Abstract
Background
Surgical treatment of spinal deformities in Duchenne muscular dystrophy (DMD) is influenced by a number of factors which have proven to be a difficult challenge. Each case should be carefully evaluated, considering not only the natural history of the spinal deformity, but also the patient’s general condition. These should be thoroughly assessed through clinical and radiographic investigations together with other medical specialists. Life expectancy should be determined according to the cardio-respiratory function, and both preoperative and postoperative quality of life should be taken into consideration, trying to imagine the functional status of each patient after surgery.
Methods
From February 1985 to February 2000, 58 patients with spinal deformity in DMD were surgically treated. Of 25 patients that were operated on between 1985 and 1995, only 20 were followed-up after 5 years because 5 of them had died during this time. Therefore, the present study focuses on the results obtained in 20 cases. The 20 cases reviewed presented with a mean angular value of scoliosis equal to 48° (range 10–92°). Spinal fusion with our modified Luque technique [6] was performed in 19 cases, whereas CD instrumentation was applied in only one case.
Results
At the 5 year follow-up (range 5.6–10 years), the age ranged from 18 to 24 years and averaged 20.4 years. The postoperative angular value of scoliosis averaged 22° (58%, range 0–43°), the mean correction at follow-up was 28° (range 0–60°), and the mean loss of correction was equal to 6° (range, 0–11°). Vital capacity showed a slow progression, slightly inferior to its natural evolution in untreated patients. The severest complication was the death that occurred in one of the patients.
Conclusions
According to the present study, an early surgery (angular value lower than 35–40°) dramatically reduces the rate of risk factors associated with spinal deformities in DMD, and its advantages far exceed the disadvantages, above all in terms of quality of life.
Keywords: Duchenne muscular dystrophy, Scoliosis, Vital capacity, Arthrodesis
Introduction
A spinal deformity is almost never observed in children with Duchenne muscular dystrophy (DMD) who can walk [48], and therefore its onset is usually registered between the ages of 12 and 13 years and rarely before the age of 11. Numerous factors are responsible for the onset of the deformity. According to Gibson and Wilkins [22] the main cause of spinal deformity is the paralysis of the extensor muscles.
