Abstract
Objective. To evaluate healthcare students’ perceptions of an introductory interprofessional exercise and their team dynamics.
Design. A workshop was developed, combining second-year medical students, fourth-year nursing students, and third-year pharmacy students to work as an interdisciplinary team. The teams alternated between working together on patient cases focusing on chronic obstructive pulmonary disease and asthma, and on the evaluation of standardized pneumonia patients. Teams were given the patients' health information and no other instructions. A faculty member and the standardized patient evaluated the students using a teamwork global rating scale.
Assessment. Student survey results showed a positive response to interprofessional teamwork. The faculty members and standardized patients reported that the students worked as a cohesive unit and demonstrated good team communication.
Conclusions. This introductory interprofessional experience had a positive impact on the students’ understanding of collaboration and teamwork. This type of experience will help students foster future collaborations as healthcare providers.
Keywords: interprofessional, team, workshop healthcare students, communication, collaboration
INTRODUCTION
The World Health Organization defines interprofessional education (IPE) as “occurring when two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes.”1 The Committee of Health Professions Education is involved in developing strategies for integrating a core set of competencies into the curriculum of future healthcare professionals, including “the ability of professionals to cooperate, collaborate, communicate, and integrate care as part of an interdisciplinary healthcare team.”2 Interprofessional education is necessary in preparing healthcare providers for effective collaborative practice, which will ultimately improve patient health outcomes.3
Accrediting bodies involved in health professional education and training recognize the need for IPE. The Accreditation Council for Pharmacy Education issued guidelines to ensure that graduates of all accredited pharmacy programs have the competencies needed to function as members of an interprofessional team.4 The Accreditation Council for Graduate Medical Education includes interpersonal and communication skills as 1 of its core competencies and specifically notes that resident physicians should work collaboratively in healthcare teams.5 In 2011, the Interprofessional Education Collaborative concluded that in a continuously evolving healthcare system, future healthcare professionals should be educated and trained in a collaborative manner.6 The guidelines developed by these organizations parallel the Institute of Medicine’s (IOM’s) 5 core competencies for healthcare professionals. One basic tenet of the IOM related to the provision of patient-centered care encourages health profession educators to instruct students on interprofessional teamwork, communication, ethics, and roles and responsibilities for collaborative practice.2
Several studies have evaluated IPE, one of which focused on communication skills through the use of a facilitated standardized patient encounter. A small change was noted in participants’ attitudes toward IPE after the event.7 Another study assessed a longitudinal curriculum in which students from medicine, pharmacy, and nursing worked in groups for 3 weeks and then were evaluated for differences in teamwork attitudes. A significant change in participants’ attitudes toward IPE were seen after the curriculum was completed.8 Another study demonstrated that interprofessional communication skills training in undergraduate medical education improved students’ confidence as well as their effectiveness in communicating with allied health professionals.9 Finally, and perhaps most practically, 1 study showed that educating nonpharmacy healthcare students about what pharmacists do increases student awareness of services provided by pharmacists.10
Only recently have researchers measured the value of incorporating IPE experiences using simulation for prelicensure healthcare students.11 One study looked at an IPE curriculum using simulation mannequins to teach cardiac resuscitation and intravenous access. Students felt that this curriculum was valuable and relevant. Another study demonstrated that medical and nursing students can work effectively together in a mock code situation.12 Studies also demonstrate that students from different health professions enjoy working with and learning from each other.13
In 2009, Health Canada awarded a grant to Dalhousie University, Halifax, Nova Scotia, Canada, to be used explicitly to introduce health professional students to IPE training early in their curriculum. The goal was to “develop students’ IPE skills through active and problem-based learning in a model called ‘Seamless Care.’”14 Using this model as our conceptual framework, we introduced IPE experiences to pharmacy, medical, and nursing students prior to their concentrated clinical training. This paper describes the implementation and evaluation of an IPE curriculum at 3 schools for health professions.
