Abstract
Objectives: (1) The aim of this study is to assess the efficacy of The Bethesda System for Reporting Thyroid Cytology (TBSRTC) in accurate prediction of thyroid lesions on fine needle aspiration (FNA). (2) To appraise the surgeon with guidelines for adequacy of samples, and interpretation of FNA reports with TBSRTC and hence aiding them in surgical decision making. Five hundred and sixty four FNAs were done on patients with thyroid swellings in the department of Pathology and reported using TBSRTC guidelines. In cases where surgery was done, histopathological report was correlated. Using TBSRTC the commonest cytological diagnosis was benign-Hashimotos thyroiditis followed by benign follicular nodule. TBSTRC reduces inter-observer variability in reporting thyroid FNAs and provides good communication between the surgeon and pathologist. It also implicates guidelines for cancer risk and clinical management to the surgeons, thus avoiding unnecessary surgery.
Keywords: Thyroid, Cytology, Fine-needle aspiration, Terminology
Introduction
Fine needle aspiration (FNA) cytology is a widely utilized tool for the diagnosis of thyroid lesions with a high degree of sensitivity, specificity and diagnostic accuracy [1, 2].
To address the terminology and other issues related to thyroid FNA, the National Cancer Institute (NCI) hosted the “the NCI Thyroid Fine Needle Aspiration State of the Science conference” in 2007 at Bethesda, Maryland. The conclusions of the meeting led to the Bethesda Thyroid Atlas Project and formed the framework for The Bethesda System for Reporting Thyroid Cytology (TBSRTC). The adoption of the system will facilitate communication among the cytopathologist, surgeon, endocrinologist and radiologist and also allow easy and reliable sharing of data from different laboratories for national and international collaborative studies.
TBSRTC recommended certain categories and the rationale of this categorization is to implicate cancer risk associated with each category along with guidelines for clinical management.
Materials and Methods
A prospective study of 564 cases of thyroid FNAs done in the Department of pathology over a period of 17 months (August 2009 to December 2010) was undertaken. Complete clinical history, thyroid hormonal profile and imaging studies were done.
FNAs were performed using 22G needle, with or without an airtight syringe, using imaging guidance wherever necessary. Smears were fixed in 95% methanol, while still wet and stained using the standard Haematoxylin and Eosin, Giemsa and Papanicolaou stains. FNAs were reported using TBSRTC and cancer risk with guidelines for further management were communicated to the surgeon.
The recommended diagnostic categories by TBSRTC are demonstrated in Table 1. The implied risk of malignancy and recommended clinical management are seen in Table 2.
Table 1.
TBSRTC: recommended diagnostic categories [4]
| Number | Name of the category |
|---|---|
| I | Nondiagnostic or unsatisfactory |
| Cystic fluid only | |
| Virtually acellular specimen | |
| Other (obscuring blood, collecting artifacts, etc.) | |
| II | Benign |
| Consistent with a benign follicular nodule (includes adenomatoid nodule, colloid nodule etc.) | |
| Consistent with lymphocytic (Hashimoto) thyroiditis in the proper clinical context | |
| Consistent with granulomatous (subacute) thyroiditis | |
| Other | |
| III | Atypia of undetermined significance or follicular lesion of undetermined significance |
| IV | Follicular neoplasm or suspicious for a follicular neoplasm |
| Specify if Hurthle cell (oncocytic type) | |
| V | Suspicious for malignancy |
| Suspicious for papillary carcinoma | |
| Suspicious for medullary carcinoma | |
| Suspicious for metastatic carcinoma | |
| Suspicious for lymphoma | |
| Other | |
| VI | Malignant |
| Papillary thyroid carcinoma | |
| Poorly differentiated carcinoma | |
| Medullary thyroid carcinoma | |
| Undifferentiated (anaplastic) carcinoma | |
| Squamous cell carcinoma | |
| Carcinoma with mixed features (specify) | |
| Metastatic carcinoma | |
| Non-Hodgkin’s lymphoma | |
| Other |
Table 2.
