Abstract
Objective: To review the current status and recent trends in the American Board of Psychiatry and Neurology (ABPN) specialties and neurologic subspecialties and discuss the implications of those trends for subspecialty viability.
Methods: Data on numbers of residency and fellowship programs and graduates and ABPN certification candidates and diplomates were drawn from several sources, including ABPN records, Web sites of the Accreditation Council for Graduate Medical Education and the American Medical Association, and the annual medical education issues of the Journal of the American Medical Association.
Results: About four-fifths of neurology graduates pursue fellowship training. While most recent neurology and child neurology graduates attempt to become certified by the ABPN, many clinical neurophysiologists elect not to do so. There appears to have been little interest in establishing fellowships in neurodevelopmental disabilities. The pass rate for fellowship graduates is equivalent to that for the “grandfathers” in clinical neurophysiology. Lower percentages of clinical neurophysiologists than specialists participate in maintenance of certification, and maintenance of certification pass rates are high.
Conclusion: The initial enthusiastic interest in training and certification in some of the ABPN neurologic subspecialties appears to have slowed, and the long-term viability of those subspecialties will depend upon the answers to a number of complicated social, economic, and political questions in the new health care era.
Keywords: ABMS = American Board of Medical Specialties; ABPN = American Board of Psychiatry and Neurology; ACGME = Accreditation Council for Graduate Medical Education; MOC = maintenance of certification; RRC-N = Residency Review Committee in Neurology.
In American Medicine and the Public Interest: A History of Specialization, Stevens1 writes: “Arguably, specialization is the fundamental theme for the organization of medicine in the 20th century.” In Time to Heal, Ludmerer2 also identifies specialty and subspecialty certification as one of the positive actions taken over the last century “to assure that medical practice was conducted at the highest possible level,” and suggests that the trend toward subspecialization “rapidly accelerated” after World War II. While the observations of Stevens and Ludmerer may well be accurate, the historical movement toward specialization and subspecialization has been more intermittent than constant. There has been an ongoing debate over the past several decades about whether the US health care system would be better served by more primary care physicians than more specialists and subspecialists,3 and the Accreditation Council for Graduate Medical Education (ACGME) even initiated a moratorium on the recognition of new subspecialties from 1992 to 1993.4 In recent years, however, as detailed knowledge and clinical advances have increased, the pendulum seems to have swung more in the direction of promoting new subspecialties. At least to this point in time, the American public seems very protective of their “right” to receive medical care from the specialist or subspecialist of their choice.5
The American Board of Psychiatry and Neurology (ABPN) has 3 primary specialties: neurology, child neurology, and psychiatry. As Langsley6 suggested, the ABPN has been relatively conservative in its approach to subspecialties.6,7 The ABPN offered its first subspecialty, in child psychiatry, in 1959 but did not establish its first neurologic subspecialty, in clinical neurophysiology, until 1992 (child neurology is a primary specialty). Since then, however, the ABPN has recognized neurologic subspecialties in 6 other areas. The noninterdisciplinary subspecialty of vascular neurology (2005) was established only for neurologists. The interdisciplinary subspecialty of clinical neurophysiology (1992) was established for both neurologists and psychiatrists, while neurodevelopmental disabilities (2001) was established for neurologists and pediatricians, neuromuscular medicine (2008) for neurologists and physiatrists, and pain medicine (2000), sleep medicine (2007), and hospice and palliative medicine (2008) for neurologists, psychiatrists, and specialists in several other medical disciplines.
The decision by the ABPN to establish a new subspecialty is based upon a complicated analysis of several factors that will ultimately determine the long-term viability of the subspecialty.8 These include the current and recent trends in the number of neurologists practicing in the subspecialty, the number of current nonaccredited fellowship training programs and trainees and the estimated potential for new accredited fellowship programs and trainees, the scientific and academic basis for the subspecialty, and professional organizational support for the subspecialty. The assessment of several of these factors may be very difficult, especially estimating the potential for new accredited fellowship programs and trainees. Mistakes in this analysis can have significant political and financial consequences not only for general neurology and the new subspecialty but for the ABPN as well.
