Abstract
Pituicytoma is a rare primary tumour of the neurohypophysis or infundibulum, which masquerades as a pituitary adenoma. We present a pituicytoma case in a 45-year-old female presenting as a focal lesion of the neurohypophysis. This case report reviews the clinical, neuroimaging and histopathological features of this rare tumour in order to understand it better.
Pituicytomas are very rare primary tumours of the adult neurohypophysis. They may be easily confused with pituitary adenoma, craniopharyngiomas and meningioma owing to their location in the sella and suprasellar region. In 2007, pituicytoma was named as a distinct entity according to the World Health Organization (WHO) classification of central nervous system tumours [1, 2]. We present the clinicopathological features and review the literature in order to understand the natural history, behaviour and treatment of this rare tumour.
Case report
A 45-year-old female patient with a 1 year history of decreased left eye vision was admitted to our hospital with polyuria and dry mouth in 2009. She had experienced progressively increasing headaches over the 2 months prior to admission.
Neurological examination disclosed bitemporal hemianopsia. Endocrine studies for the pituitary gland were normal except for an elevated level of serum prolactin (PRL) (187.97 ng⋅ml−1). MRI demonstrated a nodular thickening of the pituitary stalk with homogeneous signal intensity. The nodule was slightly hypointense on T1 weighted images, hyperintense on T2 weighted images and showed marked enhancement following intravenous (iv) administration of Gd-DTPA.
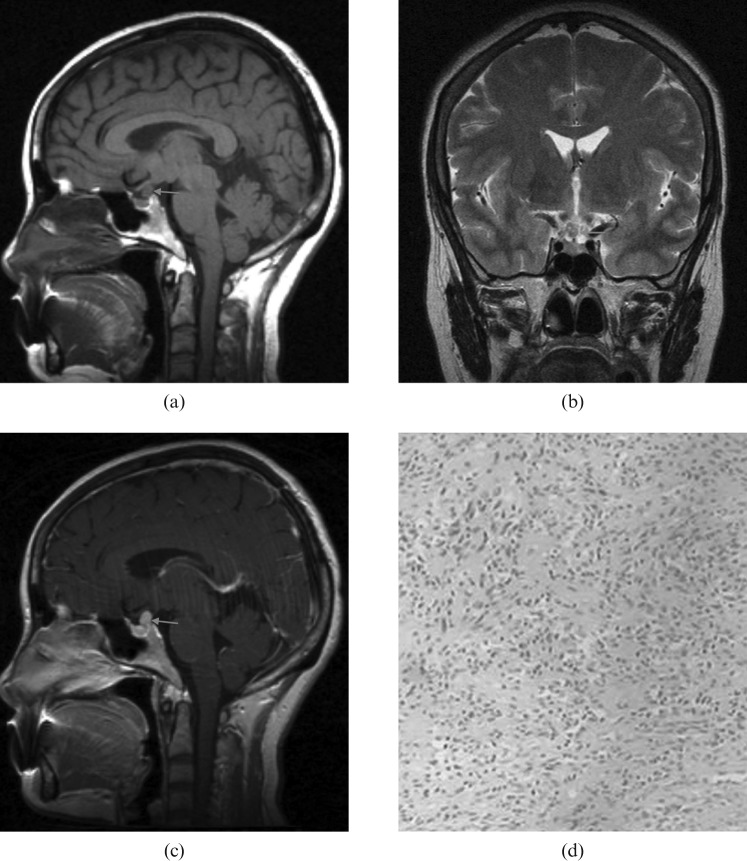
The mass was totally resected via a transsphenoidal approach. An intra-operative view showed a reddish solid and hypervascular nodule in the middle of the pituitary stalk, measuring 1.0 × 0.8 cm. The nodule was pressed tightly against the optic chiasm (Figure 1).
Figure 1.
(a) Sagittal unenhanced T1 weighted MRI showing nodular thickening of the pituitary stalk causing optic chiasmal compression (arrow). Note the absence of hyperintensity within the hypophysis. (b) Coronal T2 weighted MRI showed slight hyperintensity of the tumour compared with the brain parenchyma (arrow). (c) Sagittal contrast-enhanced T1 weighted MRI demonstrated marked enhancement of the tumour (arrow). (d) Histology with haematoxylin and eosin stain revealed the tumour to be composed of spindle-shaped cells, which are characterised by a storiform structure.