Rideau [44], Siegel [48] and Dubousset [10, 11] considered the inclination of the pelvis to be the major cause of the deformity—in particular the asymmetry of the scar retractions at level with the lower limbs. Ledoux [30] focused on the position usually maintained by the wheelchair-bound patient when he/she frees and uses his/her dominant hand: concluding that such a posture would determine the permanent spinal curve.
Regardless of the mechanisms responsible for the onset of the deformity, it is important to know that its progression cannot be stopped in more than 90% of patients with DMD [16, 19, 42, 46]. From the onset, progression can be extremely rapid (Fig. 1) and in all cases seriously affects the unsupported sitting ability and deteriorates the respiratory function, already compromised by the disease [18, 21, 22, 27, 49].
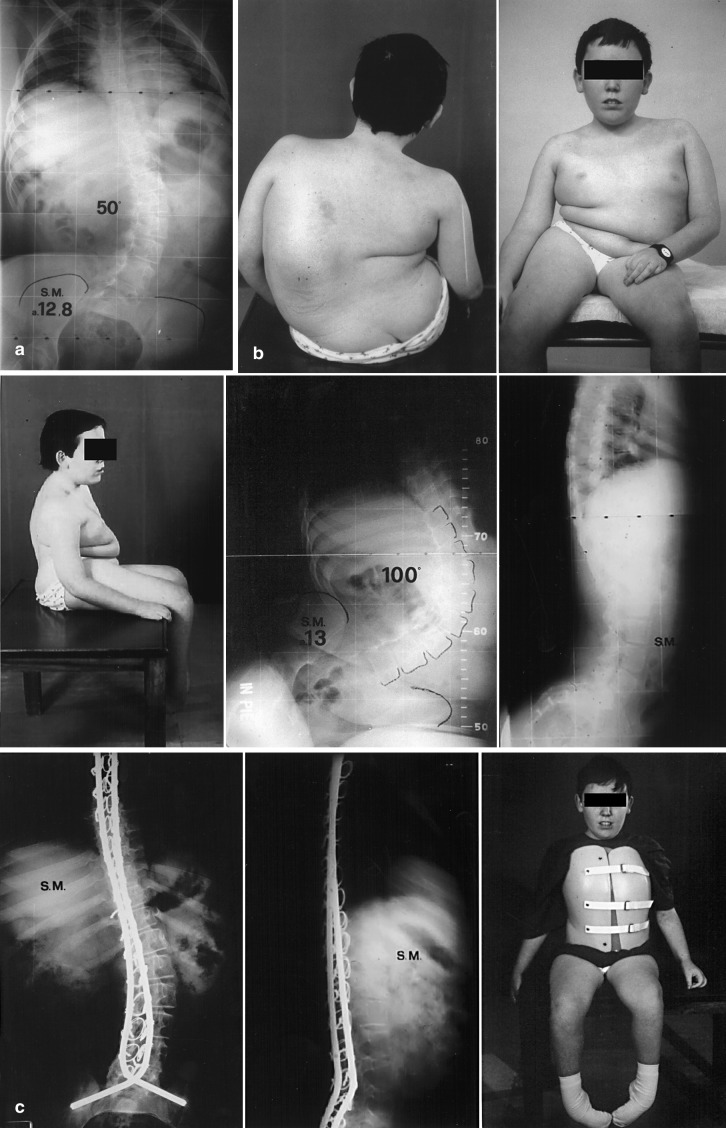
Fig. 1.
a Patient aged 12 years and 8 months with DMD. He stopped walking at the age of 9 years. b Very rapid worsening of spinal deformity within only 4 months. Clinical and radiographic picture. c After surgery, the patient wore an orthopaedic brace for 3 months while sitting. The surgery was performed by the Luque technique. The follow-up was at 5 years
Kurz et al. [29] observed a 4% decrease in vital capacity (VC) for every 10° progression of the curve in patients with DMD. According to Galasko et al. [17, 18], VC decreases by 8% per year in patients with scoliosis secondary to DMD. No brace can prevent the progression of this kind of spinal deformity. Nonoperative treatment can only be considered as an acceptable compromise in exceptional cases: when the patient refuses surgery or when the patient comes to us with a very seriously advanced deformity and general health has begun to collapse [14, 25, 34].
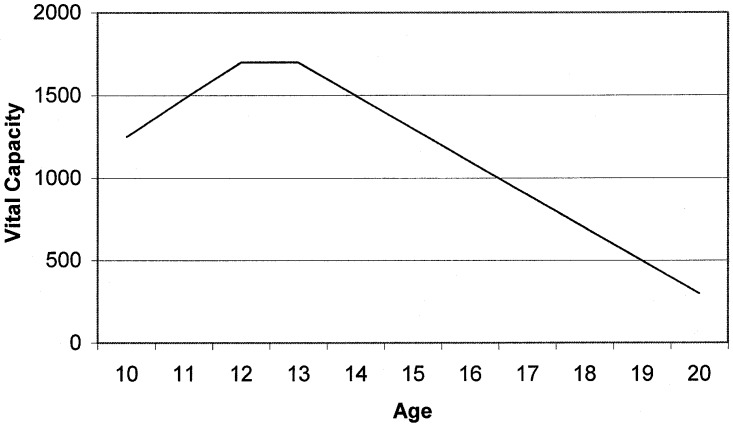
It is absolutely necessary to assess VC in order to evaluate a prognosis. Rideau et al. [44] classified patients with DMD into three groups by their VC. They asserted that VC increases until the age of 10–12 years, until a plateau is reached; then it progressively decreases over the following years (Fig. 2). The knowledge of this plateau VC value allows a prognosis of the restrictive pulmonary syndrome to be made.
Fig. 2.
Natural evolution of the VC by age in patients with DMD according to Rideau. The most appropriate time to perform surgery is between the age of 12 and 13 years
The first type (VC<1,200 ml) is characterised by a bad prognosis. The deformity is very severe and progresses rapidly. Death occurs before the age of 18 years. The second type (VC 1,200–1,700 ml) is characterised by a bad prognosis, too, but death occurs between the ages of 18 and 22 years. The third type (VC>1,700 ml.) has a better prognosis: spinal deformity occurs later and progresses more slowly. These patients have a longer life expectancy.
