ABSTRACT
Purpose: To examine the effect of resistance exercises on self-reported physical function and activities of daily living (ADL) in older adults with osteoporosis or osteopenia. Methods: A search of available literature was conducted using PubMed, CINAHL, SPORTDiscus, PEDro, ProQuest Nursing and Allied Health Source, and Cochrane Controlled Trials Register. Studies were included if they involved (1) randomized controlled trials; (2) participants with osteoporosis or osteopenia; (3) resistance exercise as an intervention; and (4) self-report of physical function or ADL. Articles were independently reviewed for quality by two authors using the Physiotherapy Evidence Database (PEDro) scale. Cohen's d effect size was calculated by dividing standardized mean differences by the standard deviation to determine treatment effect in terms of physical function or ADL. Results: Five full-text articles were selected for inclusion. PEDro scores ranged from 5 to 7 (out of 10). Effect size mean differences as a result of resistance intervention ranged from 0.08 to 1.74, suggesting “trivial” to “large” effects on self-reported physical function and ADL. Conclusion: Results suggest that interventions using resistance training have a beneficial impact on the domains of physical function and ADL in participants with osteoporosis or osteopenia. More high-quality studies are needed to lend further validity to this supposition.
Key Words: activities of daily living, exercise, osteopenia, osteoporosis, resistance training
RÉSUMÉ
Objectif : Examiner l'effet des exercices avec résistance sur la fonction physique autorapportée et sur les activités de la vie quotidienne (AVQ) chez les adultes âgés aux prises avec de l'ostéoporose ou de l'ostéopénie. Méthode : Une recherche de la documentation disponible a été utilisée à l'aide des bases de données PubMed, CINAHL, SPORTDiscus, PEDro, ProQuest Nursing et Allied Health Source et du registre central Cochrane des essais contrôlés. Des études ont été retenues si elles comportaient (1) des essais contrôlés randomisés; (2) des participants souffrant d'ostéoporose ou d'ostéopénie; (3) des exercices avec résistance en tant qu'intervention ou (4) une fonction physique ou des AVQ autorapportées. La qualité des articles a fait l'objet d'une évaluation indépendante par deux auteurs, qui ont utilisé l'échelle PEDro (Physiotherapy Evidence Database). La taille de l'effet (le d de Cohen) a été calculée en divisant les différences moyennes normalisées par l'écart type afin de déterminer l'effet du traitement sur la fonction physique et sur les AVQ. Résultats : Cinq articles complets ont été sélectionnés afin d'être inclus. Les pointages à l'échelle PEDro variaient de 5/10 à 7/10. Les différences moyennes dans la taille de l'effet, à la suite d'une intervention en résistance, variaient de 0,08 à 1,74, ce qui suggère que l'étendue des effets autorapportés des exercices avec résistance sur la fonction physique et sur les AVQ varie de « minimes » à « importants ». Conclusion : Les résultats semblent indiquer que les interventions où on a recours à un entraînement avec résistance ont un effet bénéfique sur les domaines de la fonction physique et sur les AVQ chez les participants aux prises avec l'ostéoporose ou l'ostéopénie. Des études de plus grande qualité seront nécessaires pour donner plus de validité à cette hypothèse.
Mots clés : activités de la vie quotidienne, exercice, fonction, ostéoporose, ostéopénie, entraînement avec résistance, entraînement en force
Osteoporosis is a skeletal disease characterized by a significant decrease in bone mass,1–3 which can lead to an increase in bone fragility2 and susceptibility to fracture.1 Osteopenia is also a condition of decreased bone density and is considered a precursor to osteoporosis.1 Women are three times more likely than men to be diagnosed with osteoporosis during their lifespan.1,2
Hip fracture is a notable, potential consequence of osteoporosis.1 Most hip fracture survivors are unable to perform activities of daily living (ADL) without assistance; a small percentage require permanent care.1 Spine fractures4 are also a common cause of disability among older adults with osteoporosis or osteopenia,1 and can lead to loss of height, back pain, and difficulty performing ADL.4 Both hip and spine fractures can lead to lower levels of quality of life (QOL).3,5 Resistance training may provide multiple benefits to those with osteoporosis or osteopenia. Mechanical stimuli may aid in improving or maintaining bone mineral density and bone health.6 A resistance training programme may also aid in pain reduction, improve levels of fitness, and confer psychological benefits, as well as improve or maintain cognitive function and improved self-efficacy.6,7
A limited number of research studies have analyzed the effect of resistance exercises on self-reported physical function in older adults with osteoporosis or osteopenia. A recent systematic review that included many different types of exercise concluded that all forms of exercise improve physical function, pain, and physical and vitality domains of QOL.8 Li and colleagues8 reported that resistance exercise can improve objective measures of physical function in postmenopausal women. Swanenberg and colleagues9 explored the effect of resistance training in conjunction with adjunctive treatment such as vitamin D supplementation on participants with osteoporosis and found reductions in falls and increases in activity levels.9 Long-term studies (8 weeks to 30 months) that explored the effect of resistance programmes among community-based individuals demonstrated improved physical ability, decreased fall risk, and prevention of functional limitations over time.10–13
It is also necessary to measure one's subjective perception of health to fully assess the benefits of a given intervention.9 Therapists tend to view subjective measures as less reliable than objective measures because participants report their subjective experiences.14 However, this may not be true since health-related QOL questionnaires have been established as reliable and valid while many objective measures lack reliability and validity.14 Measurements of subjective phenomena that have good reliability between observers may be the most useful clinical measurement, because these subjective phenomena are more closely related to issues that matter to patients, such as disability15 or QOL. While self-reported measures are often associated with performance-based measures, the two do not measure the same concepts.16 Previous research has found that self-reported scores frequently depend on the pathological condition17 and may also be influenced by recent medical changes.18 At present, the relationship between self-reported and physical measures of function in individuals with osteoporosis has not been evaluated, and therefore should be the focus of future research.