Pathological examination revealed the tumour to be composed of spindle-shaped cells, which are characterised by a storiform structure and are slightly pleomorphic. No significant mitotic activity was seen. Immunohistochemical studies showed tumour cells to be immunoreactive for vimentin, S-100 protein, epithelial membrane antigen (EMA) and glial fibrillary acidic protein (GFAP). No anterior pituitary tissue was present and routine immunohistochemistry was negative for p53 protein, Ki-67, synaptophysin (Syn), PRL, growth hormone (GH), follicle-stimulating hormone (FSH), thyroid stimulating hormone (TSH) and adrenocorticotropic hormone (ACTH). The histopathological diagnosis was pituicytoma WHO Grade I.
Discussion
The term “pituicytoma” has been used to refer to granular cell tumour, infundibuloma, and pilocytic astrocytoma affecting the suprasellar region, infundibulum or posterior pituitary [1]. According to the 2007 WHO classification of tumours of the central nervous system, pituicytoma is defined as a low-grade spindle cell astrocytic tumour affecting adults, originating in the posterior pituitary or its stalk [1, 2]. The tumour is considered WHO Grade I. Pituicytomas are rare, to date only 31 cases have been reported [3-15]. All tumours have occurred in adults with a male predilection of 1.6:1 [1].
Clinical presentation
The clinical symptoms are variable owing to tumour size and location. For example, bitemporal haemianopsia can be caused by optic chiasm compression. Infundibular compression results in interference of hypothalamic dopamine delivery, with subsequent hyperprolactinemia and the accompanying amenorrhea and decreased libido [3]. Rarely, pituicytoma has been reported as an incidental autopsy finding or presented with spontaneous haemorrhage [4, 5].
Clinically, even without optic chiasm compression, pituicytomas can still cause blindness in the superior temporal quadrant of the visual field at an early stage by decreasing blood supply to the central zone of the optic chiasm. This may be explained by the fact that the anteroinferior aspect of the optic chiasm shares a common blood supply, the superior hypophyseal artery, with the pituitary gland and infundibuloma, and, consequently, the pituicytoma.
Our case presented with bitemporal haemianopsia owing to optic chiasm compression. In addition, the patient had diabetes insipidus and the absence of a high signal for the posterior pituitary gland on the T1 weighted image might be interpreted as an infiltration of the pituitary stalk.
CT and MRI findings
Pituicytomas have few distinctive radiographic features. On CT and MRI scans, pituicytomas are architecturally solid and demarcated as homogeneous in appearance. Our case showed a small round mass of homogeneous signal intensity on MRI, similar to pituitary adenomas. Sometimes they can exhibit sellar enlargement and bony remodelling [6]. Most reported MRI findings are isointense on T1 weighted images and hyperintense on T2 weighted images, with marked homogeneous enhancement after administration of gadolinium [3, 6-15]. Gibbs et al [7] depicted apparent tumour stain during the venous phase of selective internal carotid artery angiograms and, even during the late venous phase, the shape of the tumour stain could still be seen well. So we can speculate that pituicytoma had a slightly delayed enhancement on dynamic contrast-enhanced studies, unlike pituitary adenoma which was apparently enhanced during the earlier arterial phase. Histology confirmed that the tumour had developed blood vessel networks. Heterogeneous enhancement, calcification and cystic change were rarely seen [3, 8-15]. Pituicytomas should be distinguished from other tumours predominantly arising from the optic chiasm with extension up into the infundibulum, such as meningioma, glioma, metastasis and langerhans cell histiocytosis.
Histopathology
On gross examination, the specimen revealed a peach or rose colour, was solid in nature, had a well-demarcated margin and was highly vascular. Histological findings were similar to other cases in the literature. Pituicytomas consist almost exclusively of elongated bipolar spindle cells arranged in interlacing fascicles or in a storiform pattern [3, 6-15]. Nuclei are moderate in size, often oval or elongate, and generally show little atypia. Mitoses are rare to absent. No Rosenthal fibres and eosinophilic granular bodies were seen. Pituicytomas are immunoreactive for vimentin, S-100 protein and GFAP (usually focal). Cytoplasmic EMA positivity is occasionally seen. No neuronal or neuroendocrine marker reactivity, such as neurofilament protein, synaptophysin or chromogranin is evident, nor are pituitary hormones present [1].
