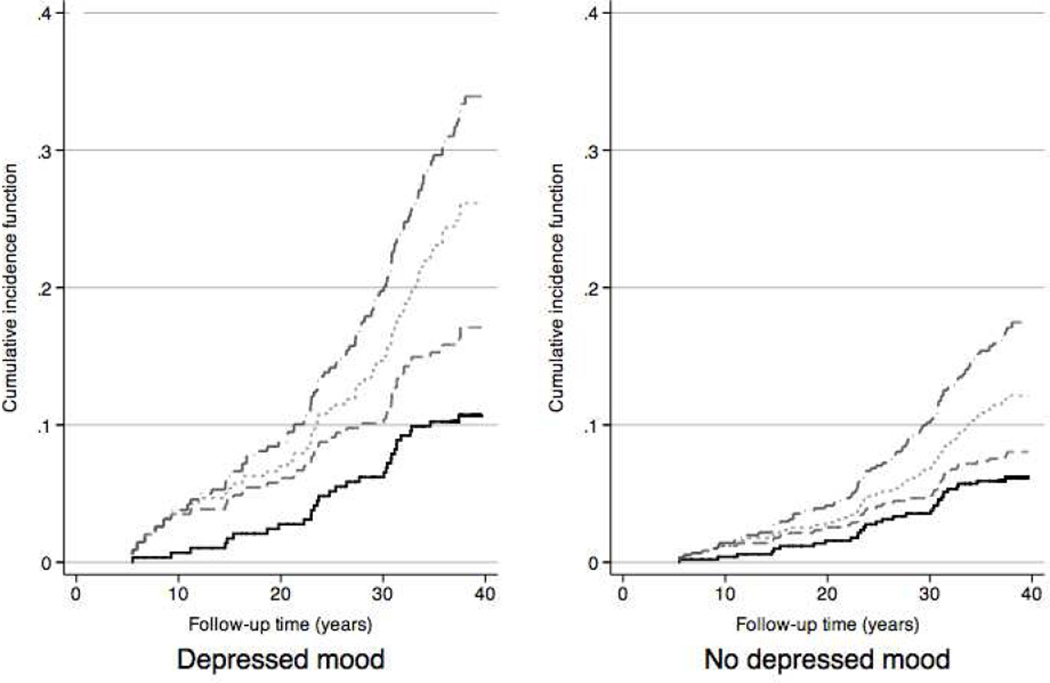
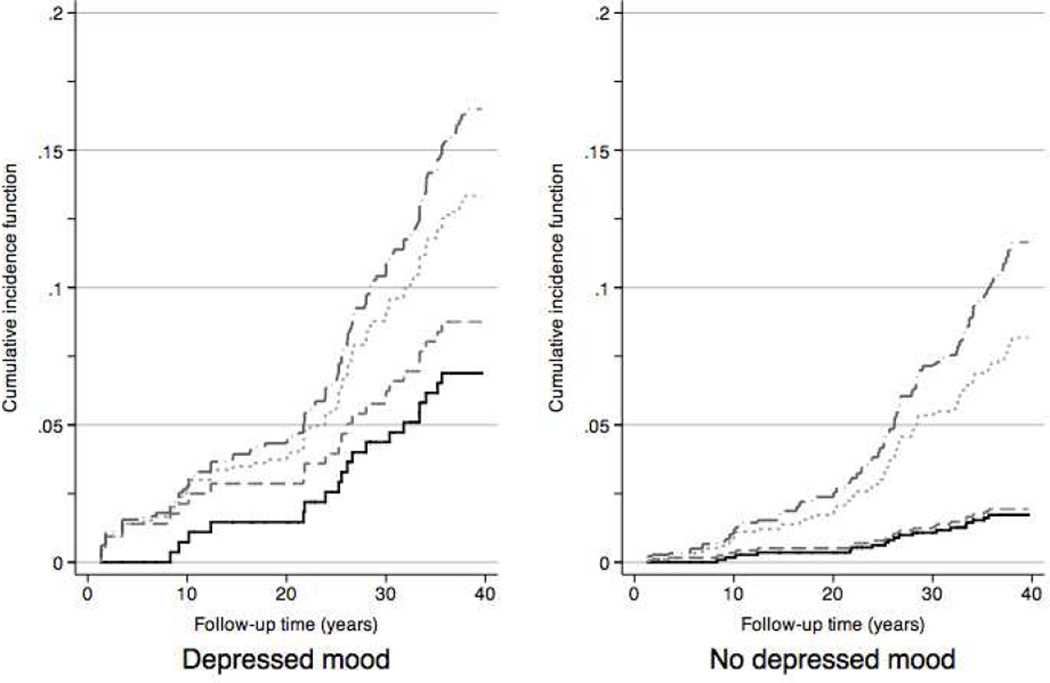
The differences between young adults with and without depressed mood can are further highlighted in Figures 1 and 2. Young adult males (Figure 1) with depressed mood displayed higher total mortality (36.2% vs. 18.8%, P <.001). The stacked cumulative incidence functions for the 4 main cause of death categories appeared similar between males with and without depressed mood. The reverse can be seen for females (Figure 2). Females with depressed mood did not display significantly higher total mortality (16.8% vs. 11.9%, P= 0.12), but higher cumulative incidence functions for cardiovascular and injury mortality.