We set 2 goals for our IPE curriculum: to give students from pharmacy, nursing, and medicine insight into the knowledge and skills required for each discipline to function in the healthcare arena; and to create an environment for the students that would foster positive attitudes and allow them to build self-confidence as a member of an interprofessional healthcare team. This workshop enabled the students to develop a better understanding of the approaches various health professionals use when caring for patients. We evaluated the student outcomes of this initiative through a student survey instrument, standardized patient evaluation, and faculty evaluation.
DESIGN
In cooperation with the Warren Alpert School of Medicine of Brown University (AMS), the University of Rhode Island (URI) Colleges of Pharmacy and Nursing developed an interprofessional, student-focused workshop that introduces students to a team-based, patient-centered care experience. AMS is a medical school based in Providence, RI, and URI is a research university based in Kingston.
The initiative began in 2005 with the development of a series of interprofessional practice laboratory modules involving nursing and pharmacy students15 and was expanded in 2008 to include medical students. The objective of the curriculum is to introduce students to IPE early in their health professional curriculum. Faculty members met several times prior to the workshop to discuss intended student outcomes and content for each learning module. The exercise was designed to be an opportunity for active learning with 2 problem-based learning cases (1 each on chronic obstructive pulmonary disease and asthma) and 1 standardized patient encounter on pneumonia.
The workshop’s curriculum has been modified each year based on reviews of the literature and student feedback through survey data. Faculty members from all 3 colleges facilitated the workshop and modeled interprofessional collaboration, ensuring that the workshop met the academic goals of all 3 disciplines collectively. Prior to the workshop, students were assigned to equally balanced interdisciplinary teams comprised of 1 student each from pharmacy, nursing, and medicine. Students worked in groups through the 2 problem-based cases on chronic respiratory diseases. This exercise included evaluative questions from each of the 3 disciplines. The hidden curriculum involved students teaching each nother about the medical, pharmacy and nursing aspects of chronic obstructive pulmonary disease and asthma in this small-group setting.
During this time, a third of the student cohort (16 teams) were brought, en masse, to examination rooms to assess, diagnosis, and develop treatment plans for a standardized patient with pneumonia. In preparation for this event, the standardized patients underwent intensive training on the disease state they were presenting with, along with training on evaluating teamwork, provided by the director of AMS’s standardized patient program. Faculty members at AMS developed a teamwork global rating scale based on a validated evaluation instrument. The instrument was adapted specifically to meet the needs of the IPE curriculum described in this paper and focused on team communication and performance.16
Faculty members remained in the room as students navigated through the standardized patient encounters. Based on our teamwork global rating scale, standardized patients and faculty members evaluated how effectively the student teams worked together. Faculty members and standardized patients also noted who took the lead in the following areas: patient medical history, physical examination, vital signs, interpretation of a chest x-ray, and communication of a care plan with the patient. We also asked the standardized patients to rate their level of comfort with the care provided by the team.
Students were asked to complete a voluntary questionnaire prior to the workshop and immediately after its completion. Constructed on the basis of previous research, this questionnaire assessed students’ attitudes toward interdisciplinary education.15 Students were also surveyed after the standardized patient encounter about their experiences as participants in the teamwork exercise. The survey tool was reviewed and approved by URI’s Institutional Review Board.
EVALUATION AND ASSESSMENT
Analyses were conducted on the data produced by the student pre- and post-workshop survey instruments, student post-standardized-patient encounter survey instruments, and faculty and standardized-patient evaluations using the teamwork global rating scale. To measure and test for differences in student attitudes before and after the workshop, differences in centers of distribution (means and medians) were analyzed. The paired t test was used to look for a difference in means, while the nonparametric signed rank test was used to look for a difference in medians. A 2-tailed alpha level of 0.05 was set as the criterion for significance. We performed all statistical analyses using Microsoft Excel (Version 2010, Redmond, WA) and SAS (version 9.3, SAS Institute, Cary, NC).
