Abstract
Video-assisted thoracic surgery is useful during a typical lobectomy procedure, though challenging in complicated cases. We report successful video-assisted thoracic surgery lobectomy procedures performed after coronary artery bypass grafting in two lung cancer patients, with severe adhesion of lung parenchyma to grafts of the internal thoracic artery. We avoided dissection of the lung from the grafts and divided the lung parenchyma. No intrathoracic infection or local recurrence was found 5 years after surgery in either patient. The present ‘non-dissection technique’ is a feasible and safe optional procedure during a lobectomy after coronary artery bypass grafting using internal thoracic artery grafts.
Keywords: Lung cancer, Video-assisted thoracoscopic surgery, Coronary artery bypass grafting
INTRODUCTION
Video-assisted thoracic surgery (VATS) was introduced in the 1990s and is now a commonly utilized approach for early stage lung cancer [1, 2]. In addition to use in a typical lobectomy, this approach has been reported to be adapted for complicated cases, such as segmentectomy and bronchoplasty procedures [3, 4]. A reoperation following thoracic surgery, such as coronary artery bypass stent grafting (CABG), is also considered to be difficult [5]. In CABG, the intrathoracic artery (ITA) is most often used as the key graft, though severe adhesion between the graft and surrounding tissues is expected. When an upper lobectomy for lung cancer on the same side of the bypass graft is intended, there is a risk of injury to the bypass graft by intraoperative dissection. However, there is no report showing the method of lobectomy with the preservation of the internal thoracic artery graft via the VATS approach and its feasibility based on long-term outcomes. Herein, we report the results of VATS upper lobectomy procedures after CABG, without dissection of lung parenchyma adhering to the ITA in two cases with lung cancer.
CASES
Case 1
The patient was a 60-year old male, who was admitted with an abnormal lung nodule in the left upper lobe. He underwent CABG 5 years previously, during which the left internal thoracic artery (LITA) was used as a graft to the left anterior descending (LAD) coronary artery. Chest computed tomography (CT) findings revealed the possibility of adhesion between the LITA graft and surrounding tissues and lung parenchyma (Fig. 1b). The left upper lobectomy was performed in c-stage IB adenocarcinoma via VATS. During the operation, a camera port was made on the axial line of the sixth intercostal space, and working ports at the fourth and fifth intercostal space of the anterior chest. The VATS approach provided a clear surgical view of the severe adhesion between the graft pedicle and upper lobe. The adhesion area was localized and apart from the primary tumour, and there was also free space around the hilum (Fig. 2a). Therefore, we divided the lung parenchyma with an adequate margin from the tumour and the graft, using an endo-stapler (Fig. 2b). We then divided the hilar vessels and upper bronchus, and the left upper lobectomy was completed.
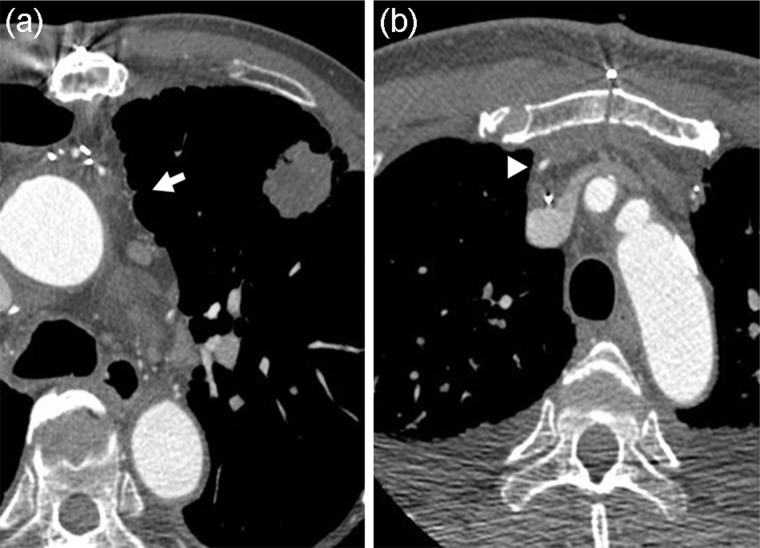
Figure 1:
Preoperative chest CT findings. (a) Case 1: white arrow indicates possible adhesion to ITA graft pedicle and left upper lobe. (b) Case 2: white arrow head indicates the ITA graft.