According to the present literature review, 48 patients with spinal deformity in DMD were treated using the Harrington technique [22, 24, 35, 45, 52, 54] during the 1970s. About half of the cases encountered mechanical complications [35], and the long immobilisation period in plaster cast was responsible for many general problems.
Since 1980, 208 cases of patients who were treated by sublaminar wiring have been reported in the literature [2, 3, 4, 5, 9, 10, 12, 17, 31, 35, 38, 39, 44, 47, 50, 51]. The authors reported a mean correction of deformity on the frontal plane equal to 50%, and only the severest cases required postoperative immobilisation. The advantages of surgery that they described include increased comfort and sitting tolerance [1, 2, 4, 5, 13, 32, 35, 38, 43, 44, 47, 55], cosmetic improvement [2, 38], no need for orthopaedic braces [2, 8, 37, 40], easier nursing care by parents [2, 7] and pain relief [2, 15, 38].
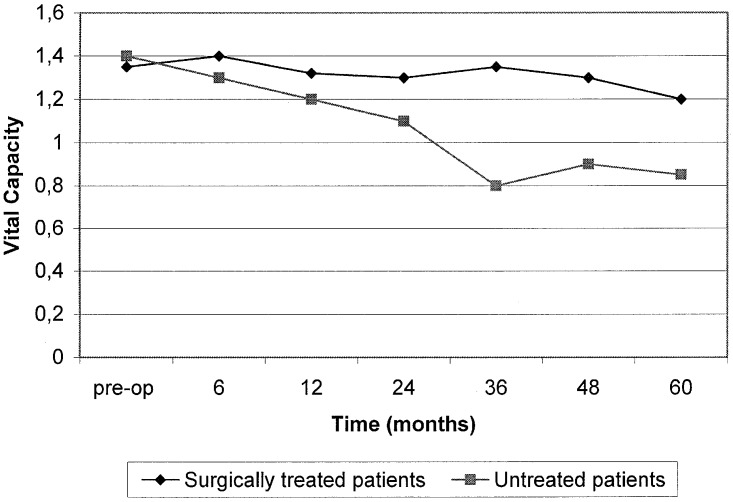
The effects of spinal surgery on respiratory function and life expectancy are still controversial. According to many authors, spinal fusion has no effects on the natural involution of the respiratory function [5, 33, 35, 36, 47], both at short-term and at a 5-year follow-up [38]. In contrast, Rideau et al. [44] and Galasko et al. [17] reported a period of VC stabilisation in surgically treated patients of 24 and 36 months, respectively (Fig. 3).
Fig. 3.
In patients with DMD and surgically treated by spinal fusion, VC is stable for about 3 years and then tends to decrease at a markedly lower rate compared to untreated patients [15]
Regarding life expectancy, Galasko [17] observed a significantly higher rate of mortality in untreated versus surgically treated patients; however, other authors [5, 7, 20, 28, 36] stated that spinal surgery does not improve life expectancy. Of the 208 patients treated with sublaminar wiring and reported in the literature, 3 died during surgery or on the following day, and 43 died during an average time interval of 4 years after surgery. The purpose of the present report is to assess the surgical results achieved in patients with DMD at a minimum follow-up of 5 years.
Materials and methods
From February 1985 to February 2000, we surgically treated 58 patients with spinal deformity in DMD. Twenty patients were followed up at a minimum of 5 years. Therefore, results obtained in 20 cases are reported. In all of the cases, the diagnosis was primarily based on familial history, as well as on clinical, haematochemical and bioptical data. All of the patients had stopped walking before the age of 13 years. The average age at surgery was 13 years (range 11.8–15 years). The 20 cases that were reviewed presented with a mean angular value of scoliosis equal to 48° (range 10–92°).
The site of the scoliosis was thoracolumbar in 18 cases and lumbar in 2. In 15 cases, scoliosis was associated with thoracolumbar kyphosis with a mean angular value of 40° (range 21–75°). In 3 cases, scoliosis was associated with lordosis and had a mean angular value of 112° (range 90–135°). In the 2 remaining cases, there was only scoliosis.