Figure 1.
Stacked cumulative incidence plots for specific causes of death, males 18–39 years old at baseline
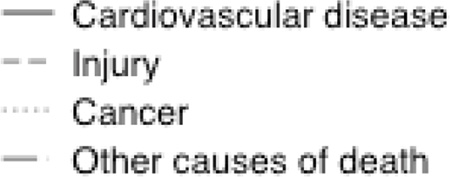
Figure 2.
Stacked cumulative incidence plots for specific causes of death, females 18–39 years old at baseline
The most noticeable difference among middle-aged participants was the lack of fatal injuries among those with depressed mood. Only one fatal injury occurred among middle-aged participants with depressed mood. The death (a motor vehicle accident) occurred in a female. Twenty fatal injuries occurred in middle-aged males without depressed mood. Five of these deaths (25%) were due to suicide and seven (35%) were related to accidental falls. There were no sustained significant associations between cardiovascular or cancer deaths and depressed mood for middle-aged participants over the full 40-year follow-up period.
Significant findings for the elderly age group were limited to the 0–15 year follow-up period. Elevated estimates for both cardiovascular and injury deaths were calculated, but only cardiovascular remained statistically significant (1.75 (1.20–2.56)). As very few participants survived to the last stage of follow-up, reliable risk estimates could not be calculated. Associations with cancer deaths remained null.
The cardiovascular association was linked to males in this age group. During the first 15 years of follow-up, 91.7% of all deaths among males with depressed mood were cardiovascular related, resulting in an associated relative subdistribution hazard of 2.99 (1.67–5.37).
Discussion
Findings from this study involving a 40-year follow-up period, suggest persistent associations between depressed mood and cause-specific mortality that differ by sex, age group, and proximity to baseline. Even several decades after baseline, young adult females with depressed mood remained at excess risk of death from cardiovascular disease. Young adult males with depressed mood were at excess risk of fatal injury in time periods closer to baseline.
Our findings confirm those from other community-based studies (28, 29, 41, 42): the total mortality associated with depression in the general community is driven by common causes of death. Individuals with depressed mood in this study died from the same diseases as individuals without depressed mood: mainly cardiovascular disorders and cancer. Our findings confirm previously reported findings that the excess mortality risk associated with depression is not explained by excess suicide deaths (28).
The majority of suicide deaths in this study occurred among individuals without depressed mood, a previously reported finding (31). Fatal injuries were important causes of death among middle-aged males without depressed mood. Fatal injuries were the only causes of death for young adult males with depressed mood during the first twenty years of follow-up. Other studies have indicated that deaths related to hazardous behaviors often occur before middle-age for many males experiencing depression (43–45). The middle-aged males with depressed mood in this study may have represented the lower end of the fatal injury risk spectrum; the highest end population may have been deceased by study entry.
The association between depression and excess risk of cardiovascular death has been a common finding of studies involving older adults (46–49). The current study allowed identification of another distinct group who experienced similar excess risk: young adult females. Young adult females with depressed mood may have experienced cardiovascular mortality on a completely different trajectory as the elderly males with depressed mood in this population. Emergence of depression in young adulthood is believed to have a strong genetic basis versus a direct link to pre-existing illness (50). The genetic link to depression may be associated with future development of cardiovascular disease (51, 52). Recent analyses of NHANES III have also suggested young adult females with depression may be at excess risk of premature cardiovascular related death over a 15-year follow-up period (53). Results from this current study augment these findings by indicating this excess risk may extend into late adulthood for females experiencing depression as young adults.