This article outlines the formal process for the recognition of a new subspecialty and reviews the recent trends in ABPN specialties and neurologic subspecialties. It concludes with a discussion of several of the implications of these data as well as some of the interrelated social, economic, and political questions, the answers to which will ultimately determine the fate of any existing or proposed neurologic subspecialty.
PROCESS FOR THE RECOGNITION OF A NEW NEUROLOGIC SUBSPECIALTY
The usual process for the recognition of a new neurologic subspecialty begins with a request from a group of practitioners in that area. Those practitioners usually seek the help of their professional societies (e.g., the American Academy of Neurology or other subspecialty societies) in advocating for recognition from the ABPN. The staff of those professional societies usually complete the required application forms and respond to requests by the ABPN for documentation of required information pertaining to the subspecialty. Once the application is complete, the ABPN decides whether to support the request. If the decision is positive, the ABPN requests formal approval from the American Board of Medical Specialties (ABMS). The ABMS then begins its own lengthy approval process that includes the opportunity for review and comment by the other ABMS Member Boards, professional societies, and the public.9 At the end of that process, which can take more than a year, the ABMS votes to approve or deny the request. If the request is approved, the ABPN appoints experts in the subspecialty area to develop the new certification and maintenance of certification (MOC) examinations.
Following ABMS approval, the ABPN also begins the process of seeking recognition of a new fellowship in the subspecialty from the Residency Review Committee in Neurology (RRC-N) and the ACGME. If the RRC-N and the ACGME approve the request, the RRC-N then develops the program requirements for residencies in the new fellowship. This complicated effort might take several years, during which time candidates are credentialed into the ABPN certification examination through a “grandfathering” process based upon their clinical experience in the subspecialty or completion of nonaccredited training. This “grandfathering” period usually lasts about 5 years, and once it ends, all candidates for certification must have completed an ACGME-accredited fellowship in the subspecialty. It is also possible for requests for subspecialty recognition to be made to the RRC-N and the ABPN at the same time or to begin with a request to the RRC-N. In any event, the approval process is similar to the more common process outlined above.
METHODS
ABPN records were reviewed for data on the numbers of specialty and subspecialty candidates for certification and MOC as well as the numbers of specialty and subspecialty certification and MOC certificates awarded. The Web site of the ACGME (acgme.org) provided the number of accredited residency and fellowship programs.10 The Web site of the American Medical Association (ama-assoc.org) provided data on the percent of residency graduates pursuing fellowship training.11 The annual medical education issues of the Journal of the American Medical Association provided data on the numbers of trainees and graduates.12–18 Due to their brief history, their interdisciplinary status, or the small numbers of participating neurologists, data were not available for several of the neurologic subspecialties.
RESULTS
The American Medical Association conducts an annual survey of training program directors about their graduates' postresidency plans. In 2008, it was reported that almost 80% of neurology graduates and about half of child neurology graduates intended to pursue additional training.11 For subspecialists, about 60% of vascular neurology graduates and about 25% of clinical neurophysiology graduates planned to do more training.11
The recent trends in numbers of ABPN specialty (neurology, child neurology, and psychiatry) residency programs, graduates, and new ABPN certification candidates (first-time takers) appear in table 1. Table 2 contains the same data for the subspecialties of clinical neurophysiology, neurodevelopmental disabilities, vascular neurology, and neuromuscular medicine. In recent years, there have been modest increases in the numbers of neurology, child neurology, and clinical neurophysiology programs, substantial increases in the numbers of neurodevelopmental disabilities, vascular neurology, and neuromuscular medicine programs, and a small decrease in the number of psychiatry programs. There were also increases in the numbers of graduates in neurology, child neurology, clinical neurophysiology, and vascular neurology but decreases in the numbers of graduates in neurodevelopmental disabilities and psychiatry.
