Abstract
Our aim was to validate a culturally adapted, Tunisian-language version of the Roland-Morris Disability Questionnaire (RMDQ), which is a reliable evaluation instrument for low-back-pain disability. A total of 62 patients with low back pain were assessed by the questionnaire. Reliability for the 1-week test/re-test was assessed by a construction of a Bland Altman plot. Internal construct validity was assessed by Cronbach’s αtest. External construct validity was assessed by association with pain, the Schober test and the General Function Score. Sensitivity to change was determined using a t-test for paired data to compare RMDQ scores at inclusion and at completion of the therapeutic sequence of local corticosteroid injections. We also compared the questionnaire score with the General Function Score, both taken after completion of the therapeutic sequence. The constructed Bland Altman plot showed good reliability. Internal consistency of the RMDQ was found to be very good and the Cronbach’s α test was 0.94, indicating a good internal construct validity. The questionnaire is correlated with the pain visual analogue scale (r=33; p=0.0001), with the Schober test (r=0.27; p=0.0001) and the General Function Score (r=56; p=0.0001) indicating an adequate external construct validity. The RMDQ administered after the therapeutic sequence is sensitive to change (r=0.83; p=0.000). Comparison of the questionnaire score to the General Function Score, after completion of the therapeutic sequence, was satisfactory (r=0.75; p=0.000). We conclude that the Tunisian version of the Roland-Morris questionnaire has good reliability and internal consistency. Furthermore, it has a good internal- and external construct validity and high sensitivity to change. It is an adequate and useful tool for assessing low-back-pain disability.
Keywords: Low back pain, Roland-Morris Disability Questionnaire
Introduction
Low back pain (LBP) is a ubiquitous health problem. It represents the most frequent illness in humans. LBP lifetime prevalence ranges 60–90%, and the annual incidence is 5% [6]. It is reported to be the leading cause of disability in people under 45 years of age and the third cause of disability in those over 45 [21]. High costs associated with LBP and its socio-economic impact have made this so-called self-limited and benign condition a considerable health-care policy challenge, especially in industrial countries [1, 7, 20, 21]. LBP may have an impact on the functional status of the patient, interfering with basic activities like standing, walking, dressing and many work-related activities, leading to pain and disability. Measuring the disability is important. First, as an outcome measure, it is an important indicator of the of the patient’s quality of life. In addition, this outcome can be used for planning and monitoring therapy, clinical and epidemiological research, program evaluation, policy analysis, risk factors and use of health services [10, 12].
A variety of outcome measures are used for LBP. The Roland-Morris Disability Questionnaire (RMDQ) [16] (Appendix) is the most common instrument used, and studies have reported that the test/re-test reliability, validity and responsiveness of RMDQ are adequate [16, 18]. Furthermore, it has been successfully adapted across cultures [11, 12, 15, 22]. The purpose of this study is to validate the culturally adapted, Tunisian-language version of the RMDQ.
Materials and methods
The RMDQ was translated according to a process using the recent guidelines for cross-cultural adaptation [2]. The Tunisian version includes all items of the original questionnaire, in the same order, and is also designed to be self-administered. The method used for calculating the disability score is unchanged from the original questionnaire. The maximum possible score is therefore 24 (1 point for each of the 24 items), and the minimum score is 0.
Sixty-two consecutive patients suffering from chronic LBP for at least 3 months and needing a series of three local, corticosteroid injections, were included in the study. All patients underwent physical and neurological examinations, spine radiography and laboratory tests (complete blood count, erythrocyte sedimentation rate). All patients were assessed by the same observer (I.B.). The assessment included lumbar flexibility measured by Schober test, pain visual analog scale (0–100), and functional disability by RMDQ. The RMDQ was self-completed by literate patients. For illiterate patients, the questionnaire was administered by the observer. We also administered the General Function Score [9]. Patients were asked to attend an additional assessment 1 week later, at admission to the ward for local corticosteroid injections.
We tested the reliability, validity and responsiveness of the RMDQ. The common forms of reliability [17] for a self-completed questionnaire in a yes/no format, such as the present instrument, are KAPPA statistics of agreement, or a construction of a Bland Altman plot [3] for test/re-test agreement, chosen for this study. We also tested the validity in its two forms: internal validity, in which attention is given to the integrity of the defined construct [14] and external validity, which is concerned with expected associations with other key variables [19]. Internal construct validity was assessed by Cronbach’s α test [5]. External construct validity was assessed by association with pain, the Schober test and the General Function Score. Responsiveness, a more recently analysed quality of an instrument, assesses the ability of the instrument to detect any change.