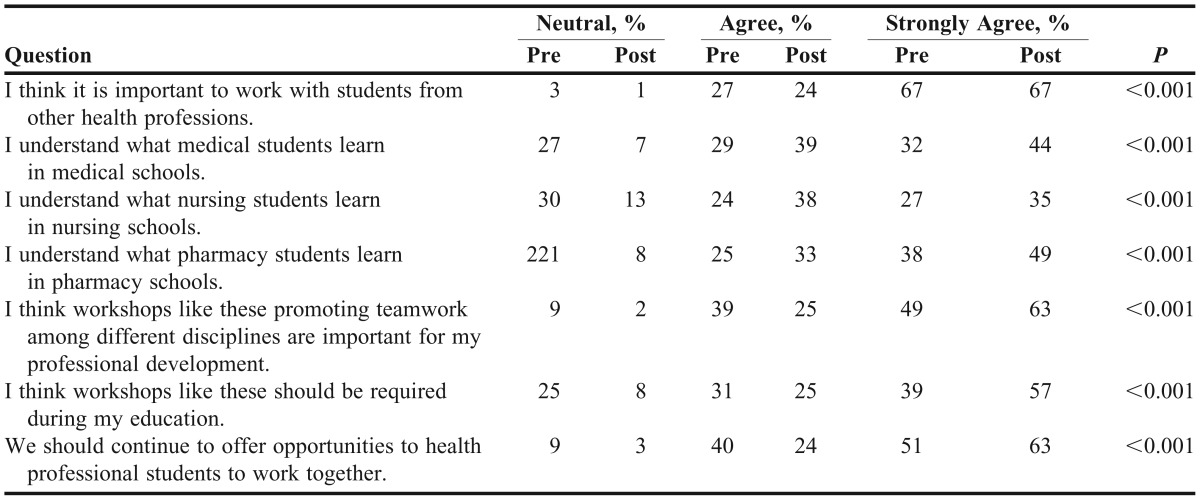
Of the 251 students who participated in the workshop, 232 students completed all the questions on the pre- and post-survey instrument, resulting in an overall response rate of 92.4%. The sample set consisted of 101 (40.2%) third-year pharmacy students, 67 (26.7%) fourth-year nursing students, and 83 (33.1%) second-year medical students. Table 1 describes the students’ demographic characteristics.
Table 1.
Demographic Characteristics of Students Participating in a Multidisciplinary Team Patient Care Workshop
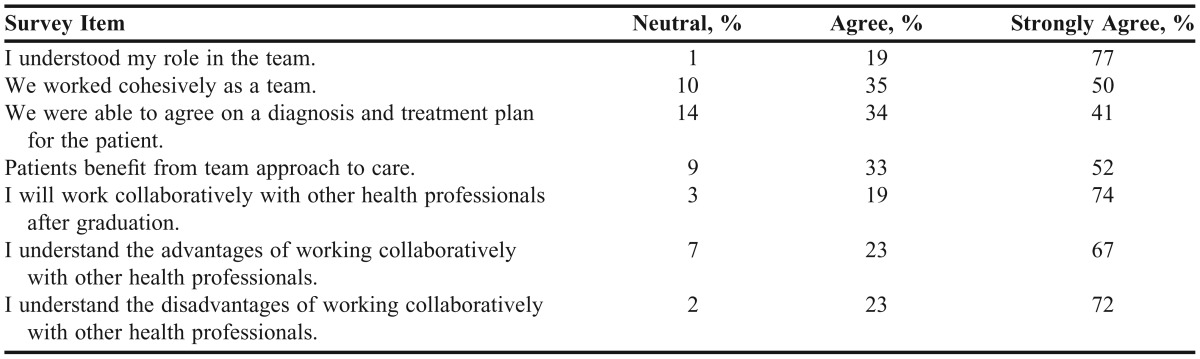
An analysis of prior student experience with interprofessional collaboration showed that approximately 61% of students who participated in the workshop had no previous experience working with other health professionals, 43% had no prior experience working in teams, and 80% had observed their mentors working with professionals from other health professions. Statistical analysis of the pre- and post-workshop responses on the student questionnaire demonstrated a significant change related to the students’ perceptions of their ability to describe the nature of the education being provided in the other 2 disciplines. The responses also indicated an improvement in their level of comfort with being part of healthcare teams and their perception of the value of such workshops to their learning. Table 2 presents a summary of the results of the survey tool analysis.