Table 1 Recent trends in ABPN specialties: Number of residency training programs and graduates and number of new ABPN candidates
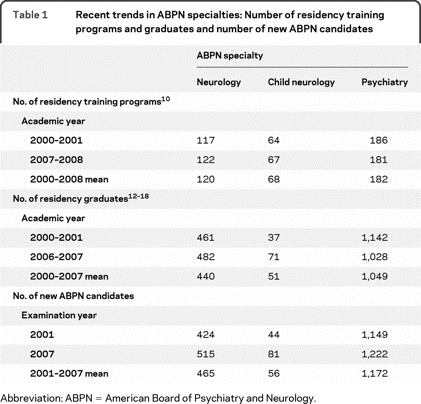
Table 2 Recent trends in ABPN subspecialties: Number of fellowship training programs and graduates and number of new ABPN candidates
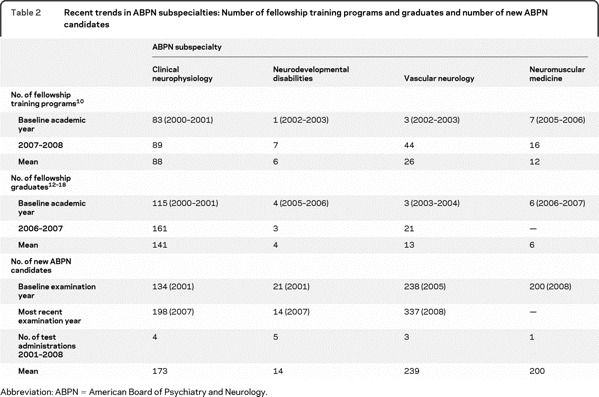
The numbers of new ABPN certification candidates increased in all areas except neurodevelopmental disabilities. In all 3 specialties, the mean numbers of new ABPN certification candidates exceeded the mean numbers of graduates, due in part to the participation in ABPN examinations of graduates from previous years. In clinical neurophysiology, however, the mean number of new ABPN candidates was substantially less than the mean number of graduates (about 60%).
Since the data pertaining to the numbers of new ABPN candidates in neurodevelopmental disabilities, vascular neurology, and neuromuscular medicine include “grandfathered” candidates who have not completed an ACGME-accredited fellowship, it is too early to draw conclusions about the participation in ABPN certification examinations by the graduates of these programs. For neurodevelopmental disabilities, ACGME-accredited training was required in 2009, and one candidate met that requirement. For vascular neurology, ACGME-accredited training will be required in 2010; thus far, 52 candidates (out of 718 new candidates) have met that requirement. For neuromuscular medicine, ACGME-accredited training will be required in 2013; thus far, 12 candidates (out of 200 new candidates) have met that requirement.
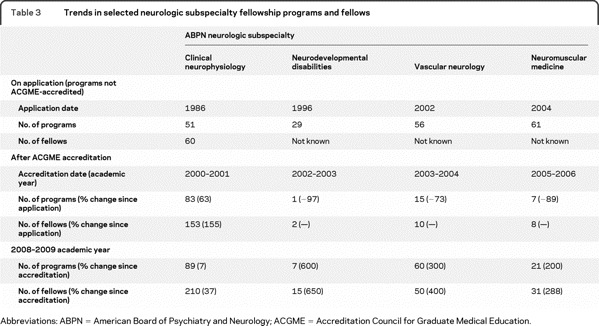
The trends in the numbers of selected neurologic fellowship programs and fellows from the date of the application to establish the programs until the 2008–2009 academic year are documented in table 3. By the date of ACGME accreditation, there were substantial increases in the numbers of clinical neurophysiology programs and fellows but substantial decreases in the numbers of neurodevelopmental disabilities, vascular neurology, and neuromuscular medicine programs. Because the numbers of fellows in these 3 subspecialties were not documented at the time of program application, the changes to the date of accreditation are unknown. From the dates of accreditation until academic year 2008–2009, there have been substantial increases in the numbers of programs and fellows in all of these subspecialties; however, the total numbers of programs and fellows in neurodevelopmental disabilities and neuromuscular medicine remain small.
