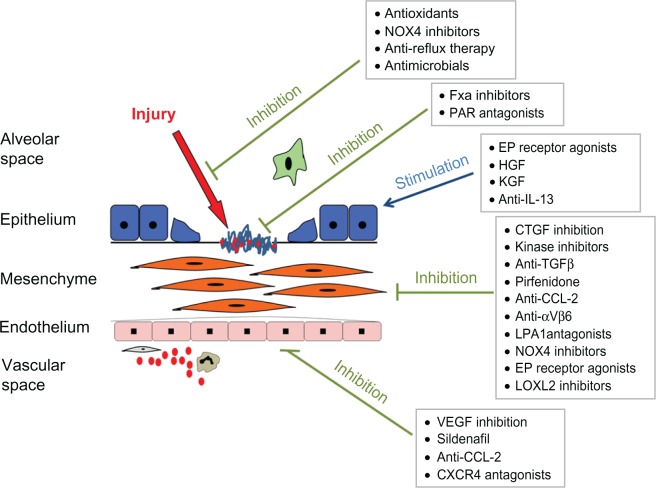
Figure 1.
Current understanding of the pathogenesis of idiopathic pulmonary fibrosis (IPF) suggests that repetitive alveolar epithelial injury results in basement membrane denudation and activation of key pathways involved in the wound-healing response.
Notes: This in turn leads to fibroblast proliferation, transformation of fibroblasts to myofibroblasts, and expansion of the extracellular matrix. These effects are augmented by the influx of circulating inflammatory cells, including the putative bone marrow–derived fibroblast precursor – the fibrocyte. Various treatments are in development targeting different aspects of IPF disease pathogenesis through inhibition of fibrogenesis, promotion of antifibrotic pathways, or reduction of alveolar injury.
Copyright© 2012. Reprinted with permission from Elsevier. Maher TM. Idiopathic pulmonary fibrosis: pathobiology of novel approaches to treatment. Clin Chest Med. 2012;33:69–83.54
Abbreviations: FXa, factor Xa; PAR, protease-activated receptor; HGF, hepatocyte growth factor; KGF, keratinocyte growth factor; IL, interleukin; TGF, transforming growth factor; CTGF, connective tissue growth factor; VEGF, vascular endothelial growth factor; NOX4, NADPH Oxidase 4. EP, E prostanoid; LPA, Lysophosphatidic acid; CCL-2, Chemokine (C-C motif) ligand 2.