In 18 patients, pelvic obliquity averaged 22° (range 10–36°). In the 2 remaining cases, there was no pelvic obliquity. Preoperative average VC was 1,668 ml (range 810–2,240 ml). Of 20 patients, 13 showed echocardiographic disorders.
Spinal fusion was performed in 19 cases using our modified Luque technique [6] (the technique used by us involves the use of two 5 mm rods correctly moulded both on the frontal and sagittal plane (maintaining the lumbar lordosis) and fixed to the spine with 0.9 mm wires passed through each spinal level.
Meanwhile, we have modified the pelvic fixation. We initially used the Luque technique: the short part of the L rod was inserted into the ileum without any anchorage and this often resulted in the short part of the L rod falling out. In the second phase, we crossed the two L rods at the lumbosacral junction, fixing the cross with a sublaminar wire. This method became more complex than the previous method but the stability of the fixture was assured. Now we do not cross the rods as previously described, but we fix them with one or two DTT at the level of the lumbosacral junction: this prevents the short part of the L rod falling out), while the CD instrumentation was applied only in one case (Fig. 4a,b).
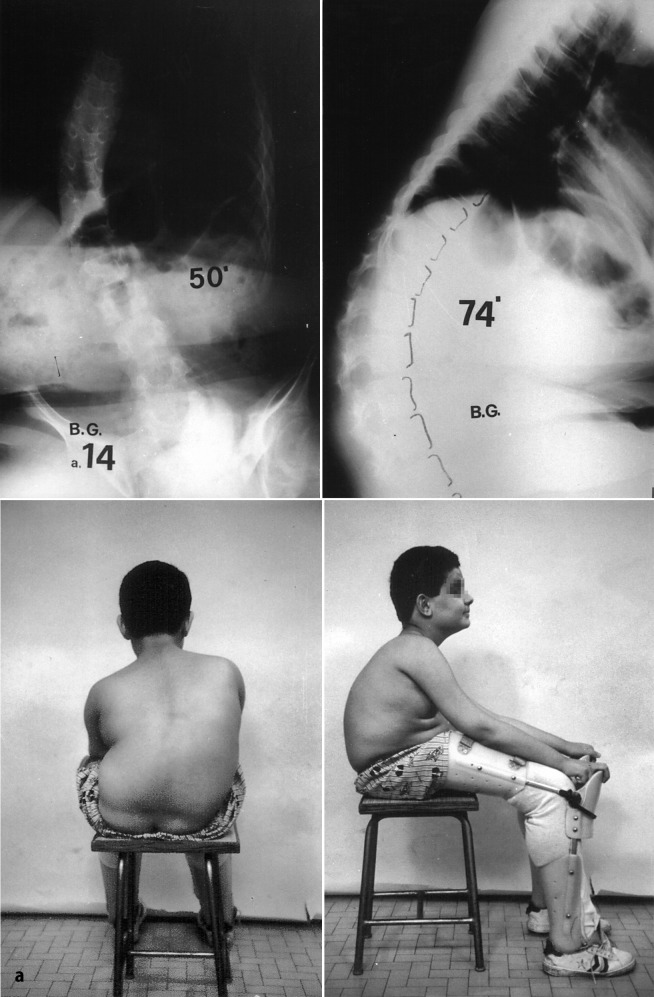
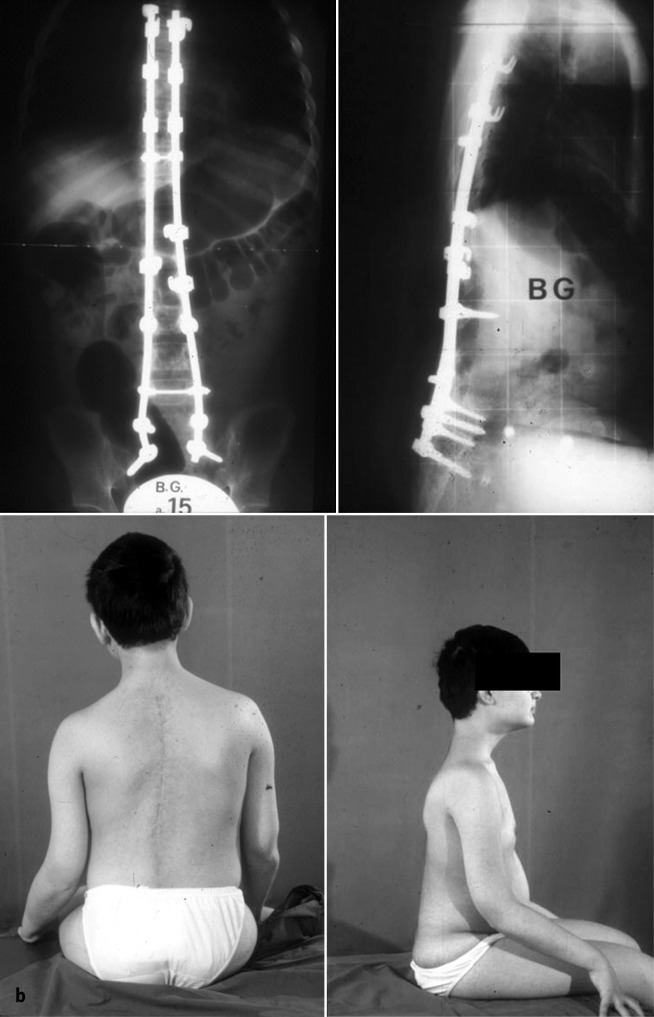
Fig. 4.
a 14-year-old patient with kyphoscoliosis in DMD. He is loosing his ability to walk. b Spinal fusion with CD. Clinical and radiographic picture after 7 years
Fusion was extended from the first 3 thoracic vertebrae to the sacrum in all of the cases. Autologous bone graft from the spinous processes was always used together with abundant bank bone. Surgery lasted 3 h on average (range 2.30–4.15 h). Blood losses averaged 1,200 ml (range 700–1,600 ml). Intraoperative blood recovery was performed in 6 cases.