Table 3 Trends in selected neurologic subspecialty fellowship programs and fellows
As mentioned previously, at the onset of a new subspecialty certificate, candidates can qualify via the practice track or completion of unaccredited training. After a relatively short period of time (usually 5 years), these tracks close, and all candidates have to complete training in an ACGME-accredited program. For clinical neurophysiology, those who attempted certification during the “grandfathering years” 1992–1998 had a 75% (975/1,292) examination pass rate, and for fellowship graduates the pass rate has been almost identical (837/1,102 = 76%).
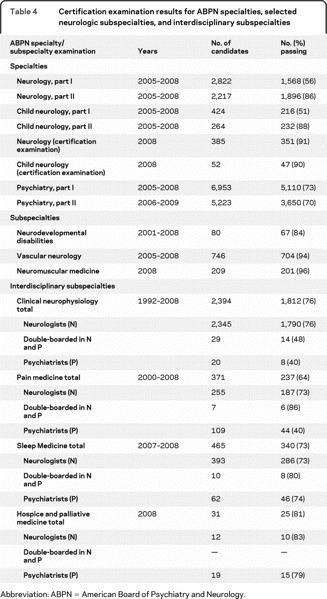
The recent certification examination results for ABPN specialties, selected neurologic subspecialties, and interdisciplinary subspecialties appear in table 4. Part I pass rates in all 3 ABPN specialties (neurology, child neurology, and psychiatry) have been lower than the pass rates in all of the neurologic subspecialty examinations and in the new certification examination that was administered for the first time in 2008 (replacing parts I and II for those meeting a new clinical skills requirement). For the interdisciplinary subspecialties (including clinical neurophysiology, which is also available to psychiatrists), about three-fourths of neurology candidates have successfully passed these examinations to date. The pass rates for psychiatry candidates have been somewhat lower in clinical neurophysiology and pain medicine.
Table 4 Certification examination results for ABPN specialties, selected neurologic subspecialties, and interdisciplinary subspecialties
Participation in MOC by ABPN specialty and clinical neurophysiology diplomates with time-limited certificates is summarized in table 5. Higher percentages of ABPN specialty diplomates have cho-sen to maintain their certification than their colleagues in clinical neurophysiology.
Table 5 Rates of participation in maintenance of certification and performance on maintenance of certification examinations
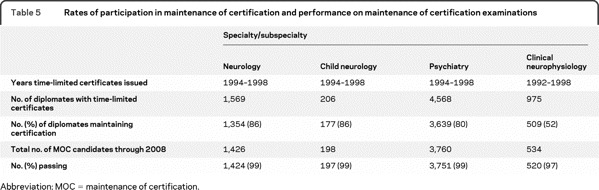
Table 5 also contains the total numbers of diplomates (time-limited plus lifetime certificate holders) in the ABPN specialties and clinical neurophysiology who have participated in MOC and their respective pass rates. To date, almost all participating diplomates have passed the MOC examinations. A comparison of the numbers of time-limited diplomates who have maintained certification with the total numbers of diplomate MOC candidates (time-limited plus lifetime certificate holders) suggests that only a few of those diplomates with lifetime certificates have chosen to participate in MOC to date. The President and CEO as well as all Directors of the ABPN are required to participate in MOC even if they hold lifetime certificates.
DISCUSSION
The data presented here indicate that most recent graduates of the ABPN primary specialties of neurology, child neurology, and psychiatry recognize the value of certification and attempt to achieve and maintain that status. While the main reasons for seeking certification are undoubtedly different among these specialists, they almost certainly include a desire to demonstrate competence to provide state-of-the-art quality care, obtain personal and professional recognition, become eligible for academic advancement, and fulfill credentialing requirements of service delivery systems and insurance panels.
Unlike their child neurology and psychiatry colleagues, most neurology graduates evidently see the value of fellowship training. Many neurologists who do pursue fellowship training in clinical neurophysiology do not perceive the added value of obtaining certification in that subspecialty to be worth the effort and expense to obtain it. (For 2010, the fees for specialty certification are $3,000, and for the subspecialties they are $1,900.) The ABPN requires all candidates for certification in a neurologic subspecialty to be certified first in neurology. Many fellowship-trained clinical neurophysiologists evidently consider their certification in neurology to be adequate to meet their practice and reimbursement requirements.