TBSRTC: implied risk of malignancy and recommended clinical management [4]
| Diagnostic category | Risk of malignancy (%) | Usual management |
|---|---|---|
| Nondiagnostic or unsatisfactory | 1–4 | Repeat FNA with ultrasound guidance |
| Benign | 0–3 | Clinical follow-up |
| Atypia of undetermined significance or follicular lesion of undetermined significance | 5–15 | Repeat FNA |
| Follicular neoplasm or suspicious for follicular neoplasm | 15–30 | Surgical lobectomy |
| Suspicious for malignancy | 60–75 | Near-total thyroidectomy or surgical lobectomy |
| Malignant | 97–99 | Near-total thyroidectomy |
Results
A total of 564 cases were aspirated in the department of Pathology. Male to female ratio being 1:9 and age at presentation varied from 10 to 82 years with mean age being 34 years. Most of the patients presented with a swelling in the thyroid region. The commonest cytological diagnostic category was benign-Hashimotos thyroiditis followed by benign follicular nodule. Table 3 shows the number of cases in each TBSRTC category.
Table 3.
Showing number of cases in each TBSRTC category
| S. no. | Category | Number of cases | Percentage (%) | F:M | Common age group (years) |
|---|---|---|---|---|---|
| 1 | Non-diagnostic/unsatisfactory | 96 | 17 | 13:1 | 20–30 |
| 2 | Benign | 398 | 70.56 | 16:1 | 20–30 |
| 3 | AUS/FLUS | 11 | 1.95 | 10:1 | 30–40 |
| 4 | FN/SFN | 24 | 4.2 | 5:1 | 50–70 |
| 5 | Suspicious of malignancy | 15 | 2.6 | 6.5:1 | 20–30 |
| 6 | Malignant | 20 | 3.5 | 1:1 | 60–70 |
Table 4 shows details of Benign (TBSRTC primary category II) lesions.
Table 4.
Details of benign (TBSRTC primary category II)
| S. no. | Sub category | Number of cases | Percentage (%) | F:M | Common age group (years) |
|---|---|---|---|---|---|
| 1 | Benign follicular nodule | 193 | 48.49 | 11:1 | 30–50 |
| 2 | Hashimoto’s thyroiditis | 184 | 46.23 | 37:1 | 20–30 |
| 3 | Acute thyroiditis | 4 | 1 | 3:1 | 30–40 |
| 4 | Colloid nodule | 12 | 3 | 2:1 | 10–20 |
| 5 | Subacute/granulomatous thyroiditis | 5 | 1.26 | 4:1 | 20–30 |
Table 5 shows details of lesions categorized as suspicious of malignancy (TBSRTC primary category V).The cases of suspicious papillary thyroid carcinomas (PTCs) formed the majority (14 cases).
Table 5.
Details of lesions categorized as suspicious of malignancy (TBSRTC primary category V)
| S. no. | Sub category | Number of cases | Percentage (%) | (F:M) | Common age group (years) |
|---|---|---|---|---|---|
| 1 | Suspicious of PTC | 13 | 87 | 12:1 | 60–70 |
| 2 | Suspicious of medullary thyroid carcinoma | 1 | 6.5 | F | 26 |
| 3 | Suspicious of lymphoma | 1 | 6.5 | F | 28 |
Table 6 shows details of lesions categorized as malignant (TBSRTC primary category VI). Majority of cases were again papillary carcinoma (16 cases).
Table 6.
Details of lesions categorized as malignant (TBSRTC primary category VI)
| S. no. | Sub category | Number of cases | Percentage (%) | F:M | Common age group (years) |
|---|---|---|---|---|---|
| 1 | Papillary Ca | 15 | 75 | 2:1 | 40–50 |
| 2 | Medullary Ca | 1 | 5 | F | 25 |
| 3 | Anaplastic Ca | 2 | 10 | M | 50–60 |
| 4 | NHL | 1 | 5 | F | 62 |
| 5 | Metastatic | 1 | 5 | F | 70 |
Discussion
An FNA sample of a thyroid nodule should be representative of the underlying lesion, in order to provide useful diagnostic information. FNA reduces the rate of unnecessary thyroid surgery in patients with benign nodules and detects those with thyroid cancers who have to be surgically treated.
Before the routine use of thyroid FNA, the percentage of surgically thyroid nodules that were malignant was 14%. With current thyroid FNA practice, the percentage of resected nodules that are malignant surpasses 50% [3]. It is essential that the cytopathologist communicates thyroid FNA interpretations to referring surgeons in terms that are succinct, unambiguous and helpful in clinical management. Historically, terminology for thyroid FNA has varied from one laboratory to another, creating confusion and hindering the sharing of data among multiple institutions.