Table 2.
Comparison of Student Perceptions of Collaboration Among Healthcare Professionals Before (Pre) and After (Post) Participating in a Multidisciplinary Patient Care Workshop
After the workshop, approximately 67% of students strongly agreed that it was important to work with students from other health professions. Students also reported better knowledge of other health care disciplines as a result of the workshop: approximately 84% of students better understood what medical students learn in medical school following the workshop; 74% better understood what nurses learn in nursing school, and 82% better understood what pharmacists learn in pharmacy school. The results of the post-workshop survey were all significantly different (p<0.001) from preworkshop results. After the interdisciplinary workshop, there was a significant increase in the percentage of students who strongly agreed that workshops promoting the idea and experience of teamwork with other healthcare professionals could prove invaluable in the professional development of the students (preworkshop, 49%; post-workshop, 64%; p<0.001). Based on an analysis of student perceptions regarding the requirement of such workshops in their education, a majority strongly agreed that these workshops should be required (preworkshop, 39%, post-workshop, 57%; p<0.001). There was also a significant increase in the number of students who strongly agreed the health professional schools should offer workshops in which healthcare professionals could work together (preworkshop 51%; post-workshop 64%; p<0.001). The results were similar when the data were analyzed using the nonparametric Wilcoxon signed rank sum test, as all the questions demonstrated a significant improvement.