The original enthusiasm expressed in most of the neurologic subspecialty applications about the opportunities to increase the future numbers of accredited fellowship programs seems not to have been completely realized. While the numbers of clinical neurophysiology programs and fellows have steadily increased from the date of application, the numbers of neurodevelopmental disabilities, vascular neurology, and neuromuscular medicine programs and fellows initially decreased substantially. In recent years, the numbers of programs and fellows have increased substantially in vascular neurology and neuromuscular medicine and minimally in neurodevelopmental disabilities.
Large numbers of practicing subspecialists desiring certification do not necessarily translate into an adequate number of fellowship programs or sufficient numbers of trainees recruited into those programs to ensure the long-term survival of the subspecialty. The numbers of “grandfathers” seeking certification have been greater than the numbers of fellowship graduates doing so for all of the neurologic subspecialties. Under the current ABPN examination development process, fees from about 150 candidates are required to cover examination costs. Given the current number of fellowship graduates, it is unlikely that that number of candidates will be achieved in any subspecialty other than clinical neurophysiology even by administering the subspecialty examinations every other year.
The equivalent average performance of clinical neurophysiology graduates compared to “grandfathers” on the certification examination raises questions about the added value of fellowship training in that subspecialty. It appears that the experiences available to the “grandfathers” prepared them adequately for the breadth of content covered on the ABPN certification examination. Of course, it is also probable that additional competencies are gained through fellowship training that are not assessed on the ABPN certification examination.
The part I examinations in the ABPN specialties appear to have been barriers to certification for many candidates. While residents, residency programs, and residency graduates historically have expended considerable effort in preparation for the ABPN oral part II examinations, these results suggest that perhaps greater attention should have been paid to preparing for the content covered in these basic cognitive examinations. Since subspecialty certification is not possible without specialty certification, the part I examinations have also served as a barrier to subspecialty certification. While the performance of candidates on the initial administration of the new neurology and child neurology certification examination appears to be superior to the performance of candidates on the part I examinations, it is well to remember that only new candidates who have just finished their residencies took the new certification examination while the part I examinations included both new and repeat candidates. When only new part I candidates are considered, their pass rate is only about 5% less than that of the new certification examination candidates.
Once fellowship graduates achieve ABPN specialty certification, their success on the subspecialty examinations has been very good. This is undoubtedly due in part to their clinical experiences and participation in fellowship training. It also seems likely, however, that some individuals are very adept at taking standardized examinations, and their success on the part I examination predicts a high likelihood of success on subsequent subspecialty examinations.
Just as clinical neurophysiology graduates seek certification in smaller percentages than specialty graduates, to date they have also maintained their certification in smaller percentages than specialty diplomates. Like their colleagues who never sought certification in the first place, these subspecialty diplomates have evidently concluded that the value of subspecialty certification is not currently worth the effort and expense to maintain it.
Most specialty and clinical neurophysiology diplomates who seek to maintain their ABPN certification have little trouble passing the MOC examinations. (In 2010, the fees for these examinations are $1,500.) These results should not be surprising, since all of these diplomates have already passed the relatively difficult part I and part II specialty certification examinations, most are only about 10 years into their careers, and the MOC examinations focus on practical, clinically oriented content. Whether or not these same diplomates will be able to maintain these levels of performance over time remains to be seen.
While the current status of some ABPN neurologic subspecialties (clinical neurophysiology and vascular neurology) seems fairly secure, others (neurodevelopmental disabilities and neuromuscular medicine) remain in doubt. The long-term viability of any neurologic subspecialty will most likely depend on the answers to at least some of the following interrelated social, economic, and political questions, which are not presented in any particular order of priority. Each of these questions could be the subject of an extensive analysis in its own right, and space limitations permit only brief comments here.
First, will there be a change in emphasis on subspecialty care in the new health care era? Political decisions about the relative need for different types of physicians in the coming years could have a major impact on the types of students recruited into medical schools and the interest of those students in subspecialty medicine.