To our knowledge, no summative review has exclusively evaluated the effect of resistance exercise on self-reported function and ADL of older adults with osteoporosis or osteopenia. The purpose of our study, therefore, was to evaluate the strength and quality of literature that examined the effect of resistance exercises using self-reported measures on physical function and ADL. We reviewed randomized controlled trials that assessed the effectiveness of resistance exercise on physical function and ADL in older adults with osteoporosis or osteopenia. This systematic review is significant because it provides clinicians with current evidence for the effectiveness of resistance exercises for self-reported physical function in order to create an evidence-based treatment approach for older adults with osteoporosis or osteopenia.
METHODS
Study design
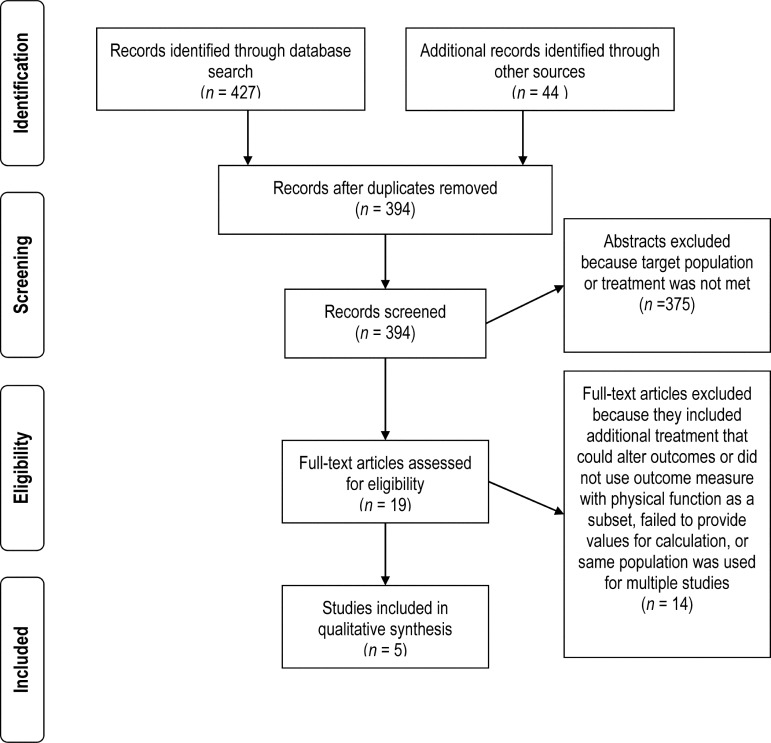
Our systematic review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines throughout the literature search and reporting phases of development. The PRISMA statement consists of a 27-item checklist and a 4-phase flow diagram, which aims to help authors improve the reporting of systematic reviews and meta-analyses. The PRISMA statement is intended for use as a basis for reporting systematic reviews of randomized trials.19 The PRISMA checklist and flow diagram are used prospectively in creating systematic reviews and meta-analyses.
Eligibility criteria
Studies were considered for inclusion if they met the following criteria: (1) randomized controlled trial, (2) participants with osteoporosis or osteopenia, (3) resistance exercise as an intervention, and (4) a self-report questionnaire with a domain of either physical function or ADL. Resistance exercise was operationally defined as site-specific resistance exercises that use isometric, concentric, or eccentric contractions against a load of the body segment or an external load. Studies were excluded if another intervention that might have influenced physical function was administered to the intervention group concurrently or if participants had an unhealed fracture or a recent fracture within the last 3 months.
Information sources
The available literature was searched for research articles published from January 1966 through August 12, 2011, to locate studies reporting the effect of resistance exercise on self-reported physical function for older adults with osteoporosis or osteopenia. The electronic databases searched were PubMed, CINAHL, SPORTDiscus, PEDro, ProQuest Nursing and Allied Health Source, and Cochrane Controlled Trials Register. Additional articles were identified through a manual search of reference lists from articles as well as a manual search of the journal Osteoporosis International from October 1990 through November 2010. Osteoporosis International was targeted since the aim of the journal is prevention, treatment, and management of osteoporosis and other metabolic bone diseases, and since some of the papers included in this review were from that journal.