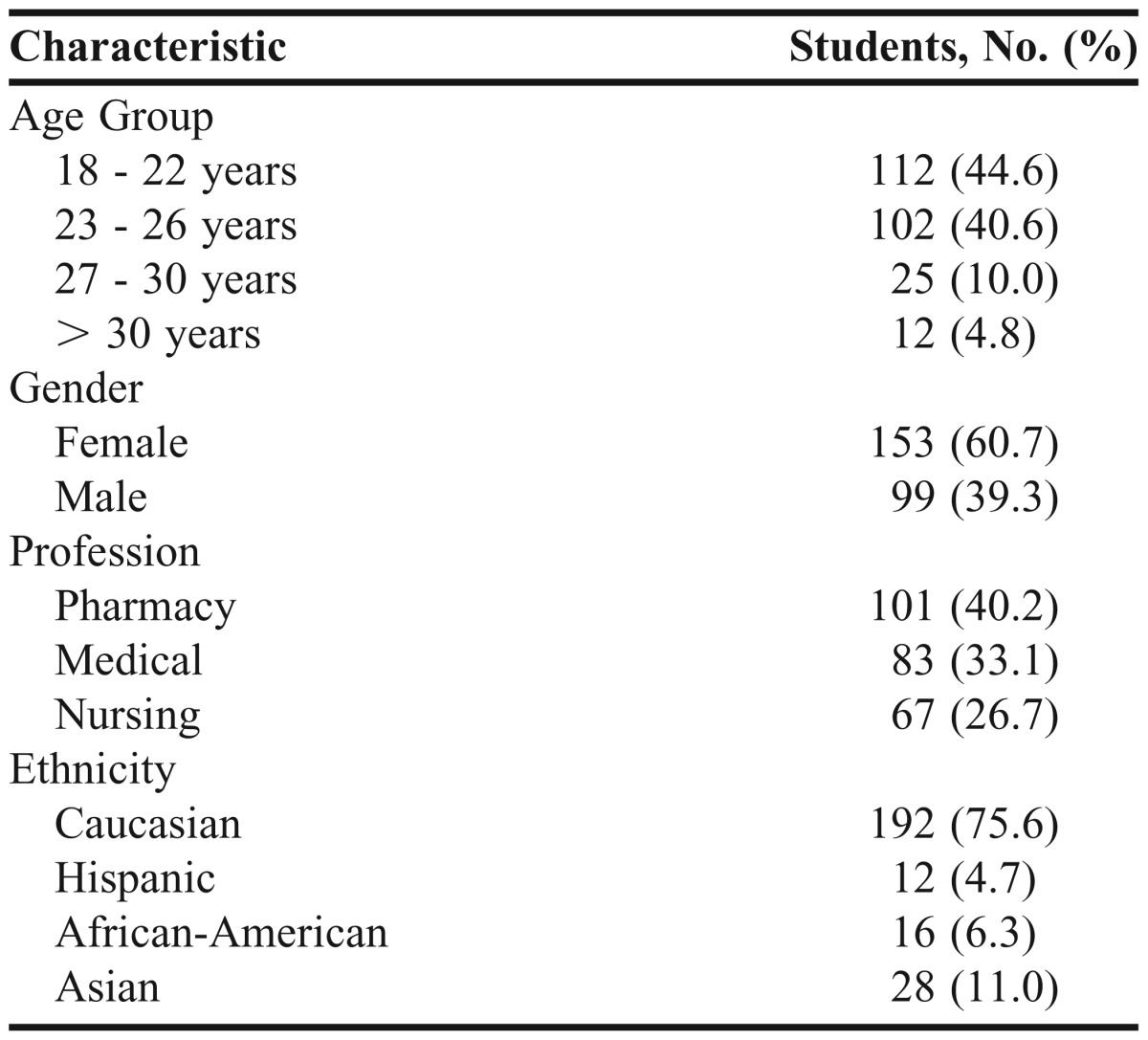
Table 3 outlines the results of the post-workshop standardized patient survey instrument. Approximately 77% of the students strongly agreed that they had an understanding of their role on the healthcare team. A majority of the students (85%) reported working cohesively as a team, and 75% of the students were satisfied with the level of agreement among the different team members regarding diagnosis and treatment of the patient. A majority (52%) strongly believed that the patient would benefit from such an interprofessional team approach to healthcare delivery, and 74% had a positive perception regarding collaborating with other healthcare professionals in the future. Most students (67% and 72%, respectively) demonstrated an understanding of the advantages and disadvantages of working in a team with other healthcare professionals.
Table 3.
Results of Student Survey Results Following the Standardized Patient Encounter
Faculty members and standardized patients both evaluated the tasks performed by individual students in the patient encounter. Table 5 summarizes what percentage of medical, nursing, and pharmacy students assumed the lead in taking a history, performing a physical examination, taking vital signs, interpreting a chest x-ray, discussing with a patient the diagnosis and discussing the plan with a patient as part of the standardized patient exercise.
Table 5.