The null findings related to cancer deaths are consistent with many studies (11–13, 54). A prior study in this population (10) with more limited follow-up did indicate an association between depressed mood and respiratory-related cancers in the presence of smoking. The current analysis was not site-specific. Furthermore, depressed mood was only associated with smoking in the young adult population. Given that the average age of lung cancer death is 72 years (55), more follow-up time may be needed to fully evaluate whether depressed mood is associated with certain site-specific cancers.
Data are limited regarding the presence of pre-existing illnesses among study participants. Data were collected on whether individuals dying very early in follow-up (e.g. <5 years) were ill at the time of interview. Individuals with depressed mood were less likely to have evidence of prior illness. Whether individuals dying in later time periods were physically ill at baseline remains unknown. The young adult females with depressed mood who died 30–40 years after baseline most likely did not have active, cardiovascular disease at baseline.
The accuracy of death certificate information has been questioned for decades. Studies have indicated the overrepresentation of circulatory disorders (56) and the blurred line between intentional and unintentional injuries (57). The use of a broader injury category better captured misclassification between unintentional and intentional injury. Studies also suggest that misclassification along a spectrum of disease like cardiovascular disease is more common than misclassification between separate major disease categories (56).
Depression is now considered to be the leading cause of disability in the world (58). Understanding of how depression contributes to mortality is obscured though. General community studies should continue exploring total mortality risk with consideration how cause-specific risks may differ. Depression is a serious, common illness often emerging early in adulthood. The expectation that depression has a wide influence on mortality should be agreed upon today.
Acknowledgments
The project described was supported by Grant Number T32 HL07024 from the National Heart, Lung, and Blood Institute. Additional funding was provided by the Department of Epidemiology Doctoral Thesis Research Fund and the George W. Comstock Center for Public Health Research and Prevention. The authors thank Judy Hoffman-Bolton for her assistance with the mortality linkage.
Abbreviations and acronyms
- CES-D
Center for Epidemiologic Studies Depression scale
- CI
Confidence interval
- CMHE
Community Mental Health Epidemiology Program study
- ICD
International Classification of Disease
- NDI
National Death Index
- SSDI
Social Security Death Index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72:227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 2.Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med. 1998;158:1422–1426. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 3.Marzari C, Maggi S, Manzato E, Destro C, Noale M, Bianchi D, et al. Depressive symptoms and development of coronary heart disease events: the Italian longitudinal study on aging. J Gerontol A Biol Sci Med Sci. 2005;60:85–92. doi: 10.1093/gerona/60.1.85. [DOI] [PubMed] [Google Scholar]
- 4.Rowan PJ, Haas D, Campbell JA, Maclean DR, Davidson KW. Depressive symptoms have an independent, gradient risk for coronary heart disease incidence in a random, population-based sample. Ann Epidemiol. 2005;15:316–320. doi: 10.1016/j.annepidem.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Wulsin LR, Singal BM. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom Med. 2003;65:201–210. doi: 10.1097/01.psy.0000058371.50240.e3. [DOI] [PubMed] [Google Scholar]