For clarity of communication and uniformity of terminology NCI hosted “The NCI Thyroid FNA State Science Conference”. The conclusions regarding terminology and morphologic criteria from this meeting led to The Bethesda Thyroid Atlas Project and formed the framework for TBSRTC.
TBSRTC recommends five general diagnostic categories and suggests that each report should begin with a general diagnostic category. The diagnostic categories are given in Table 1. Some degree of subcategorization is also done. Each of the categories has an implied cancer risk (ranging from 0 to 3% for the benign category to nearly 100% for the malignant category) with rational clinical management guidelines (Table 2).
Category I—nondiagnostic or unsatisfactory (ND/UNS)
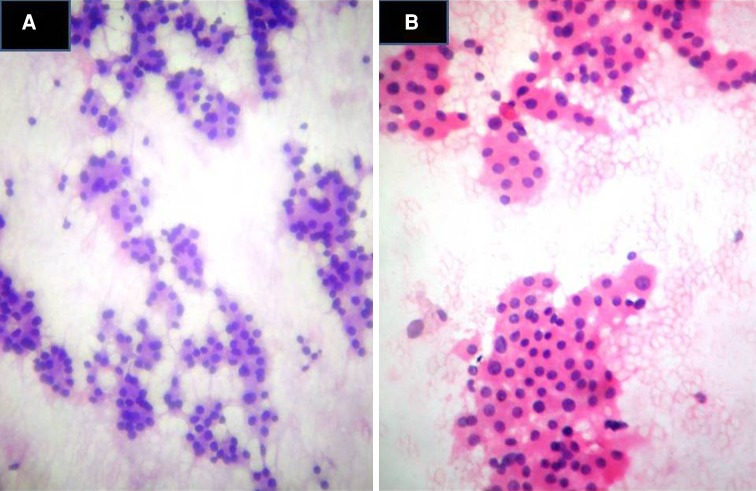
An UNS specimen is always ND but some technically satisfactory specimens may also be considered “nondiagnostic” that is, showing nonspecific features not conclusively diagnostic of a particular entity. TBSRTC recommends certain criteria for adequacy, as a minimum of six groups of well visualized thyroid follicular cells with at least 10 cells per group, preferably on a single slide. Most of our cases showed only cyst fluid with plenty of foamy macrophages (Fig. 1). Exceptions to this category are solid nodules with cytologic atypia, solid nodules with inflammation and colloid nodules. ND/UNS results occur in 2–20% of cases but ideally should be limited to no more than 10% of thyroid FNAs [5, 7]. According to these criteria, in our present study ND/UNS cases were 96 (17%). In these cases we advised repeat aspiration with ultrasound guidance as recommended by TBSRTC (Table 2).
Fig. 1.
TBSRTC category I (ND/UNS) cyst fluid with macrophages (H&E ×400)
Category II—benign
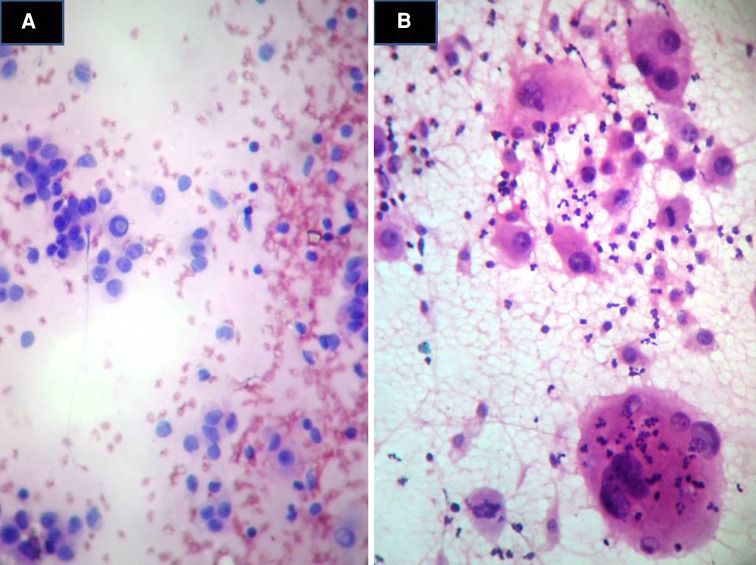
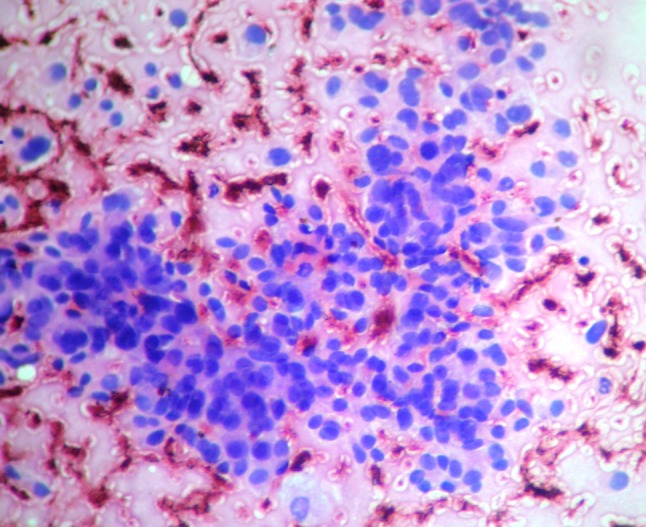
This category includes benign follicular nodule (adenomatoid nodule, colloid nodule), lymphocytic (Hashimotos) thyroiditis and granulomatous (subacute) thyroiditis. The benefit of thyroid FNA in these cases is when a reliably benign interpretation is done it avoids unnecessary surgery. The term benign follicular nodule is applied to the most common benign pattern; where an adequate specimen is composed of varying proportion of colloid and benign follicular cells arranged as macro follicles and micro follicle fragments. On histopathology these nodules turned out to be nodules of multinodular goiter (MNG) or follicular adenomas (FAs). In our study the false negative rate was low (2%). Other benign subcategories include “consistent with lymphocytic (Hashimotos) thyroiditis” in the proper clinical context and “consistent with granulomatous (subacute) thyroiditis”. The criteria for Hashimotos thyroiditis is a polymorphic lymphoid population and occasional plasma cells and hurthle calls arranged in sheets or as isolated cells (Fig. 2).