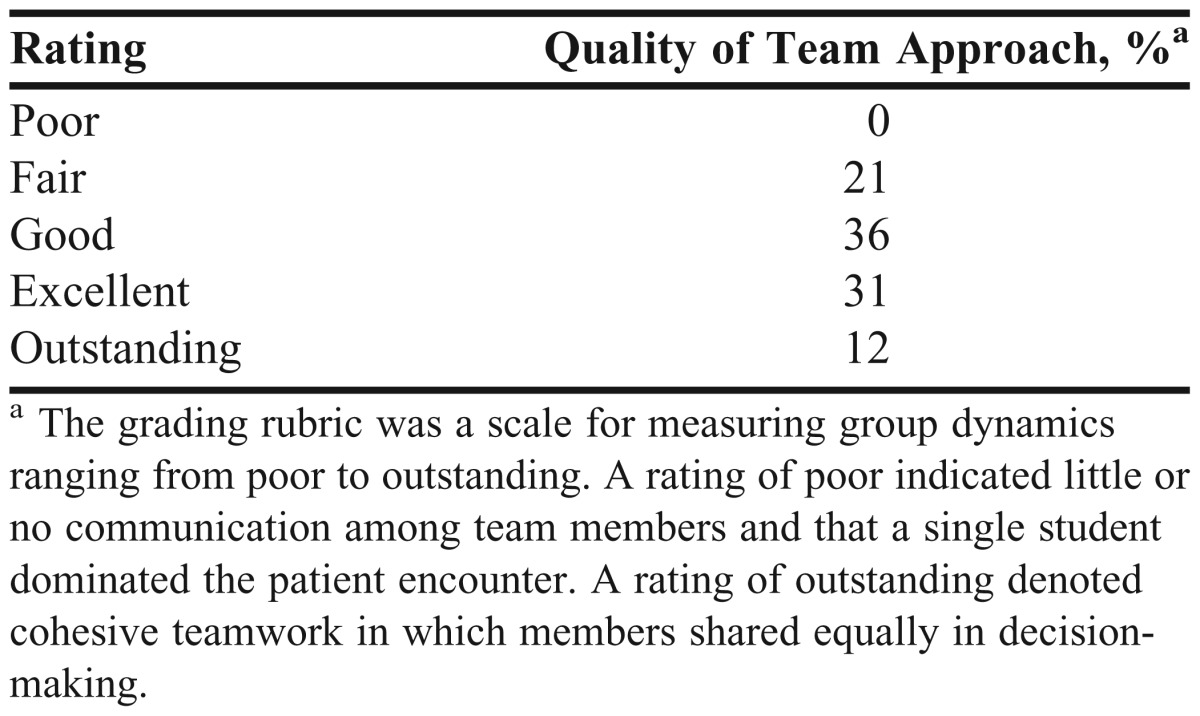
Teamwork Scores Based on Evaluation by Standardized Patients and Faculty Members Using the Teamwork Global Rating Scalea
We also analyzed who carried out certain functions on each team in the standardized patient encounter (Table 4). Medical students took the lead in performing the history, conducting physical examinations, and interpreting chest x-rays; nursing students took the lead in taking vital signs; and all 3 groups of health professional students contributed to the development of a diagnosis and treatment plan in the standardized patient encounter.
Table 4.
Standardized Patient and Faculty Evaluation of Team Member Involvement, by Discipline
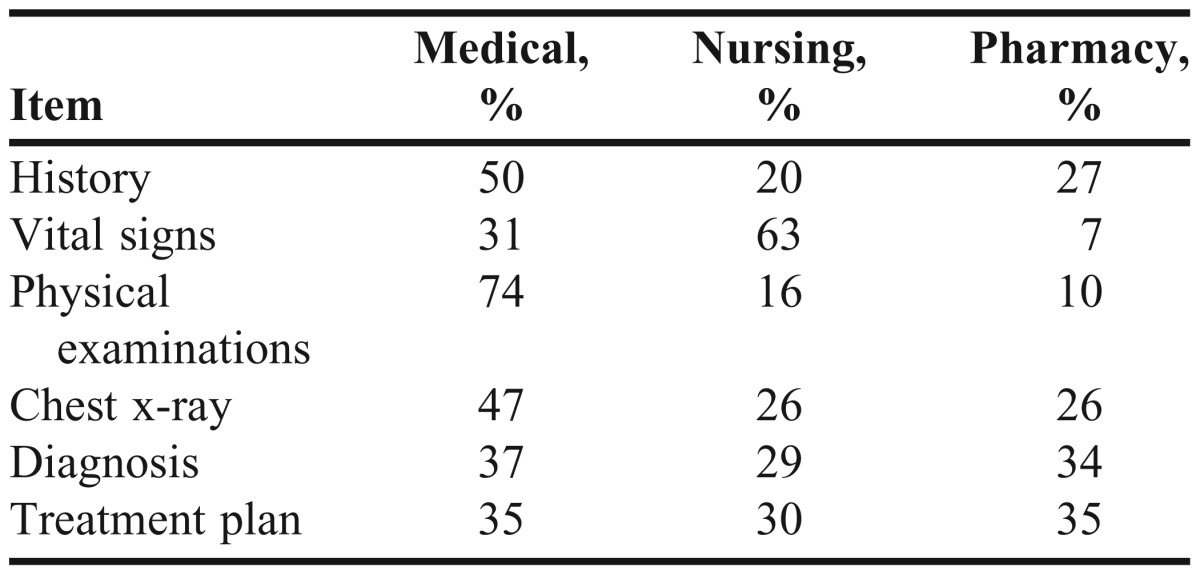
Table 5 details the results of the teamwork global rating scale. The students were evaluated based on a grading rubric that rated team dynamics. The scale included ratings of poor, fair, good, excellent and outstanding. A rating of poor indicated the team demonstrated little or no communication with each other and that a single student dominated the patient encounter. A rating of outstanding denoted that the students worked cohesively as a team, sharing equally in decision-making. Approximately 79% of student teams earned a rating of good or better in the standardized patient encounter.
DISCUSSION
The results of our study demonstrate that after a 1-day workshop, students of 3 different health professional disciplines valued IPE in their training and could effectively work as a team in taking care of patients. Additionally, students gained an increased understanding of the expertise of healthcare professionals in other disciplines and believed that the IPE curriculum should be integrated into health professions curricula.
The standardized patient exercise, in particular, demonstrates that students are able to share the responsibilities of patient care. A principal goal of this exercise was for students from all 3 disciplines to participate actively in developing a healthcare plan for the patients. More importantly however, the data also reveal that students were able to function as a team, even with little prior interprofessional experience or familiarity with each other.