- 6.Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, Cochrane B, et al. Depression and cardiovascular sequelae in postmenopausal women. The Women's Health Initiative (WHI) Arch Intern Med. 2004;164:289–298. doi: 10.1001/archinte.164.3.289. [DOI] [PubMed] [Google Scholar]
- 7.Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33:203–216. doi: 10.1016/j.genhosppsych.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Penninx BW, Guralnik JM, Pahor M, Ferrucci L, Cerhan JR, Wallace RB, et al. Chronically depressed mood and cancer risk in older persons. J Natl Cancer Inst. 1998;90:1888–1893. doi: 10.1093/jnci/90.24.1888. [DOI] [PubMed] [Google Scholar]
- 9.Knekt P, Raitasalo R, Heliovaara M, Lehtinen V, Pukkala E, Teppo L, et al. Elevated lung cancer risk among persons with depressed mood. Am J Epidemiol. 1996;144:1096–1103. doi: 10.1093/oxfordjournals.aje.a008887. [DOI] [PubMed] [Google Scholar]
- 10.Linkins RW, Comstock GW. Depressed mood and development of cancer. Am J Epidemiol. 1990;132:962–972. doi: 10.1093/oxfordjournals.aje.a115739. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan GA, Reynolds P. Depression and cancer mortality and morbidity: prospective evidence from the Alameda County study. J Behav Med. 1988;11:1–13. doi: 10.1007/BF00846165. [DOI] [PubMed] [Google Scholar]
- 12.McGee R, Williams S, Elwood M. Depression and the development of cancer: a meta-analysis. Soc Sci Med. 1994;38:187–192. doi: 10.1016/0277-9536(94)90314-x. [DOI] [PubMed] [Google Scholar]
- 13.Zonderman AB, Costa PT, Jr, McCrae RR. Depression as a risk for cancer morbidity and mortality in a nationally representative sample. JAMA. 1989;262:1191–1195. [PubMed] [Google Scholar]
- 14.Steel JL, Geller DA, Gamblin TC, Olek MC, Carr BI. Depression, immunity, and survival in patients with hepatobiliary carcinoma. J Clin Oncol. 2007;25:2397–2405. doi: 10.1200/JCO.2006.06.4592. [DOI] [PubMed] [Google Scholar]
- 15.Goodwin JS, Zhang DD, Ostir GV. Effect of depression on diagnosis, treatment, and survival of older women with breast cancer. J Am Geriatr Soc. 2004;52:106–111. doi: 10.1111/j.1532-5415.2004.52018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dalton SO, Steding-Jessen M, Gislum M, Frederiksen K, Engholm G, Schuz J. Social inequality and incidence of and survival from cancer in a population-based study in Denmark, 1994–2003: Background, aims, material and methods. Eur J Cancer. 2008;44:1938–1949. doi: 10.1016/j.ejca.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 17.Stommel M, Kurtz ME, Kurtz JC, Given CW, Given BA. A longitudinal analysis of the course of depressive symptomatology in geriatric patients with cancer of the breast, colon, lung, or prostate. Health Psychol. 2004;23:564–573. doi: 10.1037/0278-6133.23.6.564. [DOI] [PubMed] [Google Scholar]
- 18.Petticrew M, Bell R, Hunter D. Influence of psychological coping on survival and recurrence in people with cancer: systematic review. BMJ. 2002;325:1066. doi: 10.1136/bmj.325.7372.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nordstrom DL, Zwerling C, Stromquist AM, Burmeister LF, Merchant JA. Epidemiology of unintentional adult injury in a rural population. J Trauma. 2001;51:758–766. doi: 10.1097/00005373-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Wan JJ, Morabito DJ, Khaw L, Knudson MM, Dicker RA. Mental illness as an independent risk factor for unintentional injury and injury recidivism. J Trauma. 2006;61:1299–1304. doi: 10.1097/01.ta.0000240460.35245.1a. [DOI] [PubMed] [Google Scholar]
- 21.Cascardi M, Langhinrichsen J, Vivian D. Marital aggression. Impact, injury, and health correlates for husbands and wives. Arch Intern Med. 1992;152:1178–1184. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- 22.Marcelli D, Ingrand P, Delamour M, Ingrand I. Accidents in a population of 350 adolescents and young adults: circumstances, risk factors and prediction of recurrence. Bull Acad Natl Med. 2010;194:953–964. discussion 965-957. [PubMed] [Google Scholar]