Search strategy
The following combination of MeSH terms and keywords was used to search the PubMed database: (osteoporosis OR osteopenia) AND (resistance training OR strength training OR exercise) AND (outcome). Search terms for PEDro, CINAHL, and SPORTDiscus were (osteoporosis) AND (exercise) AND (function). Lastly, search terms for ProQuest included (osteoporosis) AND (resistance training) AND (outcomes). Electronic searches were limited to studies involving humans and publications in the English language.
Study selection
Titles and abstracts were reviewed independently by two reviewers (MW and GR) and assessed for inclusion or exclusion. In cases of discrepancy between the two initial reviewers, a third reviewer (CC) assessed the abstract. The articles identified for possible inclusion were then read in full and reviewed by two authors working independently. Inclusion of articles was decided by consensus between the two abstract reviewers (MW and GR) (Figure 1).
Figure 1.
Flow diagram for study inclusion.
Quality assessment
Once accepted for inclusion, each article was independently reviewed for quality by the two reviewers using the PEDro scale; any variations were resolved by consensus. The PEDro scale is an 11-item scale designed to rate the methodological quality of RCTs.20–22 The PEDro scale has been shown to be a valid measure of methodological quality of clinical trials,21 to have acceptable reliability when based on consensus judgments, and to have sufficient reliability for use in systematic reviews of physical therapy RCTs.20 Item 1, “eligibility criteria were specified,” pertains to external validity and is not included in the overall score.20 The remaining 10 items are answered as either “yes” or “no.” The “yes” answers are summed to obtain a final PEDro score out of 10; a higher score reflects higher methodological quality.
Data collection
Means and standard deviations for calculation of effect size were extracted from the included articles by one author and reviewed by a second author for accuracy. The outcomes of the self-reported measures of physical function, role-physical (a domain identified in Short Form-36 [SF-36] studies), and ADL were specifically targeted. If data were not available within the published study, the corresponding author of the paper was contacted to obtain the data.
Outcome measures
We accepted several different self-report outcome measures for inclusion in our review, even those associated with QOL measures, as long as each included a domain for physical function or ADL and each reported values for effect size calculations. Physical function is defined as the participant's performance of daily activities required to sustain oneself, including dressing, bathing, walking, meal preparation, shopping, and vehicular transportation.23 The outcome measures accepted were the SF-36, the Osteoporosis Functional Disability Questionnaire (OFDQ), the Quality of Life Questionnaire of the European Foundation for Osteoporosis (Qualeffo-41), and the Japanese Osteoporosis Quality of Life Questionnaire (JOQOL).
The SF-36 consists of 36 items that assess 8 different health domains: physical function, physical role, bodily pain, general health perceptions, vitality, social functioning, emotional role, and general mental health.24 The SF-36 has been shown to be both a valid and reliable measure of QOL.25 The SF-36 domains of physical function and role-physical were used to calculate Cohen's d effect size.
The OFDQ is a self-administered questionnaire developed to measure disability in 5 domains: overall assessment of general health and degree of back pain, a depression scale, a list of daily living activities, categories of socialization and recreation, and confidence in benefits from the planned intervention. A higher score represents increased disability for all domains, except activities of daily living where an increase in score represents decreased disability. The OFDQ has been shown to have acceptable reliability for short-term test or retest trials, and OFDQ scores were correlated with the presence of vertebral fracture.26 The entire functional disability questionnaire was used to calculate effect size.
The Qualeffo-41 consists of 48 questions and 6 visual analogue scales in 5 domains: pain, physical function, social function, general health perception, and mental function. Because the Qualeffo-41 is repeatable and coherent, it can be used for patients with osteoporosis.27 The physical function domain of the Qualeffo-41 was used to calculate effect size.
The JOQOL consists of 38 items in 6 domains: pain, activities of daily living, recreation and social activities, general health, posture and body image, and falls and psychological factors. Each domain contains 3 to 16 items, which are graded from 0 to 4, for a total score of 152. A higher score indicates higher QOL.28 The JOQOL has been confirmed as a reliable and valid tool for measuring QOL in Japanese patients with osteoporosis.29 The activities of daily living domain of the JOQOL questionnaire was used to calculate effect size.
Data items
The following information was extracted from each article: (1) characteristics of trial participants (including age, gender, and diagnosis of osteoporosis or osteopenia); (2) type of intervention and number of participants assigned to resistance exercise group; (3) type of outcome measures used in each study and length of time between baseline and follow-up; and (4) baseline and follow-up mean and standard deviation for physical function domain for the resistance exercise group or, when physical function domain was not available, ADL domain.
Summary measures
In this study, Cohen's d effect size measurement was used to determine treatment effect in terms of self-reported physical function or ADL across multiple self-report questionnaires of physical function. Effect size was calculated from baseline mean (SD) and follow-up mean (SD) for physical function or ADL domain. Cohen interpreted an effect size of 0.0–0.10 as trivial, 0.20–0.40 as small, 0.50–0.70 as moderate, and more than 0.80 as large.30 Agreement among reviewers was measured using a linear weighted kappa with 95% CIs for PEDro scoring. Conventionally, a κ<0.20 is considered poor agreement, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 strong, and >0.80 near-complete agreement.31(p.212–36)
RESULTS
A total of 394 titles and abstracts were reviewed for applicability. After assessment, 19 full-text articles were screened, and 6 were deemed appropriate for inclusion. In the case of one study that did not report the data needed for our summary analyses, we contacted the corresponding author. However, the author sent inappropriate data and did not provide the necessary data upon further contact; therefore, only 5 studies6,32–35 met our inclusion criteria (see Table 1). Most studies were excluded because they provided additional treatments, measured different outcomes, or did not use standardized outcome measures that included a self-report of physical function or ADL subset.