Postoperatively, 17 patients required intensive care unit management for an average period of 48 h (range 20–62 h), and 3 patients returned to the ward. Patients could sit with no immobilisation as of postoperative day 5–6 and after careful radiographic evaluation. They were discharged from the hospital on postoperative day 9–10 and had to wear an orthopaedic brace during the day for about 3 months (range 1–5 months). Physiatric treatment for rehabilitation was prescribed.
At the last follow-up (over 5 years), patients were assessed by clinical evaluation, respiratory test, and radiographic evaluation of the spine (anteroposterior and laterolateral views in the sitting position plus 2 oblique views of the lumbosacral tract). Moreover, patients were given a questionnaire about their quality of life and the advantages and disadvantages of surgery.
Results
At a follow-up greater than 5 years (range 5.6–10 years), patient mean age was 20.4 years, ranging from 18 to 24 years. The postoperative angular value of scoliosis averaged 22° (range 0–43°), the mean angular value at follow-up was 28° (range 0–60°), and the mean loss of correction was equal to 6° (range 0–11°). Kyphosis and lordosis were corrected to 24° (range 10–45°) and 48° (range 32–75°), respectively and were stable over time. At follow up, there was no loss of correction in respect of postoperative value.
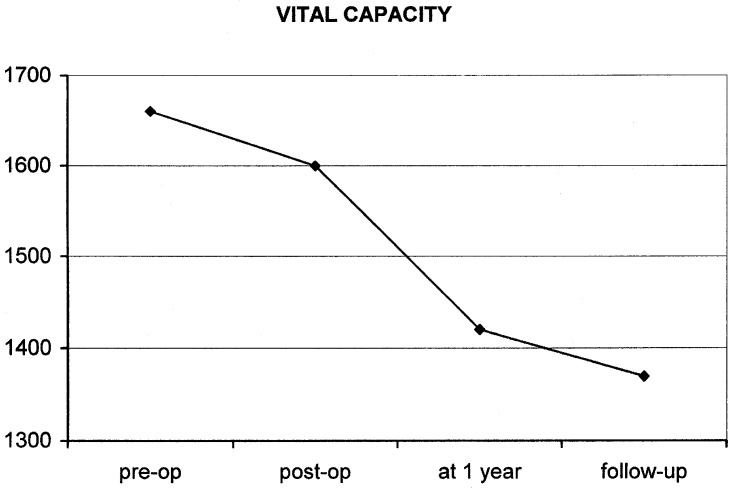
Pelvic obliquity was significantly corrected to 10° (range 0–22°), with a modest loss of correction at follow-up (but only in those cases with scoliosis greater than 50°). The worsening of the VC showed a slow progression, slightly inferior to the natural evolution of the respiratory function in untreated patients. At last follow-up, VC was 1,380 ml (range 300–2,200 ml) (Fig. 5).