Fig. 2.
TBSRTC category II Benign—Hashimotos thyroiditis—Hurthle cells with abundant pink cytoplasm and lymphocytes (H&E ×400)
Most of our cases were from this category with a total of 398 cases (70.56%).
The recommended management of this category is clinical follow up.
Category III—atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS)
Thyroid FNAs that do not fit into benign, suspicious or malignant categories are included here. AUS/FLUS is reserved for specimens that contain cells (follicular, lymphoid) with architectural atypia that isn’t sufficient to be classified as suspicious for a follicular neoplasm (FN) or malignancy and on the other hand atypia is more marked than benign change (Fig. 3).
Fig. 3.
TBSRTC category III (AUS/FLUS) thyroid follicular cells with architectural and cytological atypia (H&E ×400)
According to TBSRTC AUS/FLUS is a category of resort and should not be used indiscriminately. In our study 11 cases (1.95%) were of this category out of which 7 cases were papillary carcinoma and 4 were FA. The cancer risk for this category according to TBSRTC is 5–15% and recommended management protocol is repeat FNA after sufficient time gap. We advised the same in all our 11 cases.
Category IV—FN or suspicious for a FN (FN/SFN)
The aim of this category is to identify a nodule that might be a follicular carcinoma. Follicular carcinomas have cytomorphologic features that distinguish them from benign follicular nodules but do not permit distinction from a FA. They are reportable as FN or SFN. About 15–30% of these cases called FN/SFN prove to be malignant [3–5] the rest being FAs or adenomatoid nodules of MNG [3, 6]. The criteria for reporting under TBSRTC category IV are significant alteration in the follicular cell architecture, characterized by cell crowding, micro follicles, dispersed isolated cells and scant or absent colloid (Fig. 4). The criteria for FN Hurthle cell type/suspicious for a FN Hurthle cell type FNHCT/SFNHC (subcategory of TBSRTC IV) are a sample consisting exclusively of hurthle cells, usually little or no colloid or virtually no lymphocytes or plasma cells (Fig. 4).
Fig. 4.
a TBSRTC category IV (FN/SFN) follicular cells in micro follicles with abundant colloid (H&E ×400). b Hurthle cell neoplasm showing only Hurthle cells (H&E ×400)
In the present study 24 cases (4.2%) were from this category. Hurthle cell subcategory were 2 cases only, the remaining being of follicular nature.
TBSRTC recommends lobectomy for this category.