Second, will the public have ready access to subspecialty services or will there be renewed efforts by the payers for clinical services to encourage gatekeeping by primary care physicians and specialists? Economic or administrative barriers to subspecialty physician access could have a negative impact on the interest of physicians in pursuing additional training and certification in those areas.
Third, will there be increased public and political pressure on physicians to objectively demonstrate that they are competent to provide quality clinical care? If so, then additional subspecialty training and certification credentials could well be of value to physicians.
Fourth, will public and private institutions that credential physicians or pay for clinical services increase their requirements for subspecialty training and certification? If those institutions continue to credential and reimburse non-subspecialty-trained or non-subspecialty-certified physicians, there will be little incentive to pursue subspecialty training or certification.
Fifth, will adequate numbers of stipends be available to support fellowship training? Closely related to the first question above, government and private support of fellowship education will be a major determinant of whether or not subspecialties thrive in the future.
Sixth, will future research findings support the continued existence of specific subspecialties? Biomedical and genetic research developments are producing dramatic changes in our basic understanding of health and disease processes. No subspecialty can exist for long without an academic basis of support, and it may well be that some current subspecialties will be replaced with entirely new conceptual models for education, research, and clinical services.
Seventh, will states adopt maintenance of licensure requirements mandating that physicians document objectively their competence to provide quality medical care to specific types of patients in order to remain licensed to practice medicine? If so, then it is likely that those states will accept ABPN certification and MOC participation as sufficient to meet their requirements, and this could promote added interest in subspecialty training and certification.
Eighth, will the ABPN develop new methods for subspecialty certification that reduce costs? The ABPN is currently exploring new and less expensive methods for the development of subspecialty examinations that might reduce the certification fees for existing subspecialties and also make it more feasible to recognize new ones. Anything that improves the cost-benefit ratio for subspecialty certification will likely result in increased numbers of physicians seeking that status.
While the ABPN was relatively slow to embrace the subspecialty movement, in recent years it has recognized increasing numbers of subspecialties. The interest of physicians in training and certification in some of the subspecialties, however, has not lived up to expectations. Whether or not any of the ABPN subspecialties will thrive in the future will depend upon a complicated series of questions whose answers will be decided in the social, political, and economic arenas of the new health care era.
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. Larry R. Faulkner and Dr. Dorthea Juul.
DISCLOSURE
Dr. Faulkner serves as President and CEO of the American Board of Psychiatry and Neurology (ABPN). Dr. Juul is an employee of the ABPN. Dr. Pascuzzi receives honoraria from the ABPN. Dr. Aminoff receives royalties from the publication of Neurology & General Medicine (Elsevier, 2008), Clinical Neurology (McGraw-Hill, 2009), and chapters in Cecil (Saunders), Harrison's (McGraw-Hill), and Current Medical Diagnosis & Treatment (McGraw-Hill) 2008–2009; has received speaker honoraria from Baxter International Inc.; serves as a consultant for iPierian, Inc. and Biovail Corporation; served as Editor-in-Chief, Neurology Section, for UpToDate; receives/has received research support from Genzyme Corporation, the NIH (NINDS 5 U10 NS044460 [Site PI] and R01 NS37167 [Site PI]), and the University of Rochester; has served as an expert witness in legal proceedings; and receives honoraria from the ABPN. Dr. Crumrine serves on the editorial boards of the Journal of Child Neurology and Pediatric Neurology; receives research support from