Table 1.
Characteristics of Studies Included in Systematic Review
| Study | Design | Participant details | Intervention and frequency | Intervention parameters | Adherence rate | Dependent variables | PEDro score | Results | Cohen's d effect size |
|---|---|---|---|---|---|---|---|---|---|
| Arnold et al.32 (2008) | RCT1 | Mean (SD) age: RG=69.1 (6.3) y, CG=67.7 (6.3) y No. of participants: RG=33, CG=2710; dropouts: RG=6, CG=4 |
50-min sessions, 3×/wk; supervised by physical therapist and assistant; duration: 20 wk |
Land exercise targeting upper and lower extremities and trunk strength (5–10 repetitions, increasing to 20–25) | 67% attendance rate for RG, with dropouts eliminated attendance was 78% | OFDQ, functional reach test, backward tandem walk, Berg Balance Scale | 7 | There were no differences in balance, function, and QOL scores between land exercises compared to no exercises. | 0.19 |
| Chien et al.6 (2005) | RCT1 | Mean (SD) age: RG=61.7 (9.0) y, CG=58.6 (9.3) y No. of participants: RG=14, CG=147; dropouts: RG=4, CG=3 |
HEP 3×/d, 7 d/wk; first introductory session with supervision; duration: 12 wk |
Resistance exercises for abdominals, low back musculature, and hip musculature (3 sets of 10 repetitions held for 3 s initially, increasing to 10 s) | 11/14 participants (78.6%) completed programme with over 90% compliance, meeting 70% compliance requirement | SF-36, trunk flexion/extension strength, spinal ROM in sagittal, frontal and transverse planes, Oswestry Disability Questionnaire | 7 | The exercise group increased spinal range of motion, velocity, trunk extensor, and flexor strength and improved in multiple domains in the SF-36 but not the physical examination domain. | RP 1.74 PF 0.27 |
| Hongo et al.33 (2007) | RCT1 | Mean (SD) age: RG=67 (5) y, CG=67 (7) y No. of participants: RG=42, CG=386; dropouts: RG=2, CG=4 |
1×/d, 5 d/wk; duration: 4 mo |
Single, unsupervised HEP: back extension (1 set of 10 repetitions) |
Not reported | JOQOL, isometric strength | 5 | QOL scores increased in the exercise group and were unchanged in the control group. Back extensor strength increased in both the control and exercise groups. | 0.46 |
| Grahn Kronhed et al.34 (2009) | RCT1 | Mean (95% CI) age: RG=71.6 (69.8–73.4) y; CG=71.2 (69.4–73.0) y No. of participants: RG=37, CG=36; dropouts: RG=6, CG=2 |
60-min sessions, 2×/wk; supervised by physical therapist; duration: 4 mo |
Back, abdomen, and extremity strengthening (5–6 sets of 15 repetitions with progressively increased load) | 80% average attendance rate | SF-36, pain, balance, handgrip and back-straightening test | 7 | The exercise group improved in multiple domains in the SF-36. | RP 0.08 PF 0.42 |
| Liu-Ambrose et al.35 (2005) | RCT2 | Mean (SD) age: RG=79.6 (2.1) y, CG=79.5 (3.2) y No. of participants: RG: 34, CG: 346; dropouts: RG: 2, CG: 2 |
50-min supervised, group-based sessions, 2×/wk; duration: 25 wk |
Resistance training targeting upper and lower extremities and trunk strength (2 sets of 10–15 repetitions at 50–60% 1RM, increased to 2 sets of 6–8 repetitions at 75–85% 1 RM) |
Average compliance of 85% | Qualeffo-41, Oswestry Disability Questionnaire | 6 | Resistance and agility training significantly improved QOL. | 0.14 |
RCT1=randomized controlled trial with true control group; RG=research group; CG=control group; OFDQ=Osteoporosis Functional Disability Questionnaire; QOL=quality of life; HEP=home exercise programme; ROM=range of motion; SF-36=Short Form-36; RP=Role physical; PF=physical function; JOQOL=Japanese Osteoporosis Quality of Life Questionnaire; RCT2=randomized controlled trial with the control group receiving intervention; 1RM=1 repetition maximum; Qualeffo-41=Quality of Life Questionnaire of the European Foundation for Osteoporosis.
Sample sizes of the 5 studies ranged from 28 to 98. All study designs were randomized controlled trials. The control group in each study consisted of aged matched participants in similar numbers to the intervention group. The control groups in four studies were instructed not to perform any additional activities that were not performed before the study6,32–34; the control group in the remaining study performed stretching (sham exercise) for the duration of the study but no additional activities.35 PEDro scores for the studies ranged between 5 and 7 (see Table 2); agreement between reviewers on study quality was 93% (κ=0.82; 95% CI, 0.63–0.92). Several different standardized QOL outcome assessment tools and subsets were represented in the studies, including the role-physical and physical function subsets of the SF-36 (twice), the physical function subset of the Qualeffo-41, and the functional ability domain of the OFDQ and the JOQOL. Effect size measures yielded a range from trivial (0.8) to large (1.74).6,32–35
Table 2.