Sensitivity to change was determined using a t-test for paired data to compare RMDQ scores at inclusion, and at completion of the therapeutic sequence (local corticosteroid injections), after a mean duration of 1 month. We also compared the RMDQ score and General Function Score, both taken after completion of the therapeutic sequence. Data were analysed using the statistical package for the social sciences, SPSS 10.0 for Windows. The significance level was fixed at 0.05.
Results
Patients’ characteristics
A total of 62 patients were enrolled in the study. Patients’ characteristics are shown in Table 1. None of the patients had undergone surgery. Neurological examinations and laboratory tests (complete blood count, erythrocyte sedimentation rate) were normal.
Table 1.
Clinical characteristics of 62 patients with low back pain. Values are presented as means and standard deviation. RMDQ The Roland-Morris Disability Questionnaire VAS visual analogue scale
| Age (years) Number of male/female patients Duration of symptoms(years) Schober test (cm)* Pain VAS (mm)* RMDQ score* |
44 (12) 35/27 3.0 (1.1) 13.9 (0.9) 74 (17) 19.6 (3.9) |
| General function score* | 17.1 (2.9) |
*Values at baseline
Reliability, validity and responsiveness
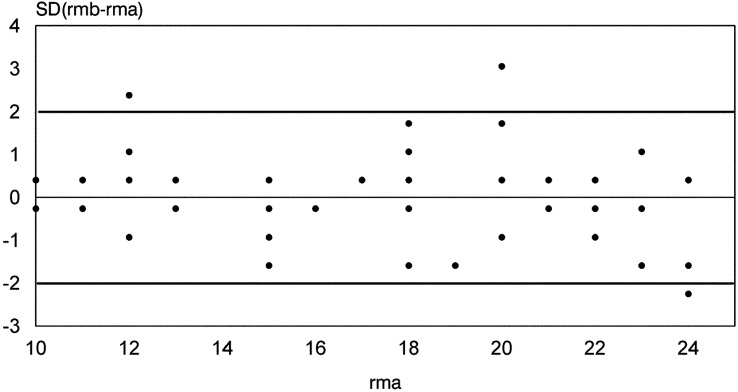
The constructed Bland Altman plot for test/re-test agreement showed a good reliability (Fig. 1). Internal consistency was adequate, with a Cronbach’s alpha test at 0.94. The RMDQ score is correlated with the pain visual analogue scale (r=0.33; p=0.0001), with the Schober test (r=0.27; p=0.0001) and the General Function Score (r=.56; p=0.0001) indicating an adequate external construct validity. The RMDQ administered after the therapeutic sequence was sensitive to change (r=0.83; p=0.0001). One month after discharge, the mean RMDQ score was 15.3 (SD: 4.8). The comparison of the RMDQ score with the General Function Score after completion of the therapeutic sequence was satisfactory (r=0.75; p=0.000).
Fig. 1.
Bland Altman plot for test/re-test reliability of the Roland-Morris Disability Questionnaire. rma initial Roland-Morris Disability Questionnaire score. rmb Roland-Morris Disability Questionnaire score 1 week later. SD Standard deviation
Acceptability
Acceptability of the questionnaire proved satisfactory. No patients declined to complete it and many expressed satisfaction that issues usually not addressed during visits for LBP were receiving attention. Completion of the questionnaire proved simple and rapid (3 min).
Discussion
The sequential process of adaptation of outcome measures for use in different cultures is well documented [2, 8]. After this process, it is necessary to establish the psychometric credentials of the newly adapted instrument. The adaptation of the RMDQ for the Tunisian language has produced an instrument that is reliable and demonstrative of both internal and external validities. Reliability levels were similar to the French [4], German [22], Italian [15], Spanish [11] and Turkish [12] versions. Although statistically significant, the correlation in our study of the RMDQ score with the Schober test and the pain visual analogue scale is weak, compared with the original version [16] and the Italian version [15], for which correlation of the RMDQ score with the pain visual analogue scale was very good (r=0.79; P<0.001). The mean pain visual analogue scale reported in Italian patients was inferior to that of our patients (42 mm vs 74 mm).
Sensitivity to change was satisfactory—the scale was able to detect changes in LBP-related functional disability over a period of 1 month and a therapeutic sequence was known to be used, as no gold standard of LBP treatment exists [13]. Thus, the validation of the Tunisian version of the RMDQ was successful, but we were not protected from a possible ceiling effect.
Tunisian spoken Arabic is very easy to understand by people of the Maghreb (Algeria and Morocco). It is also easy to understand for speakers of the Arabic spoken in the Middle East and Gulf countries. The Tunisian version of the RMDQ has good reliability and internal consistency. It has a good internal and external construct validity and high sensitivity to change. It is an adequate and useful instrument for assessing low-back-pain disability. It can be used in the Maghreb and the Middle East. Furthermore, it can be applied to Maghreb immigrants to Western Europe, as the French version is used in Belgium and Switzerland.