the J. Kiffin Penry Pediatric Epilepsy Fellowship Program and the NIH (NINDS NS045911 [site PI] and NINDS NS045803 [site PI]); and receives honoraria from the ABPN. Dr. DeKosky serves/has served on scientific advisory boards for Pfizer Inc., Eisai Inc. PsychoGenics Inc., United Medical Corporation, Novartis, and Wyeth; serves on the editorial boards of Annals of Neurology, Archives of Neurology, Neurodegenerative Diseases, the Journal of Alzheimer's Disease, Alzheimer Disease and Associated Disorders: An International Journal, and as Editor of UpToDate; receives research support from the NIH (NIA AG14449 [PI, then Co-I], NINDS NS30318 [PI, then Co-I], NIA AG05133 [PI, then Co-I], and NCCAM AT00162 [PI]) and the National Advisory Council (National Center for Complementary and Alternative Medicine); and receives honoraria from the ABPN and the Alzheimer's Association. Dr. Jozefowicz receives honoraria from the ABPN. Dr. Massey serves on the editorial board of Seminars in Neurology; serves as a consultant for Novella Clinical; receives research support from the Myasthenia Gravis Foundation of America, Alexion Pharmaceuticals, Inc., AANEM Research Foundation, and the NIH (R01 NS0442685-0142) [site PI]); receives education grant support from Allergan, Inc.; and receives honoraria from the ABPN. Dr. Pirzada receives honoraria from the ABPN. Dr. Tilton serves/has served on scientific advisory boards for Ipsen and Medtronic, Inc.; has served on a speakers' bureau for and received funding for travel and speaker honoraria from Medtronic, Inc.; serves on the editorial boards of Neurology® and the Journal of Child Neurology; has a patent for Botulinum toxin in the treatment and prevention of acne; has received research support from Allergan, Inc.; and receives honoraria from the ABPN.
Footnotes
Disclosure: Author disclosures are provided at the end of the article.
Received November 9, 2009. Accepted in final form May 28, 2010.
REFERENCES
- 1.Stevens R. American Medicine and the Public Interest: A History of Specialization. Berkeley: University of California Press; 1971
- 2.Ludmerer KM. Time to Heal: American Medical Education from the Turn of the Century to the Era of Managed Care. New York: Oxford University Press; 1998
- 3.Council on Graduate Medical Education: 2002. Summary Report. Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration; 2002.
- 4.Case GL. Letter dated June 9, 1992. Chicago: Accreditation Council for Graduate Medical Education; 1992.
- 5.Council on Graduate Medical Education. Sixteenth Report: Physician Workforce Policy Guidelines for the United States, 2000–2020. Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration; 2005
- 6.Langsley DG. Certification in psychiatry and neurology: past, present, and future. In: Shore JH, Scheiber SC, eds. Certification, Recertification, and Lifetime Learning in Psychiatry. Washington, DC: American Psychiatric Press; 1994:19–34.
- 7.Juul D, Scheiber SC, Kramer TAM. Subspecialty certification by the American Board of Psychiatry and Neurology. Academic Psychiatry 2004;28:12–17. [DOI] [PubMed] [Google Scholar]
- 8.American Board of Psychiatry and Neurology. ABPN Criteria for Approving New Subspecialties. Buffalo Grove, IL: American Board of Psychiatry and Neurology; 2008
- 9.American Board of Medical Specialties. ABMS Reference Handbook and Certificate Statistics. Evanston, IL: American Board of Medical Specialties; 2008
- 10.Number of accredited programs by academic year. Available at: www.acgme.org Accessed February 11, 2009.
- 11.FREIDA online graduates' career plans. Available at: www.ama-assn.org Accessed November 4, 2009.
- 12.Graduate medical education. JAMA 2002;288:1151–1164. [PubMed] [Google Scholar]
- 13.Graduate medical education. JAMA 2003;290:1234–1248.12962081 [Google Scholar]
- 14.Graduate medical education. JAMA 2004;292:1099–1113. [DOI] [PubMed] [Google Scholar]
- 15.Graduate medical education. JAMA 2005;294:1129–1143. [PubMed] [Google Scholar]
- 16.Brotherton SE, Etzel SI. Graduate medical education, 2005–2006. JAMA 2006;296:1154–1169. [DOI] [PubMed] [Google Scholar]
- 17.Brotherton SE, Etzel SI. Graduate medical education, 2006–2007. JAMA 2007;298:1081–1096. [DOI] [PubMed] [Google Scholar]
- 18.Brotherton SE, Etzel SI. Graduate medical education, 2007–2008. JAMA 2008;300:1228–1243. [DOI] [PubMed] [Google Scholar]