Fig. 5.
Preoperative average trend of VC until the last follow-up
Eighteen patients showed good balance of head and trunk; in 2 cases head balance was precarious and required forward flexion of the trunk. Patients’ and parents’ responses to the questionnaires were more than satisfactory. All of the patients gained improved sitting endurance, and reported improved life quality and cosmetic appearance. All except one (who regretted missing some months of school lessons) asserted that they would undergo surgery again. The parents were, above all, satisfied with the easier nursing care and wheelchair transport.
The most severe complication occurred in one of the patients who died. This 14-year-old patient was a Jehovah’s witness who weighed 54 kg and presented with scoliosis of 40°, VC of 1,470 ml (87% of theoretical values) and a normal echocardiogram. At the end of surgery, the patient had a cardiac arrest, probably ascribable to haemodilution during blood recovery.
The other complications included a neurogenic bladder that resolved after 1 year, a sacral decubitus and three painful prolapses of the horizontal part of the rod from the pelvis which required normalisation in local anaesthesia in 1, 4 and 5 years respectively.
Discussion
The knowledge of the natural history of this disease, the patient’s clinical picture [41], the short life expectancy, and the inexorable progression of spinal deformity preventing any sitting position in spite of orthopaedic braces, all recommend an early surgery in young patients who present with the most appropriate conditions to tolerate it well [23, 26].
Nowadays, according to the current authors, the indication for surgery should be given when the patient is aged 10–12 years, has a VC higher than 50% of the theoretical values, shows no cardiac alterations and presents an angular value of scoliosis lower than 30–35°. Under these conditions, surgery is easier and shorter and therefore involves lower risks.
From our experience of 15 years of spinal deformity surgery, the following advantages of an early surgery emerged: (1) higher percentage of correction of the deformity; (2) better trunk balance and (3) no recurrent pelvic obliquity, not even partial obliquity. As far as the respiratory function is concerned, there is less optimism: those patients who underwent early surgical treatment also showed a decrease in VC which was slightly lower than that of untreated and later treated patients [2, 36].
Subsequently, most authors think that the main cause of the respiratory deficit is not to be found in the evolution of the deformity, but in the severe worsening of muscular strength, which is typical of such disease. However, we do not completely share this point of view: sooner or later, the untreated patient loses his ability to sit and spends the rest of his life confined to his bed. Since the spinal deformity is neuromuscular (which generally means very flexible), the spine tends to get straight when lying down and becomes similar to a treated spine—which therefore eliminates the relation between VC and spinal deformity.
We believe that these circumstances (which are not highlighted in the literature) are extremely important: VC trend cannot be assessed in treated versus untreated patients, without stressing that those patients who refused surgery lost their capacity to sit after a certain time due to the progression of the deformity.
Needless to say that spinal collapse in the sitting position in patients with DMD does nothing but increase the restrictive respiratory deficit, thus compromising VC severely. That could be the reason why surgery does not increase life expectancy in patients with DMD according to most of the literature [5, 33, 35, 36, 47]. Therefore, it has turned out that the only important goal of spinal surgery in DMD is to improve the quality of life of these patients.
Conclusions
The presence of a spinal deformity in DMD almost always requires surgery. The only reason for not treating a deformity is a late presentation associated with very poor patient conditions, which make surgical treatment impossible. Since we know the natural history of neuromuscular scoliosis and are aware of the damage caused by orthopaedic braces (which cannot stop the evolution of the deformity), we would recommend surgery as early as possible, before the deformity gets too severe and too risky.