- 23.Cwik MF, Barlow A, Tingey L, Larzelere-Hinton F, Goklish N, Walkup JT. Nonsuicidal self-injury in an american Indian reservation community: results from the white mountain apache surveillance system, 2007–2008. J Am Acad Child Adolesc Psychiatry. 2011;50:860–869. doi: 10.1016/j.jaac.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O'Grady KE. Longitudinal predictors of past-year non-suicidal self-injury and motives among college students. Psychol Med. 2011:1–10. doi: 10.1017/S0033291711001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whitson HE, Sanders L, Pieper CF, Gold DT, Papaioannou A, Richards JB, et al. Depressive symptomatology and fracture risk in community-dwelling older men and women. Aging Clin Exp Res. 2008;20:585–592. doi: 10.1007/bf03324888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koepsell TD, Wolf ME, McCloskey L, Buchner DM, Louie D, Wagner EH, et al. Medical conditions and motor vehicle collision injuries in older adults. J Am Geriatr Soc. 1994;42:695–700. doi: 10.1111/j.1532-5415.1994.tb06526.x. [DOI] [PubMed] [Google Scholar]
- 27.Scaf-Klomp W, Sanderman R, Ormel J, Kempen GI. Depression in older people after fall-related injuries: a prospective study. Age Ageing. 2003;32:88–94. doi: 10.1093/ageing/32.1.88. [DOI] [PubMed] [Google Scholar]
- 28.Penninx BWJH, Geerlings SW, Deeg DJH. Minor and major depression and the risk of death in older persons. Primary Care Companion to the Journal of Clinical Psychiatry. 1999;1:196. doi: 10.1001/archpsyc.56.10.889. [DOI] [PubMed] [Google Scholar]
- 29.Zheng D, Macera CA, Croft JB, Giles WH, Davis D, Scott WK. Major depression and all-cause mortality among white adults in the United States. Ann Epidemiol. 1997;7:213–218. doi: 10.1016/s1047-2797(97)00014-8. [DOI] [PubMed] [Google Scholar]
- 30.Kawamura T, Shioiri T, Takahashi K, Ozdemir V, Someya T. Survival rate and causes of mortality in the elderly with depression: A 15-year prospective study of a Japanese community sample, the Matsunoyama-Niigata Suicide Prevention Project. J Investig Med. 2007;55:106–114. doi: 10.2310/6650.2007.06040. [DOI] [PubMed] [Google Scholar]
- 31.Mykletun A, Bjerkeset O, Dewey M, Prince M, Overland S, Stewart R. Anxiety, depression, and cause-specific mortality: the HUNT study. Psychosom Med. 2007;69:323–331. doi: 10.1097/PSY.0b013e31803cb862. [DOI] [PubMed] [Google Scholar]
- 32.Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychol Med. 1976;6:551–563. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- 33.Comstock GW, Helsing KJ. Characteristics of respondents and nonrespondents to a questionnaire for estimating community mood. Am J Epidemiol. 1973;97:233–239. doi: 10.1093/oxfordjournals.aje.a121504. [DOI] [PubMed] [Google Scholar]
- 34.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 35.WHO. International Statistical Classification of Diseases, Injuries, and Causes of Death. Sixth Revision. Geneva: 1965. [Google Scholar]
- 36.WHO. International Statistical Classification of Diseases, Injuries, and Causes of Death. Ninth Revision. Geneva: 1979. [Google Scholar]
- 37.WHO. International Statistical Classification of Diseases, Injuries, and Causes of Death. Tenth Revision. Geneva: 1992. [Google Scholar]
- 38.Deaths: Leading Causes for 2007. Natl Vital Stat Rep. 2011:1–95. [PubMed] [Google Scholar]
- 39.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 1999;94 doi: 10.1080/01621459.2017.1401540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 41.Ensinck KTJL, Schuurman AG, Van den Akker M, Metsemakers JFM, Kester ADM, Knottnerus JA, et al. Is there an increased risk of dying after depression? Am J Epidemiol. 2002;156:1043–1048. doi: 10.1093/aje/kwf148. [DOI] [PubMed] [Google Scholar]
- 42.Pulska T, Pahkala K, Laippala P, Kivela SL. Survival of elderly Finns suffering from dysthymic disorder: A community study. Soc Psychiatry Psychiatr Epidemiol. 1998;33:319–325. doi: 10.1007/s001270050061. [DOI] [PubMed] [Google Scholar]