Figure 2:

Operative views with VATS of Case 1. (a) White arrows indicate severe adhesion between graft pedicle and left upper lobe. The dot line circle shows no adhesion area. (b) Dissection of lung parenchyma using endo-stapler after taping. LUL: left upper lobe.
Case 2
The patient was a 65-year old male patient with c-stage IA adenocarcinoma in the right upper lobe. CABG had been performed 10 years previously for coronary artery stenosis, using the right internal thoracic artery (RITA) to connect to the LAD. Chest CT findings revealed the possibility of adhesion between the graft and neighbouring right upper lobe (Fig. 1a). We performed a VATS right upper lobectomy, using the same approach as in Case 1. Severe adhesion was found between the right upper lobe and RITA graft, and dissection of the graft from the lung was abandoned. To preserve the graft pedicle, we taped around the lung parenchyma adhering to the graft. First, the lung parenchyma was divided using an endo-stapler with an adequate margin more than 3 cm from the tumour, and then the right upper lobectomy was successfully completed.
The postoperative courses of both cases were uneventful. Perioperative antibiotic therapy was administered at normal dosages, with no occurrence of empyema or abscess in the remaining lung. Follow-up results obtained with enhanced CT and coronary angiography examinations revealed atrophic change of the remnant lung and good patency of the grafts. In the 5-year follow-up examinations, no local or distant recurrence was detected in either patient.
COMMENT
Using VATS, we surgically treated two cases of primary lung cancer after CABG with ITA grafts. Post-CABG adhesion between the graft and lung parenchyma is a critical problem in the management of radical resection for lung cancer, and great attention must be given to prevent injury to the bypass grafts. We successfully completed the lobectomy, using a VATS approach in the present cases. We believe that such a thoracoscopic approach presents advantages in regard to the surgical view compared with a conventional open thoracotomy.
This is the first report regarding the feasibility of this ‘non-dissection technique’ with VATS, including long-term follow-up results. We found that even in such complicated cases, a lobectomy could be completed with VATS, as it provided a good surgical view. The follow-up CT scan findings revealed good patency of the grafts, while ultrasound cardiography showed good cardiac function. A good outcome without recurrence was obtained in both cases.
There are some important points and limitations to the present approach. First, additional experience and training are necessary for surgical manipulation with this VATS approach compared with an open thoracotomy. Second, when the tumour is located near the grafts, it is difficult to obtain a safe surgical margin. In such cases, conversion to an open thoracotomy with direct hand assistance should be considered. Third, it is necessary to monitor carefully the waveform of the ECG electrocardiogram to prevent the graft from being damaged, before lung parenchyma is divided using an endo-stapler. Fourth, to prevent the infection of residual lung parenchyma, antibiotics were given postoperatively for longer periods than usual.
In conclusion, VATS lobectomy without dissection of an ITA graft from the lung may be a good option for patients undergoing a CABG procedure that utilizes the ITA as a graft.
Conflict of interest: none declared.
REFERENCES
- 1.Lewis RJ, Caccavale RJ, Sisler GE, Mackenzie JW. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg. 1992;104:1679–85. [PubMed] [Google Scholar]
- 2.Shaw JP, Dembitzer FR, Wisnivesky JP, Litle VR, Weiser TS, Yun J, et al. Video-assisted thoracoscopic lobectomy: state of the art and future directions. Ann Thorac Surg. 2008;85:S705–9. doi: 10.1016/j.athoracsur.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 3.Schuchert MJ, Pettiford BL, Keeley S, D'Amato TA, Kilic A, Close J, et al. Anatomic segmentectomy in the treatment of stage 1 non-small cell lung cancer. Ann Thorac Surg. 2007;84:926–32. doi: 10.1016/j.athoracsur.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Kamiyoshihara M, Ibe T, Takeyoshi I, Atsumi J, Ibe T, Kakegawa S, et al. Video-assisted thoracoscopic lobectomy with bronchoplasty for lung cancer: tip regarding bronchial anastomosis. Gen Thorac Cardiovasc Surg. 2008;56:476–8. doi: 10.1007/s11748-008-0280-5. [DOI] [PubMed] [Google Scholar]
- 5.Greene PS, Heitmiller RF. Lung cancer and the left internal mammary artery graft. Ann Thorac Surg. 1994;57:1029–30. doi: 10.1016/0003-4975(94)90235-6. [DOI] [PubMed] [Google Scholar]