Methodological Quality of Included Studies (PEDro Scale)
| Arnold et al.32 |
Chien et al.6 |
Hongo et al.33 |
Grahn Kronhed et al.34 |
Liu-Ambrose et al.35 |
|
|---|---|---|---|---|---|
| 1. Eligibility criteria specified* | Y | Y | Y | Y | Y |
| 2. Random subject allocation | Y | Y | Y | Y | Y |
| 3. Allocation was concealed | Y | Y | N | N | N |
| 4. Groups were similar at baseline | Y | Y | Y | Y | Y |
| 5. Blinding of all subjects | N | N | N | N | N |
| 6. Blinding of therapists administering therapy | N | N | N | N | N |
| 7. Blinding of assessors | Y | Y | N | Y | Y |
| 8. Measures obtained from more than 85% of initial subjects | N | N | Y | Y | Y |
| 9. All subjects received treatment or control. If not, data analyzed by “intention to treat” | Y | Y | N | Y | N |
| 10. Results of between-group comparisons reported for at least one key outcome | Y | Y | Y | Y | Y |
| 11. Provides both point measures and measures of variability for one key outcome | Y | Y | Y | Y | Y |
| TOTAL SCORE: | 7/10 | 7/10 | 5/10 | 7/10 | 6/10 |
PEDro item 1 is not used to calculate the overall PEDro score.
Y=Yes; N=No.
DISCUSSION
The purpose of our study was to investigate the effect of resistance exercises on self-reported physical function in older adults with osteoporosis or osteopenia using various outcome measurement tools. Cohen's d effect size was calculated to determine the true magnitude of the interventions on physical function and ADL. The results suggest that interventions using resistance training can have a beneficial impact on the domains of physical function and ADL in older adults with osteoporosis or osteopenia. Four studies32–35 found a trivial to small effect, one other study6 showed a large effect. Variation in effect may be due to multiple characteristics of the study, including exercise protocol and compliance rate. None of the included studies performed a follow up assessment beyond 25 weeks, which makes it difficult to determine long-term effects of resistance exercise in this population; however, all studies showed a positive effect in physical function or ADL within the time limits of the study.
The exercise protocols focused on back and core strengthening and on upper and lower extremity and trunk strengthening. Variations in frequency and duration were noted. Three of the included articles targeted resistance exercises 2–3×/week, ranging from 50 to 60 minutes in duration for each session, with direct supervision by a physical therapist or other instructor.32,34,35 Effect sizes for the resistance intervention in these studies range from trivial to small.
Participants in the study by Chien and colleagues6 performed home-based resistance exercises focusing on the abdomen, low back, and hip without direct supervision. The exercise protocol was performed 3×/day, 7 days/week. Participants in the study by Hongo and colleagues,33 which also used a home-based protocol without direct supervision, performed one back resistance exercise 10×/day, 5 days/week. Effect sizes for Chien and colleagues6 were small (0.27) for the physical function domain and large (1.74) for the role-physical domain of the SF-36, whereas Hongo and colleagues'33 intervention had a small effect (0.46).
Various self-report outcome measures were examined in this review, some of which include a domain of physical function while others include a domain of ADL. A study by Jette23 includes ADL within the definition of physical function, making it difficult to differentiate between the two terms and, thus, to determine whether the effects were influenced by the specific outcome measure used.23
An interesting finding is the notably larger effect size (1.74) in the study by Chien and colleagues6 relative to the effect sizes found for the other four studies, which ranged from 0.08 to 0.46.32–35 Based on our observations, frequency of and compliance with the exercise programme may have a more positive effect in older adults with osteoporosis than exercises that either target specific muscle groups or are a more generalized exercise programme. Future studies should examine the frequency, time, and duration of exercises rather than focusing on the exercise protocols alone. In the same study,6 participants were considered to have dropped out if they did not maintain the required 70% completion rate. As a result of this compliance standard, 2 of 14 participants in the intervention group were excluded because of low compliance. Their results may therefore show greater improvements in function for the remaining highly compliant patients, leading to a higher treatment effect compared to participants in those studies that did not set a compliance standard. Although Chien and colleagues' sample size is the smallest of all the studies, effect sizes are only marginally influenced by sample size.36,37 The effectiveness of exercise therapy cannot be established without first determining compliance with the exercise programme.38
Compared to no intervention, resistance exercise does appear to yield positive effects. A recent meta-analysis by Li and colleagues8 reviewed four randomized controlled trials to study the effect of exercise programmes on QOL in postmenopausal women with osteopenia or osteoporosis. The authors reported that pain, vitality, and physical function domains had significant improvements in the exercise groups compared to the control groups.8 In contrast to this meta-analysis, which included all forms of exercise as well as all domains within QOL questionnaires,8 our systematic review focused specifically on the effect size of resistance exercise on perception of physical function and ADL for older adults with osteoporosis or osteopenia. Research and community programmes support the notion that resistance exercise programmes improve physical ability, decrease fall risks, and prevent functional limitations.10 The results of our systematic review, combined with those presented by Li and colleagues,8 suggest that resistance exercises can provide potential benefit for older adults with osteoporosis or osteopenia in terms of both objective and subjective measures of function. Future studies should aim to establish a correlation between subjective and objective measures of function for this population.