- 43.Sanford C, Marshall SW, Martin SL, Coyne-Beasley T, Waller AE, Cook PJ, et al. Deaths from violence in North Carolina, 2004: how deaths differ in females and males. Inj Prev. 2006;12(Suppl 2):ii10–ii16. doi: 10.1136/ip.2006.012617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shen X, Hackworth J, McCabe H, Lovett L, Aumage J, O'Neil J, et al. Characteristics of suicide from 1998–2001 in metropolitan area. Death Stud. 2006;30:859–871. doi: 10.1080/07481180600853074. [DOI] [PubMed] [Google Scholar]
- 45.Skogman K, Alsen M, Ojehagen A. Sex differences in risk factors for suicide after attempted suicide-a follow-up study of 1052 suicide attempters. Soc Psychiatry Psychiatr Epidemiol. 2004;39:113–120. doi: 10.1007/s00127-004-0709-9. [DOI] [PubMed] [Google Scholar]
- 46.Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, Cochrane B, et al. Depression and Cardiovascular Sequelae in Postmenopausal Women: The Women's Health Initiative (WHI) Arch Intern Med. 2004;164:289–298. doi: 10.1001/archinte.164.3.289. [DOI] [PubMed] [Google Scholar]
- 47.Vinkers DJ, Stek ML, Gussekloo J, van der Mast RC, Westendorp RGJ. Does depression in old age increase only cardiovascular mortality? The Leiden 85-plus study. Int J Geriatr Psychiatry. 2004;19:852–857. doi: 10.1002/gps.1169. [DOI] [PubMed] [Google Scholar]
- 48.Marzari C, Maggi S, Manzato E, Destro C, Noale M, Bianchi D, et al. Depressive Symptoms and Development of Coronary Heart Disease Events: The Italian Longitudinal Study on Aging. The Journals of Gerontology: Series A: Biological Sciences and Medical Sciences. 2005;60A:85–92. doi: 10.1093/gerona/60.1.85. [DOI] [PubMed] [Google Scholar]
- 49.Kamphuis MH, Kalmijn S, Tijhuis MA, Geerlings MI, Giampaoli S, Nissinen A, et al. Depressive symptoms as risk factor of cardiovascular mortality in older European men: the Finland, Italy and Netherlands Elderly (FINE) study. Eur J Cardiovasc Prev Rehabil. 2006;13:199–206. doi: 10.1097/01.hjr.0000188242.64590.92. [DOI] [PubMed] [Google Scholar]
- 50.Glassman A. Depression and cardiovascular disease. Pharmacopsychiatry. 2008;41:221–225. doi: 10.1055/s-2008-1058108. [DOI] [PubMed] [Google Scholar]
- 51.Baghai TC, Binder EB, Schule C, Salyakina D, Eser D, Lucae S, et al. Polymorphisms in the angiotensin-converting enzyme gene are associated with unipolar depression, ACE activity and hypercortisolism. Mol Psychiatry. 2006;11:1003–1015. doi: 10.1038/sj.mp.4001884. [DOI] [PubMed] [Google Scholar]
- 52.Bondy B, Baghai TC, Zill P, Bottlender R, Jaeger M, Minov C, et al. Combined action of the ACE D- and the G-protein beta3 T-allele in major depression: a possible link to cardiovascular disease? Mol Psychiatry. 2002;7:1120–1126. doi: 10.1038/sj.mp.4001149. [DOI] [PubMed] [Google Scholar]
- 53.Shah AJ, Veledar E, Hong Y, Bremner JD, Vaccarino V. Depression and history of attempted suicide as risk factors for heart disease mortality in young individuals. Arch Gen Psychiatry. 2011;68:1135–1142. doi: 10.1001/archgenpsychiatry.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gallo JJ, Armenian HK, Ford DE, Eaton WW, Khachaturian AS. Major depression and cancer: the 13-year follow-up of the Baltimore epidemiologic catchment area sample (United States) Cancer Causes Control. 2000;11:751–758. doi: 10.1023/a:1008987409499. [DOI] [PubMed] [Google Scholar]
- 55.Horver MJ, Ries LA, Krapcho M, editors. NCI, SEER Cancer Statistics Review, 1975–2006. Bethesda, Maryland USA: National Cancer Institute; 2006. [Google Scholar]
- 56.Kircher T, Nelson J, Burdo H. The autopsy as a measure of accuracy of the death certificate. N Engl J Med. 1985;313:1263–1269. doi: 10.1056/NEJM198511143132005. [DOI] [PubMed] [Google Scholar]
- 57.Somes J, Donatelli NS. Car versus tree: accident or suicide attempt? J Emerg Nurs. 2011;37:179–181. doi: 10.1016/j.jen.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 58.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3 doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]