We consider 10–11 years as the best age range for performing a definite fusion without compromising the spinal growth [53]. If the deformity progresses too rapidly during the first years of life, it is better not to wait for its further progression. An early surgical subcutaneous distraction should be carried out in order to correct the deformity, prevent the rapid decrease of VC and reach the appropriate age for final fusion in good conditions.
DMD is a progressive disease with short life expectancy. In these cases surgery should ensure a stable correction of the deformity, with good head and trunk balance on the pelvis, which should be restored to the horizontal position as much as possible; however, the trend of the respiratory function cannot be significantly modified and life cannot be lengthened. Since we are aware of the quality of life in untreated patients, we feel compelled to perform surgery whenever possible and as early as possible.
In our opinion, the Luque technique with fusion is now the treatment of choice: it ensures a satisfactory, stable and durable correction of the deformity with good restoration of trunk balance. Additionally, this procedure requires reduced operative time. Postoperative external immobilisation (bracing) takes little time and averages about 3 months: no inconvenience occurred in this period of time in any of the surgically treated patients of the present series.
The postoperative brace is not compulsory but does reduce the pain due to the incision and the spinal correction. Our modified pelvic fixation [6] allowed us to dramatically reduce the incidence of mechanical complications and achieve a stable correction of pelvic obliquity in cases operated on very early.
Acknowledgements
We would like to thank “Telethon” for supporting this project with research funds (no. 1165C)
References
- 1.Alman J Bone Joint Surg Br. 1999;81:821. doi: 10.1302/0301-620X.81B5.9383. [DOI] [PubMed] [Google Scholar]
- 2.Bellen J Orthop Surg. 1993;7:48. [Google Scholar]
- 3.Bradford DS (1987) Neuromuscular spinal deformity. In: Bradford DS, Lonstein JE, Moe JA, Winter RB (eds) Moe’s textbook of scoliosis and other spinal deformities, Saunders, Philadelphia, pp 284–296
- 4.Bridwell Spine. 1999;24:1300. doi: 10.1097/00007632-199907010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Cambridge J Pediatr Orthop. 1987;7:436. doi: 10.1097/01241398-198707000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Cervellati Prog Pat Vert. 1995;18:17. [Google Scholar]
- 7.Chataigner Rev Chir Orthop Reparatrice Appar Mot. 1998;84:224. [PubMed] [Google Scholar]
- 8.Colbert Arch Phys Med Rehabil. 1987;68:302. [PubMed] [Google Scholar]
- 9.Drennan JC (1984) Surgical management of neuromuscular scoliosis. In: Serratrice G et al. (eds) Neuromuscular disease, Raven, New York, p 551
- 10.Dubousset Prog Pat Vert. 1996;XIX:177. [Google Scholar]
- 11.Dubousset Rev Chir Orthop. 1983;69:207. [PubMed] [Google Scholar]
- 12.Dubowitz V (1978) Muscle disorders in childhood, Saunders, Philadelphia
- 13.Dweyr Clin Orthop. 1969;62:192. [PubMed] [Google Scholar]
- 14.Forst Z Orthop Ihre Grenzgeb. 1997;135:95. doi: 10.1055/s-2008-1039563. [DOI] [PubMed] [Google Scholar]
- 15.Galasko Isr J Med Sci. 1977;13:165. [PubMed] [Google Scholar]
- 16.Galasko CSB (1987) The orthopaedic management of the dystrophies, myopathies, atrophies, neuropathies and ataxias. In: Galasko CSB (ed) Neuromuscular problems in orthopaedics, Blackwell, Oxford, pp 83–105
- 17.Galasko J Bone Joint Surg Br. 1992;74:210. doi: 10.1302/0301-620X.74B2.1544954. [DOI] [PubMed] [Google Scholar]