Compared to other studies6,8,32–35 that describe how resistance training affects QOL in older adults with osteoporosis, the present review focused primarily on patient perceptions of physical function and ADL domains as reported in multiple outcome assessment questionnaires. Our focus was on assessing effect sizes of the interventions used to determine the true magnitude of the intervention as an exclusive treatment source.30 Swanenberg and colleagues9 researched the effect of resistance training on participants with osteoporosis, but also included other forms of treatment (e.g., vitamin D supplementation) in conjunction with resistance training; their study demonstrated an 89% reduction in reported falls for the experimental (resistance exercise) group. These results correspond with our finding that resistance training does have a beneficial effect for older adults with osteoporosis or osteopenia; however, we do not know how much of the 89% reduction in falls observed by Swanenberg and colleagues9 was due to the resistance training and how much was due to increased bone mass as a result of vitamin D supplementation.
To improve the integrity of our study, only randomized controlled trials were included in the review. Effect size measures are thus more specific to the resistance exercise intervention and more closely reflect the outcome of this form of treatment approach in a supervised or quasi-supervised setting within the community.
Health related QOL outcomes distinguish between the objective and subjective meanings of a person's QOL depending on health, disability, and morbidity.23 Although many therapists believe that measuring impairments through objective clinical outcomes is more reliable, health related QOL tools have been well studied and are recognized as both reliable and valid.14 Our results suggest that clinicians and other health care professionals may see increased benefit from prescribing resistance exercise protocols with increased frequency and duration to improve physical function for older adults with osteoporosis or osteopenia.
Our systematic review had several limitations. We were limited to studies published in English. All studies included in our review scored between 5 and 7 on the PEDro scale, which we defined as moderate quality following Moseley and colleagues,39 who identified PEDro scores ≥5 as moderate to high quality. There is a risk that the effects generated in the study are reflective of the moderate quality. None of the included articles examined the effects of resistance training on self-reported function beyond 25 weeks. These findings only represent short-term follow up. It would be interesting to continue to follow participants post-treatment to identify any long-term effects.
CONCLUSION
Research involving older adults with osteoporosis or osteopenia often attempts to answer questions related to physiology, pharmacologic supplementation, bone mineral density, fracture risk, fall risk, and QOL. The use of resistance training as an intervention in this population shows a range of effect sizes, from trivial to large, on self-reported function and ADL. Future studies examining the long-term effects of resistance exercise on functional abilities would be valuable in determining exercise programmes.
Current literature and summary
Resistance training is known to decrease both fall risk and risk of fractures. This systematic review shows that resistance exercises can increase participant self-reported physical function and activities of daily living (ADL) in older adults with osteoporosis or osteopenia. Effect sizes for the interventions in the included studies ranged from 0.08 to 1.74, representing a trivial to large effect on self-reported function and ADL.
Key Messages
What is already known on this topic
Resistance exercises have been shown to improve bone mineral density and reduce risk of future fracture in individuals with osteoporosis.
What this study adds
Resistance exercise can improve self-reported physical function in patients with osteoporosis or osteopenia with an effect size ranging from trivial to large. Preliminary evidence shows that greater exercise compliance and increased intensity may be associated with higher levels of effect when measuring functional status.
Appendix
Database: PubMed
Osteoporosis
Osteopenia
1 OR 2
Resistance training
Strength training
Exercise
4 OR 5 OR 6
Outcome
3 AND 7 AND 8
Limits: Studies involving humans and publications in the English language
Database: PEDro, CINAHL, SPORTDiscus
Osteoporosis
Exercise
Function
1 AND 2 AND 3
Limits: Studies involving humans and publications in the English language
Database: ProQuest Nursing and Allied Health Source
Osteoporosis
Resistance training
Outcome
1 AND 2 AND 3
Limits: Studies involving humans and publications in the English language
Physiotherapy Canada 2012; 64(4);386–394; doi:10.3138/ptc.2011-31BH
References