Pituicytoma is a slow-growing, rare low-grade glial neoplasm that originates in the neurohypophysis. The best treatment is gross total resection via skull base or a transsphenoidal approach, which might benefit from pre-operative embolisation owing to its high vascularity. We believe that the inclusion of this unusual tumour in the differential diagnosis of a pituitary lesion is useful because of the potential for significant peri-operative haemorrhage unlike pituitary adenomas, especially if the surgeon is not aware of this possibility.
Reference
- 1.Brat DJ, Scheithauer BW, Fuller GN, Tihan T. Newly codified glial neoplasms of the 2007 WHO classification of tumours of the central nervous system: angiocentric glioma, pilomyxiod astrocytoma and pituicytoma. Brain Pathol 2007;17:319–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. Scheithauer, Paul Kleihues. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brat DJ, Scheithauer BW, Staugaitis SM, Holtzman RNN, Morgello S, Burger PC. Pituicytoma: a distinctive low-grade glioma of the neurohyophysis. The Am J Surg Pathol 2000;24:362–8 [DOI] [PubMed] [Google Scholar]
- 4.Takei H, Goodman JC, Tanaka S, Bhatacharjee MB, Bahrami A, Powell SZ. Pituicytoma incidentally found at autopsy. Pathol Int 2005;55:745–9 [DOI] [PubMed] [Google Scholar]
- 5.Beveniste RJ, Purohit D, Byun H. Pituicytoma presenting with spontaneous hemorrhage. Pituitary 2006;9:53–8 [DOI] [PubMed] [Google Scholar]
- 6.Wolfe SQ, Bruce J, Morcos JJ. Pituicytoma: Case report. Neurosurgery 2008;63:173–4 [DOI] [PubMed] [Google Scholar]
- 7.Gibbs WN, Monuki ES, Linskey ME, Hasso AN. Pituicytoma: diagnostic features on selective carotid angiography and MR imaging. Am J Neuroradiol 2006;27:1639–42 [PMC free article] [PubMed] [Google Scholar]
- 8.Uesaka T, Miyazono M, Nishio S, Iwaki T. Astrocytoma of the pituitary gland (pituicytoma): case report. Neuroradiology 2002;44:123–5 [DOI] [PubMed] [Google Scholar]
- 9.Shah B, Lipper MH, Laws ER, Lopes MB, Spellman MJ. Posterior pituitary astrocytoma: A rare tumour of the neurohypophysis: a case report. Am J Neuroradiol 2005;26:1858–61 [PMC free article] [PubMed] [Google Scholar]
- 10.Ulm AJ, Yachnis AT, Brat DJ, Rhoton AL. Pituicytoma: report of two cases and clues regarding histogenesis. Neurosurgery 2004;54:753–8 [DOI] [PubMed] [Google Scholar]
- 11.Scheithauer BW, Swearingen B, Hedley Whyte ET, Auluck PK, Stemmer-Rachamimov AO. Ependymoma of the sella turcica: a variant of pituicytoma. Hum Pathol 2009;40:435–40 [DOI] [PubMed] [Google Scholar]
- 12.Figarella-Branger D, Dufour H, Fernandez C, Bouvier-Labit C, Grisoli F, Pellissier JF. Pituicytomas, a mis-diagnosed benign tumour of the neruohypophysis: report of three cases. Acta Neuropathol 2002;104:313–19 [DOI] [PubMed] [Google Scholar]
- 13.Katsuta T, Inoue T, Nakagaki H, Takeshita M, Mroimoto K, Iwaki T. Distinctions between pituicytoma and ordinary pilocytic astrocytoma. J Neurosurg 2003;98:404–6 [DOI] [PubMed] [Google Scholar]
- 14.Nakasu Y, Nakasu S, Saito A, Horiguchi S, Kameya T. Pituicytoma: two case reports. Neurol Med Chir 2006;46:152–6 [DOI] [PubMed] [Google Scholar]
- 15.Kowalski RJ, Prayson RA, Mayberg MR. Pituicytoma. Ann Diagn Pathol 2004;8:290–4 [DOI] [PubMed] [Google Scholar]