Category V—suspicious for malignancy
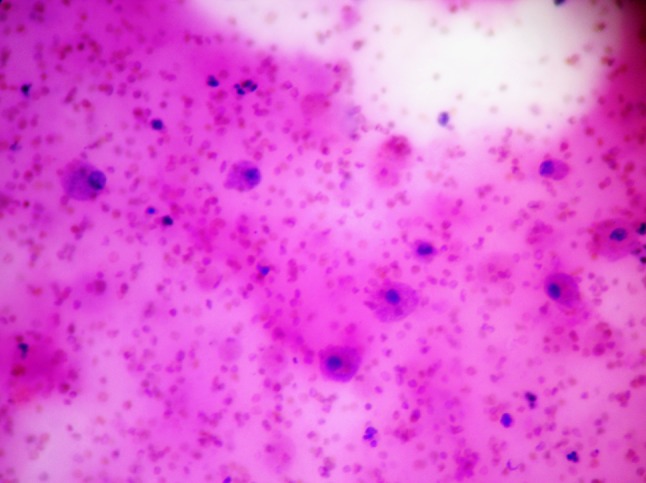
Many thyroid cancers, especially PTC can be diagnosed with certainty by FNA. But the nuclear and architectural changes of some PTCs are subtle and focal. This is particularly true of the follicular variant of PTC, which can be difficult to distinguish from a benign follicular nodule. If only one or two characteristic features of PTC are present, if they are only focal, or if the sample is sparsely cellular a malignant diagnosis cannot be made with certainty (Fig. 5). Such cases are best classified as suspicious for malignancy. Most (60–75%) of these cases prove to be papillary carcinomas and the rest are usually FAs [3, 5, 8]. The same general principle applies to other thyroid malignancies like medullary carcinoma and lymphoma, where ancillary tests help.
Fig. 5.
TBSRTC category V suspicious for papillary carcinoma-focal nuclear grooving (H&E ×400)
We reported only 16 cases in this category (2.6%). Histologically ten of these proved to be malignant the others being nodular goiter.
TBSRTC recommends near-total thyroidectomy or surgical lobectomy for cases in this category.
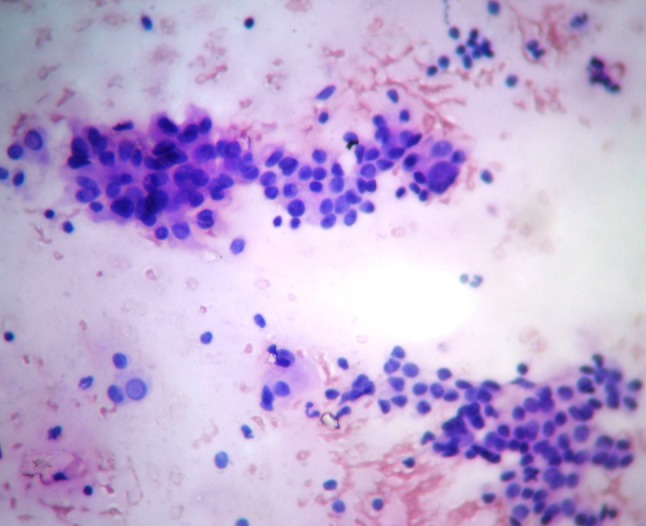
Category VI—malignant
The general category malignant is used whenever the cytomorphologic features are conclusive for malignancy.
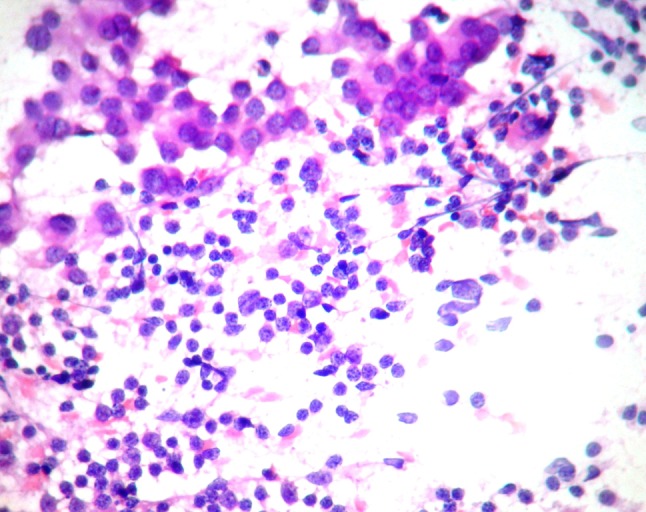
The criteria for reporting PTC are follicular cells arranged in papillae/syncytial like monolayers, altered follicular cells exhibiting characteristic nuclear features like enlarged oval or irregular molded nuclei, longitudinal nuclear grooves, intranuclear cytoplasmic pseudo inclusions, pale nuclei with powdery chromatin and psammoma bodies (Fig. 6). In the present study we reported 16 cases (80%) of papillary carcinomas all of which correlated with histology.