- 1.Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367(9527):2010–8. doi: 10.1016/S0140-6736(06)68891-0. http://dx.doi.org/10.1016/S0140-6736(06)68891-0. Medline:16782492. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization [WHO] Scientific Group on the Prevention and Management of Osteoporosis. Prevention and management of osteoporosis. Geneva: The Organization; 2003. (Technical Report Series 921). [PubMed] [Google Scholar]
- 3.Bergland A, Thorsen H, Kåresen R. Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int. 2011;22(6):1863–71. doi: 10.1007/s00198-010-1435-7. http://dx.doi.org/10.1007/s00198-010-1435-7. Medline:21060992. [DOI] [PubMed] [Google Scholar]
- 4.Kessenich CR, Guyatt GH. Domains of health-related quality of life in elderly women with osteoporosis. J Gerontol Nurs. 1998;24(11):7–13. doi: 10.3928/0098-9134-19981101-06. Medline:10392089. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128(10):793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. Medline:9599190. [DOI] [PubMed] [Google Scholar]
- 6.Chien MY, Yang RS, Tsauo JY. Home-based trunk-strengthening exercise for osteoporotic and osteopenic postmenopausal women without fracture–a pilot study. Clin Rehabil. 2005;19(1):28–36. doi: 10.1191/0269215505cr844oa. http://dx.doi.org/10.1191/0269215505cr844oa. Medline:15704506. [DOI] [PubMed] [Google Scholar]
- 7.Prior JC, Barr SI, Chow R, et al. Prevention and management of osteoporosis: consensus statements from the Scientific Advisory Board of the Osteoporosis Society of Canada. 5. Physical activity as therapy for osteoporosis. CMAJ. 1996;155(7):940–4. Medline:8925493. [PMC free article] [PubMed] [Google Scholar]
- 8.Li WC, Chen YC, Yang RS, et al. Effects of exercise programmes on quality of life in osteoporotic and osteopenic postmenopausal women: a systematic review and meta-analysis. Clin Rehabil. 2009;23(10):888–96. doi: 10.1177/0269215509339002. http://dx.doi.org/10.1177/0269215509339002. Medline:19717503. [DOI] [PubMed] [Google Scholar]
- 9.Swanenburg J, de Bruin ED, Stauffacher M, et al. Effects of exercise and nutrition on postural balance and risk of falling in elderly people with decreased bone mineral density: randomized controlled trial pilot study. Clin Rehabil. 2007;21(6):523–34. doi: 10.1177/0269215507075206. http://dx.doi.org/10.1177/0269215507075206. Medline:17613583. [DOI] [PubMed] [Google Scholar]
- 10.Seguin R, Nelson ME. The benefits of strength training for older adults. Am J Prev Med. 2003;25(3) Suppl 2:141–9. doi: 10.1016/s0749-3797(03)00177-6. http://dx.doi.org/10.1016/S0749-3797(03)00177-6. Medline:14552938. [DOI] [PubMed] [Google Scholar]
- 11.Renno A, Granito R, Driusso P, et al. Effects of an exercise program on respiratory function, posture and on quality of life in osteoporotic women: a pilot study. Physiotherapy. 2005;91(2):113–8. http://dx.doi.org/10.1016/j.physio.2004.09.020. [Google Scholar]
- 12.Madureira MM, Bonfá E, Takayama L, et al. A 12-month randomized controlled trial of balance training in elderly women with osteoporosis: improvement of quality of life. Maturitas. 2010;66(2):206–11. doi: 10.1016/j.maturitas.2010.03.009. http://dx.doi.org/10.1016/j.maturitas.2010.03.009. Medline:20395080. [DOI] [PubMed] [Google Scholar]
- 13.Korpelainen R, Keinänen-Kiukaanniemi S, Heikkinen J, et al. Effect of impact exercise on bone mineral density in elderly women with low BMD: a population-based randomized controlled 30-month intervention. Osteoporos Int. 2006;17(1):109–18. doi: 10.1007/s00198-005-1924-2. http://dx.doi.org/10.1007/s00198-005-1924-2. Medline:15889312. [DOI] [PubMed] [Google Scholar]
- 14.Resnik L, Dobrzykowski E. Guide to outcomes measurement for patients with low back pain syndromes. J Orthop Sports Phys Ther. 2003;33(6):307–16. doi: 10.2519/jospt.2003.33.6.307. discussion 317–8 Medline:12839205. [DOI] [PubMed] [Google Scholar]
- 15.Rothstein JM. Objective versus subjective: kudzu terminology. Physiother Can. 2008;60(2):103–5. doi: 10.3138/physio.60.2.103. http://dx.doi.org/10.3138/physio.60.2.103. Medline:20145773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoeymans N, Feskens EJM, van den Bos GAM, et al. Measuring functional status: cross-sectional and longitudinal associations between performance and self-report (Zutphen Elderly Study 1990–1993) J Clin Epidemiol. 1996;49(10):1103–10. doi: 10.1016/0895-4356(96)00210-7. http://dx.doi.org/10.1016/0895-4356(96)00210-7. Medline:8826989. [DOI] [PubMed] [Google Scholar]
- 17.Pua YH, Wrigley TV, Collins M, et al. Self-report and physical performance measures of physical function in hip osteoarthritis: relationship to isometric quadriceps torque development. Arthritis Rheum. 2009;61(2):201–8. doi: 10.1002/art.24277. http://dx.doi.org/10.1002/art.24277. Medline:19177533. [DOI] [PubMed] [Google Scholar]