Our IPE curriculum is unique for several reasons. It unites the efforts of a private institution (AMS) with those of a state institution (URI), the campuses of which are separated by 20 miles. The development of the IPE curriculum involved 3 separate administrations and had to be designed to incorporate 3 separate curricula. The interprofessional collaboration curriculum blended a low-fidelity simulation (the problem-based learning cases of chronic obstructive pulmonary disease and asthma) with a high-fidelity simulation (the standardized patient case of pneumonia), and after the curriculum was delivered, significant changes were seen in students’ attitudes, knowledge, and skills. Finally, because our curriculum has been rigorously developed over the past 4 years, we believe it is ready for use at other institutions with minimal planning or adaption.
There are several limitations to our study. Although our data collection instruments were based on validated tools, the adaptations made to suit our curriculum evaluation needs limit the validity of our results. Additionally, we looked only at immediate changes in attitudes, knowledge, and skills following the workshop; thus, we do not have long-term data on which to base an assessment of the efficacy of intervention. Future studies could be designed to track the cohort of students who participated in interprofessional programs early in their education, with the primary endpoint being measurable positive outcomes on patient care. Another area for future examination is whether the team approach that was demonstrated in our controlled and safe environment would extend throughout the respective discipline’s training of students and continue into their practice.
CONCLUSIONS
The results of this introductory interprofessional exercise were positive. The students overwhelmingly approved of the interdisciplinary team-based learning approach and verified that, at the workshop’s conclusion, students from each of the disciplines had a greater understanding of the others’ knowledge and skills. We believe that student experiences such as this foster interdisciplinary trust and the communication skills necessary for the effective participation of future healthcare providers as active members of multidisciplinary patient-care teams. As healthcare educators, we have overcome many of the barriers that have the potential to derail collaborations such as this. Not only is this unique instructional design included as part of the recognized curricula of URI’s Colleges of Nursing and Pharmacy, it is also now incorporated into the second-year doctor of medicine curriculum at Brown’s Medical School.17 Our initiative clearly demonstrates the promising impact that a preliminary interprofessional program has on students.