Acknowledgement
We are grateful to Adel Rdissi, an English teacher at the faculty of medicine, for reviewing the English of this manuscript
Appendix: Roland-Morris low back pain questionnaire [16]
Please read:
When your back hurts, you may find it difficult to do some of the things you normally do. Mark only the sentences that describe you today.
1. I stay at home most of the time because of my back.
2. I change position frequently to try to get my back comfortable.
3. I walk more slowly than usual because of my back.
4. Because of my back, I am not doing any jobs that I usually do around the house.
5. Because of my back, I use a handrail to get upstairs.
6. Because of my back, I lie down to rest more often.
7. Because of my back, I have to hold on to something to get out of an easy chair.
8. Because of my back, I try to get other people to do things for me.
9. I get dressed more slowly than usual because of my back.
10. I stand up only for short periods of time because of my back.
11. Because of my back, I try not to bend or kneel down.
12. I find it difficult to get out of a chair because of my back.
13. My back is painful almost all of the time.
14. I find it difficult to turn over in bed because of my back.
15. My appetite is not very good because of my back.
16. I have trouble putting on my socks (or stockings) because of pain in my back.
17. I walk only short distances because of my back pain.
18. I sleep less well because of my back.
19. Because of back pain, I get dressed with help from someone else.
20. I sit down for most of the day because of my back.
21. I avoid heavy jobs around the house because of my back.
22. Because of back pain, I am more irritable and bad tempered with people than usual.
23. Because of my back, I go up stairs more slowly than usual.
24. I stay in bed most of the time because of my back
References
- 1.Andersson GBJ (1997) The epidemiology of spinal disorders. In: Frymoyer JW (ed) The adult spine: principles and practice. Lippincott, Philadelphia, pp 93–141
- 2.BeatonSpine 200025318611124735 [Google Scholar]
- 3.BlandLancet 198613072868172 [Google Scholar]
- 4.Coste J, Le Parc JM, Berge E, Delecoeuillerie G, Paolaggi JB (1993) [French validation of a disability rating scale for the evaluation of low back pain (EIFEL questionnaire)] Rev Rhum Ed Fr 60(5):335–341 [PubMed]
- 5.Cronbach Psychometrika. 1951;16:297. doi: 10.1007/BF02289113. [DOI] [PubMed] [Google Scholar]
- 6.Frymoyer N Engl J Med. 1988;318:291. doi: 10.1056/NEJM198802043180506. [DOI] [PubMed] [Google Scholar]
- 7.Garg Occup Med. 1992;7:593. [PubMed] [Google Scholar]
- 8.Guillemin J Clin Epidemiol. 1993;46:1417. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 9.Hagg Eur Spine J. 2001;10:203. doi: 10.1007/s005860000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keith Arch Phys Med Rehabil. 1994;75:478. doi: 10.1016/0003-9993(94)90175-9. [DOI] [PubMed] [Google Scholar]
- 11.Kovacs Spine. 2002;27:538. doi: 10.1097/00007632-200203010-00016. [DOI] [PubMed] [Google Scholar]
- 12.Kucukdeveci Spine. 2001;26:2738. doi: 10.1097/00007632-200112150-00024. [DOI] [PubMed] [Google Scholar]
- 13.Marty Rev Rhum Engl Ed. 1998;65:126. [PubMed] [Google Scholar]
- 14.Nunally JC Jr (1978) Psychometric theory, 2nd edn. McGraw-Hill, New York
- 15.Padua Eur Spine J. 2002;11:126. doi: 10.1007/s005860100262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roland Spine. 1983;8:141. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Shrout J Clin Epidemiol. 1989;42:69. doi: 10.1016/0895-4356(89)90027-9. [DOI] [PubMed] [Google Scholar]
- 18.Stratford Phys Ther. 1998;78:1186. doi: 10.1093/ptj/78.11.1186. [DOI] [PubMed] [Google Scholar]
- 19.Streiner DL, Norman GR (1995) Health measurement scales. Oxford University, Oxford
- 20.Waddell G (1998) The Back pain revolution. Churchill Livingstone, Edinburgh
- 21.Weinstein SM, Herring SA (1993) Rehabilitation of the patient with low back pain. In: DeLisa JA, Gans BM (eds) Rehabilitation Medicine: Principles and practice: Lippincott, Philadelphia pp 996–1017
- 22.Wiesinger Spine. 1999;24:1099. doi: 10.1097/00007632-199906010-00009. [DOI] [PubMed] [Google Scholar]