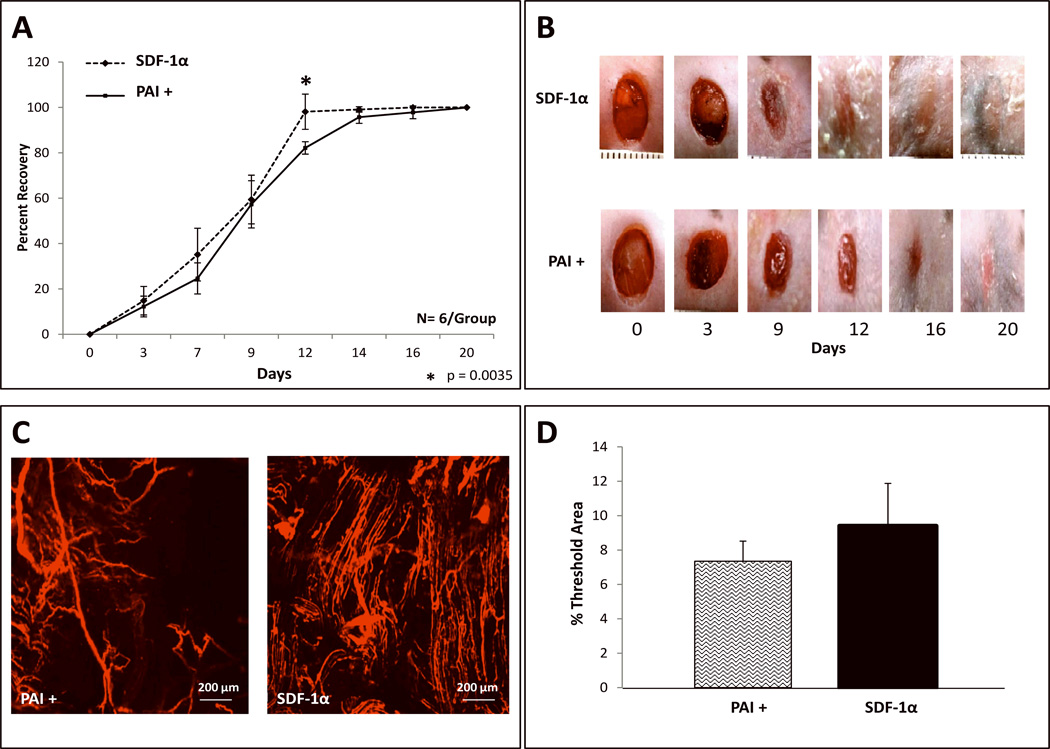
FIGURE 6. Inhibition of the Plasminogen/Pm axis by PAI-1 mildly reverses the wound healing and wound vessel density effects of SDF 1α-Primed-BMDSC.
A: Wound healing rate expressed as percent recovery. Two groups of Type 2 diabetic Leprdb/db mice were wounded and treated with [ex vivo SDF-1α activated diabetic BMDSC (labeled as SDF 1α)] versus [PAI-1 plus ex vivo SDF-1α activated diabetic BMDSC (labeled as PAI+)]. Wounds were followed and analyzed using digital photography and Image J software. Diabetic wounds in the PAI+ group had mildly prolonged wound closure rate compared to wounds treated only with SDF-1α activated BMDSC. A statistically significant delay in wound closure was noted between POD 9 through POD 12. B: Representative images of wounds at different time points are shown for both groups. C: Wound blood vessel perfusion as detected by DiI dye; images acquired using laser scanning confocal microscopy show DiI-stained blood vessels within the diabetic wounds, at day 21 post wounding. D: Quantification of vessel density in the wounds expressed as % threshold area, which covers all vessels detected as a percent of the entire wound area. SDF-1α treated wounds showed a trend towards less vessel density compared to PAI+ treated wounds, but the means did not reach statistical significance. Data are presented as mean ±SD of 6 wounds in each group.