REFERENCES
- 1.Learning Together to Work Together for Health. Report of a WHO Study Group on Multiprofessional Education for Health Personnel: The Team Approach. World Health Organization;1988. 769;1-72. [PubMed]
- 2.Summit CotHPE. Health Professions Education: A Bridge to Quality. The National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Framework for Action on Interprofessional Education and Collaborative Practice, World Health Organization. 2010:63. [PubMed] [Google Scholar]
- 4.Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. 2011 https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed May 5, 2012. [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education standards for duty hours. Common program requirements. July 2011 www.acgme.org/acwebsite/home/Common_Program_Requirements_07012011.pdf. Accessed May 5, 2012. [Google Scholar]
- 6.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: Report of an expert panel. 2011 http://www.aacn.nche.edu/education-resources/ipecreport.pdf. Accessed May 5, 2012. [Google Scholar]
- 7.Solomon P, Salfi J. Evaluation of an interprofessional education communication skills initiative. Educ Health (Abingdon). 2011;24(2):616. [PubMed] [Google Scholar]
- 8.Curran VR, Mugford JG, Law RM, MacDonald S. Influence of an interprofessional HIV/AIDS education program on role perception, attitudes and teamwork skills of undergraduate health sciences students. Educ Health (Abingdon). 2005;18(1):32–44. doi: 10.1080/13576280500042606. [DOI] [PubMed] [Google Scholar]
- 9.Buczacki S, Shalhoub J, George PM, Vearncombe LM, Byrne PD, Alazawi W. Benefits of knowledge-based interprofessional communication skills training in medical undergraduate education. J Royal Society Med Short Reports. 2011;2(8):67. doi: 10.1258/shorts.2011.011065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vrontos EB, Kuhn CH, Brittain KL. Impact of interprofessional activities on health professions students' knowledge of community pharmacists' role and services. Am J Pharm Educ. 2011;75(8):152. doi: 10.5688/ajpe758152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson J, Bandali K. Bridging the gap: Enhancing interprofessional education using simulation. J Interprof Care. 2008;22(5):499–508. doi: 10.1080/13561820802303656. [DOI] [PubMed] [Google Scholar]
- 12.Dillon PM, Noble KA, Kaplan L. Simulation as a means to foster collaborative interdisciplinary education. Nursing Educ Perspec. 2009;30(2):87–90. [PubMed] [Google Scholar]
- 13.Reese CE, Jeffries PR, Engum SA. Learning together: Using simulations to develop nursing and medical student collaboration. Nursing Educ Perspec. 2010;31(1):33–37. [PubMed] [Google Scholar]
- 14.Mann KV M-DJ, Martin-Misener R, Clovis J, Rowe R. Interprofessional education for students of the health professions: the “Seamless Care” model. J Interprof Care. 2009;23(3):224–233. doi: 10.1080/13561820802697735. [DOI] [PubMed] [Google Scholar]
- 15.MacDonnell CP JA, Lavin M, Cohen S, Cohen L. Impact of an Interdisciplinary Practice Laboratory on Pharmacy and Nursing Students’ Perceptions of Health Care Roles. Int J Pharm Educ Pract. 2011;7(1) http://www4.samford.edu/schools/pharmacy/ijpe/index.htm. Accessed May 5, 2012. [Google Scholar]
- 16.Wright MC, Phillips-Bute BG, Petrusa ER, Griffin KL, Hobbs GW, Taekman JM. Assessing teamwork in medical education and practice: relating behavioural teamwork ratings and clinical performance. Med Teach. 2009;31(1):30–38. doi: 10.1080/01421590802070853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gurpusso P DR, Dumenco L, et al. The Warren Alpert Medical School of Brown University. Acad Med. 2010;85(9):S 520–524. doi: 10.1097/ACM.0b013e3181ea67ef. [DOI] [PubMed] [Google Scholar]