The recently published article by Gadaleta and co-workers1 has demonstrated that activation of the bile acid (BA) nuclear receptor, Farnesoid X receptor α (FXR), affords multi-level protection against intestinal inflammation and inflammatory bowel disease (IBD) in mice. Of the numerous avenues of research into IBD diagnosis and treatment that are opened by these findings, the questions posed by Gadaleta and co-workers regarding the contribution of gut bacteria to FXR modulation and aetiology of IBD are of particular significance.
Bacteria resident in the human gastrointestinal tract collectively encode a distributed pathway of BA modification, the products of which are the natural ligands for FXR,2 and there is growing appreciation that this may be a key activity through which the gut microbiota integrates factors relating to diet and mucosal inflammation, to initiate or exacerbate disease.3 These modified BAs display altered binding profiles for BA receptors, with several secondary BAs being among the most potent agonists. Moreover, microbial transformation could also influence BA bioavailability for receptor binding.2 In conjunction with the protective role of FXR activation described by Gadaleta and co-workers,1 it is logical to hypothesise that the dysbiosis of the gut microbiota characteristic of IBD may alter capacity for BA modification in this community. In turn, such functional shifts may perturb BA-associated regulation of mucosal inflammatory processes, via alterations in FXR-mediated signalling.
To determine whether the capacity for BA modification is altered in the gut microbiomes of IBD patients, we embarked on an in silico analysis to determine the relative abundance of bile salt hydrolases (BSHs) in the gut microbiomes of IBD patients compared with healthy controls. Since BSH catalyses the ‘gateway’ reaction in microbial BA modification,4 the relative abundance of this function should be indicative of the capacity for BA modification in the gut microbiome.5
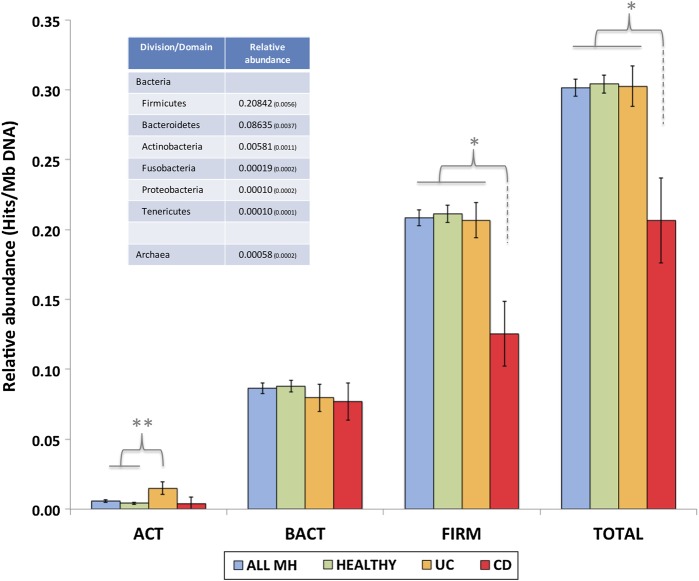
The amino acid sequences of 24 functional BSH ‘types’ were used to search human gut metagenomes constituting the MetaHIT (Metagenomics of the Human Intestinal Tract) dataset,6 which comprises the gut microbiomes of 124 individuals of varying disease status (99 healthy, 21 ulcerative colitis, 4 Crohn's disease). Sequences in the MetaHIT dataset producing valid hits (tBlastn: minimum 35% identity ≥50 amino acids, 1e−5) to these functional BSH types were retrieved, and encoded BSH-like homologues were affiliated with a phylogenetic division based on top hits (by bit-score) from subsequent BlastX searches of the non-redundant dataset. Affiliated hits were then used to construct non-redundant BSH relative abundance profiles for major phylogenetic divisions in the human gut microbiota (figure 1), as previously described.5
Figure 1.
Bile salt hydrolase (BSH) relative abundance profiles for major phylogenetic divisions in the human gut microbiota. ACT, Actinobacteria; BACT, Bacteroidetes; FIRM, Firmicutes; TOTAL, BSH-like relative abundance in complete MetaHIT dataset regardless of phylogenetic affiliation. ALL MH, complete MetaHIT dataset, HEALTHY, healthy individuals only, UC, individuals with ulcerative colitis only, CD, individuals with Crohn's disease only. Error bars indicate SEM. Level of significance in χ2 distribution analysis: *p<0.01, **p<0.001. Inset table shows relative abundance, within complete MH dataset, for other phylogenetic divisions with which BSH-like homologues were affiliated. Brackets denote SEM.
The majority of BSH-like sequences identified were affiliated with the Firmicutes division followed by the Bacteroidetes and Actinobacteria, and their general distribution between divisions was congruent with the overall composition of the human gut microbiome.6 However, we observed distinct alterations in total and division-specific BSH relative abundance in individuals diagnosed with Crohn's disease (CD) and ulcerative colitis (UC), compared with healthy individuals (figure 1). Most notable were alterations in the CD group, where BSH relative abundance was significantly reduced in the Firmicutes affiliated sequences, but no significant alterations were observed in Bacteroidetes and Actinobacteria affiliated sequences. In addition to a reduction in total BSH relative abundance, the intestinal BA metabolic profile is also likely to be altered due to distinct differences in substrate ranges of BSH originating in the Bacteroidetes compared with Firmicutes and Actinobacteria.5
Overall, this initial in silico analysis provides evidence that shifts in population structure associated with IBD perturb functions of the gut microbiome involved in FXR-mediated signalling. In tandem with the work of Gadaleta and co-workers,1 this supports the hypothesis that variations in the capacity for BA modification in the gut microbiome may be a significant factor in the onset or progression of IBD. When considered against the host genetic background of immune dysregulation, believed to be key to IBD initiation, even small perturbations in systems controlling mucosal immune responses could be important in helping sustain the inappropriate inflammatory response that results in tissue damage. If so, this opens exciting possibilities for disease treatment, prophylaxis and diagnosis. Larger, more detailed studies should now be undertaken to confirm these initial observations, and explore the potential for manipulating and exploiting this facet of host–microbe interaction in the human gut.
Footnotes
Contributors: LAO and BVJ conceived the study, analysed the data and wrote the article.
Funding: This work was supported by funding from the Medical Research Council (Grant ID number 93344/G0901553 awarded to BVJ).
Competing interests: None.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Gadaleta RM, van Erpecum KJ, Oldenburg B, et al. Farnesoid X receptor activation inhibits inflammation and preserves the intestinal barrier in inflammatory bowel disease. Gut 2011;60:463–72 [DOI] [PubMed] [Google Scholar]
- 2. Thomas C, Pellicciari R, Pruzanski M, et al. Targeting bile-acid signalling for metabolic diseases. Nat Rev Drug Discov 2008;7:678–93 [DOI] [PubMed] [Google Scholar]
- 3. O'Keefe SJD. Nutrition and colonic health: the critical role of the microbiota. Curr Opin Gastroen 2008;24:51–8 [DOI] [PubMed] [Google Scholar]
- 4. Ridlon JM, Kang DJ, Hylemon PB. Bile salt biotransformations by human intestinal bacteria. J Lipid Res 2006;47:241–59 [DOI] [PubMed] [Google Scholar]
- 5. Jones BV, Begley M, Hill C, et al. Functional and comparative metagenomic analysis of bile salt hydrolase activity in the human gut microbiome. Proc Natl Acad Sci USA 2008;105:13580–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Qin J, Li R, Raes J, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010;464:59–65 [DOI] [PMC free article] [PubMed] [Google Scholar]