- 18.Daltroy LH, Larson MG, Eaton HM, et al. Discrepancies between self-reported and observed physical function in the elderly: the influence of response shift and other factors. Soc Sci Med. 1999;48(11):1549–61. doi: 10.1016/s0277-9536(99)00048-9. http://dx.doi.org/10.1016/S0277-9536(99)00048-9. Medline:10400256. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. http://dx.doi.org/10.1016/j.ijsu.2010.02.007. Medline:20171303. [DOI] [PubMed] [Google Scholar]
- 20.Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. Medline:12882612. [PubMed] [Google Scholar]
- 21.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–33. doi: 10.1016/s0004-9514(09)70043-1. http://dx.doi.org/10.1016/S0004-9514(09)70043-1. Medline:19463084. [DOI] [PubMed] [Google Scholar]
- 22.Verhagen AP, de Vet HCW, de Bie RA, et al. The art of quality assessment of RCTs included in systematic reviews. J Clin Epidemiol. 2001;54(7):651–4. doi: 10.1016/s0895-4356(00)00360-7. http://dx.doi.org/10.1016/S0895-4356(00)00360-7. Medline:11438404. [DOI] [PubMed] [Google Scholar]
- 23.Jette AM. Using health-related quality of life measures in physical therapy outcomes research. Phys Ther. 1993;73(8):528–37. doi: 10.1093/ptj/73.8.528. Medline:8337240. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. http://dx.doi.org/10.1097/00005650-199206000-00002. Medline:1593914. [PubMed] [Google Scholar]
- 25.Brazier JE, Harper R, Jones NMB, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4. doi: 10.1136/bmj.305.6846.160. http://dx.doi.org/10.1136/bmj.305.6846.160. Medline:1285753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helmes E, Hodsman A, Lazowski D, et al. A questionnaire to evaluate disability in osteoporotic patients with vertebral compression fractures. J Gerontol A Biol Sci Med Sci. 1995;50(2):M91–8. doi: 10.1093/gerona/50a.2.m91. http://dx.doi.org/10.1093/gerona/50A.2.M91. [DOI] [PubMed] [Google Scholar]
- 27.Lips P, Cooper C, Agnusdei D, et al. Working Party for Quality of Life of the European Foundation for Osteoporosis. Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO) Osteoporos Int. 1999;10(2):150–60. doi: 10.1007/s001980050210. http://dx.doi.org/10.1007/s001980050210. Medline:10501796. [DOI] [PubMed] [Google Scholar]
- 28.Miyakoshi N, Itoi E, Kobayashi M, et al. Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos Int. 2003;14(12):1007–12. doi: 10.1007/s00198-003-1510-4. http://dx.doi.org/10.1007/s00198-003-1510-4. Medline:14557854. [DOI] [PubMed] [Google Scholar]
- 29.Kumamoto K, Nakamura T, Suzuki T, et al. Validation of the Japanese Osteoporosis Quality of Life Questionnaire. J Bone Miner Metab. 2010;28(1):1–7. doi: 10.1007/s00774-009-0125-z. http://dx.doi.org/10.1007/s00774-009-0125-z. Medline:19826753. [DOI] [PubMed] [Google Scholar]
- 30.Cohen J. Statistical power analysis for the behavioral sciences. Revised ed. New York: Academic Press; 1977. [Google Scholar]
- 31.Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York: Wiley; 1981. [Google Scholar]
- 32.Arnold CM, Busch AJ, Schachter CL, et al. A randomized clinical trial of aquatic versus land exercise to improve balance, function, and quality of life in older women with osteoporosis. Physiother Can. 2008;60(4):296–306. doi: 10.3138/physio.60.4.296. http://dx.doi.org/10.3138/physio.60.4.296. Medline:20145763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hongo M, Itoi E, Sinaki M, et al. Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: a randomized controlled trial. Osteoporos Int. 2007;18(10):1389–95. doi: 10.1007/s00198-007-0398-9. http://dx.doi.org/10.1007/s00198-007-0398-9. Medline:17572835. [DOI] [PubMed] [Google Scholar]
- 34.Grahn Kronhed A-C, Hallberg I, Ödkvist LO, et al. Effect of training on health related quality of life, pain and falls in osteoporotic women. Adv Physiother. 2009;11(3):154–65. http://dx.doi.org/10.1080/14038190902896659. [Google Scholar]
- 35.Liu-Ambrose TY, Khan KM, Eng JJ, et al. Both resistance and agility training reduce back pain and improve health-related quality of life in older women with low bone mass. Osteoporos Int. 2005;16(11):1321–9. doi: 10.1007/s00198-005-1842-3. http://dx.doi.org/10.1007/s00198-005-1842-3. Medline:15702262. [DOI] [PubMed] [Google Scholar]
- 36.Rosenthal R, Rosnow RL. Essentials of behavioral research: methods and data analysis. 2nd ed. New York: McGraw-Hill; 1991. [Google Scholar]
- 37.Rosnow RL, Rosenthal R. Computing contrasts, effect sizes, and counternulls on other people's published data: general procedures for research consumers. Psychol Methods. 1996;1(4):331–40. http://dx.doi.org/10.1037/1082-989X.1.4.331. [Google Scholar]
- 38.Sluijs EM, Kok GJ, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;73(11):771–82. doi: 10.1093/ptj/73.11.771. discussion 783–6 Medline:8234458. [DOI] [PubMed] [Google Scholar]
- 39.Moseley AM, Herbert RD, Sherrington C, et al. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro) Aust J Physiother. 2002;48(1):43–9. doi: 10.1016/s0004-9514(14)60281-6. Medline:11869164. [DOI] [PubMed] [Google Scholar]