- 18.Galasko Eur Spine J. 1995;4:263. doi: 10.1007/BF00301031. [DOI] [PubMed] [Google Scholar]
- 19.Gardner-Medwin Br Med Bull. 1980;36:109. doi: 10.1093/oxfordjournals.bmb.a071623. [DOI] [PubMed] [Google Scholar]
- 20.Gayet Chirurgie. 1999;124:423. doi: 10.1016/s0001-4001(00)80016-1. [DOI] [PubMed] [Google Scholar]
- 21.Gibson Orthop Clin North Am. 1978;9:437. [PubMed] [Google Scholar]
- 22.GibsonClin Orthop 1975108411139835 [Google Scholar]
- 23.Granata Neuromuscul Disord. 1996;6:61. doi: 10.1016/0960-8966(95)00019-4. [DOI] [PubMed] [Google Scholar]
- 24.Harrington J Bone Joint Surg Am. 1962;44:591. [PubMed] [Google Scholar]
- 25.Heller Prosthet Orthot Int. 1997;21:202. doi: 10.3109/03093649709164558. [DOI] [PubMed] [Google Scholar]
- 26.Hopf Z Orthop Ihre Grenzgeb. 1994;132:377. doi: 10.1055/s-2008-1039840. [DOI] [PubMed] [Google Scholar]
- 27.Hsu Spine. 1983;8:771. doi: 10.1097/00007632-198310000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy Thorax. 1995;50:1173. doi: 10.1136/thx.50.11.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurz J Pediatr Orthop. 1983;3:347. doi: 10.1097/01241398-198307000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Ledoux Kinesiter Scient. 1980;177:51. [Google Scholar]
- 31.Luque Spine. 1982;7:256. doi: 10.1097/00007632-198205000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Marchesi J Pediatr Orthop. 1997;17:743. doi: 10.1097/00004694-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Matsumura Rinsho Shinkeigaku. 1997;37:87. [PubMed] [Google Scholar]
- 34.McCarthy Orthop Clin North Am. 1999;30:435. doi: 10.1016/s0030-5898(05)70096-1. [DOI] [PubMed] [Google Scholar]
- 35.Miller Dev Med Child Neurol. 1992;34:775. doi: 10.1111/j.1469-8749.1992.tb11516.x. [DOI] [PubMed] [Google Scholar]
- 36.Miller J Pediatr Orthop. 1988;8:133. [PubMed] [Google Scholar]
- 37.Miller Clin Pediatr. 1985;24:94. doi: 10.1177/000992288502400207. [DOI] [PubMed] [Google Scholar]
- 38.MillerNeurology 199141381985293 [Google Scholar]
- 39.Mubarak J Pediatr Orthop. 1993;13:752. doi: 10.1097/01241398-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 40.NobleArch Dis Child 1986611683485405 [Google Scholar]
- 41.Pruijs J Pediatr Orthop. 2000;B9:217. [Google Scholar]
- 42.Rennie Nature. 1982;296:165. doi: 10.1038/296165a0. [DOI] [PubMed] [Google Scholar]
- 43.Rice Ir J Med Sci. 1998;167:242. doi: 10.1007/BF02937422. [DOI] [PubMed] [Google Scholar]
- 44.Rideau Muscle Nerve. 1984;7:281. doi: 10.1002/mus.880070405. [DOI] [PubMed] [Google Scholar]
- 45.SakaiClin Orthop 19776256340097 [Google Scholar]
- 46.Savini Rivista Italiana di Ortopedia e Traumatologia Pediatrica. 1991;7:249. [Google Scholar]
- 47.Shapiro Muscle Nerve. 1992;15:604. doi: 10.1002/mus.880150512. [DOI] [PubMed] [Google Scholar]
- 48.Siegel Muscle Nerve. 1978;1:453. doi: 10.1002/mus.880010603. [DOI] [PubMed] [Google Scholar]
- 49.Smith N Engl J Med. 1987;316:1197. doi: 10.1056/NEJM198705073161906. [DOI] [PubMed] [Google Scholar]
- 50.StrickerEur Spine J 199651018724189 [Google Scholar]
- 51.Sussman J Pediatr Orthop. 1984;4:532. [PubMed] [Google Scholar]
- 52.Swank Spine. 1982;7:484. doi: 10.1097/00007632-198209000-00013. [DOI] [PubMed] [Google Scholar]
- 53.Tunner Arch Dis Child. 1976;51:170. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weimann Spine. 1983;8:776. doi: 10.1097/00007632-198310000-00015. [DOI] [PubMed] [Google Scholar]
- 55.Yazici J Bone Joint Surg Am. 2000;82:524. doi: 10.2106/00004623-200004000-00008. [DOI] [PubMed] [Google Scholar]