Fig. 6.
a TBSRTC category VI Papillary carcinoma-follicular cells in papillae with nuclear grooving and intranuclear inclusions (H&E ×400). b Anaplastic carcinoma with multinucleated tumor giant cells, neutrophilic infiltration of cytoplasm and mitotic activity (H&E ×400)
The criteria for reporting medullary carcinoma are moderate to markedly cellular smears, with plasmacytoid, polygonal, round or spindle shaped cells. Amyloid is often present and appears as dense amorphous material. In this study we diagnosed 1 case (5%) which correlated with histopathology.
The criteria for reporting anaplastic thyroid carcinoma are neoplastic cells arranged in groups or discretely. Individual cells being epitheloid, spindled, plasmacytoid or rhabdoid in shape. Nuclear pleomorphism, multinucleation and neutrophilic infiltration of tumor cell cytoplasm are other features. Mitotic activity will be numerous and abnormal (Fig. 6). In our study we reported 2 cases (10%) and they were confirmed with histopathology.
The criteria for reporting a lymphoma are markedly cellular smears composed of noncohesive round to slightly oval cells with vesicular chromatin and prominent nucleoli.
We reported 1 case (5%) of nonHodgkins lymphoma and 1 case of metastases from a squamous cell carcinoma in our study.
TBSRTC recommends near-total thyroidectomy for these cases of malignancy.
Cytohistological Correlation
In our study of 564 cases the cases reported in the TBSRTC category II were not subjected to surgery. Only 85 cases belonging to the other categories were surgically treated, of which 77 cases correlated with the cytological diagnosis. False positives were 3 cases and false negatives were 5 cases.
Conclusion
TBSRTC reduces interobserver variability in reporting thyroid FNAs. It improves communication between the pathologist and surgeon by way of indicating cancer risk in each category and providing guidelines in surgical management and allows easy and reliable sharing of data between different laboratories.
References
- 1.Leonard N, Melcher DH. To operate or not to operate? The value of fine needle aspiration cytology in the assessment of thyroid swellings. J Clin Pathol. 1997;50:941–943. doi: 10.1136/jcp.50.11.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakhos R, Selvaggi SM, DeJong S, Gordon DL, Pitale SU, Herrmann M, Wojcik EM. Fine-needle aspiration of the thyroid: rate and causes of cytohistopathologic discordance. Diagn Cytopathol. 2000;23:233–237. doi: 10.1002/1097-0339(200010)23:4<233::AID-DC3>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 3.Yassa L, Cibas ES, Benson CB, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer. 2007;111:508–516. doi: 10.1002/cncr.23116. [DOI] [PubMed] [Google Scholar]
- 4.Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658–665. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 5.Yang J, Schnadig V, Logrono R, et al. Fine needle aspiration of thyroid nodules: a study of 4703 patients with histological and clinical correlations. Cancer. 2007;111:306–315. doi: 10.1002/cncr.22955. [DOI] [PubMed] [Google Scholar]
- 6.Baloch ZW, Fleisher S, LiVolsi VA, et al. Diagnosis of “follicular neoplasms”: a gray zone in thyroid-fine needle aspiration cytology. Diagn Cytopathol. 2002;26:41–44. doi: 10.1002/dc.10043. [DOI] [PubMed] [Google Scholar]
- 7.Ravetto C, Colombo L, Dottorini ME. Usefulness of fine needle aspiration in the diagnosis of thyroid carcinoma: a retrospective study in 37,895 patients. Cancer. 2000;90:357–363. doi: 10.1002/1097-0142(20001225)90:6<357::AID-CNCR6>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Logani S, Gupta PK, LiVolsi VA, et al. Thyroid nodule with FNA cytology suspicious for follicular variant of papillary thyroid carcinoma: follow-up and management. Diagn Cytopathol. 2000;23:380–385. doi: 10.1002/1097-0339(200012)23:6<380::AID-DC3>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]