Abstract
Background and objectives: In the last few years, several studies have focused on short-term treatment effects of exercise therapy. However, there is a lack of knowledge concerning the long-term treatment effects recorded after several years. Hence, this study was performed to investigate the short- and long-term effects of supervised physical training on functional ability, self-rated pain and disability in secondary prevention of low back pain. Methods: One hundred and eighty-three hospital employees with chronic low back pain were randomly assigned either to back school (comparison group), or three-months supervised physical training including a back school (exercise group). Various measurements of functional ability were performed and subjects completed questionnaires on self-rated pain, disability, and general well-being before treatment, immediately after intervention, and at six-months follow-up. At one-year and at ten-years follow-up participants evaluated treatment effectiveness. Results: Out of 183 employees, 148 completed the program. Participation at follow-ups ranged from 66 to 96%. Supervised physical training significantly improved muscular endurance and isokinetic strength during a six-months follow-up, and effectively decreased self-rated pain and disability during a one-year follow-up. At ten-years follow-up the subjects’ assessment of the effectiveness of treatment was significantly better in the exercise group. Conclusions: Supervised physical training effectively improved functional capacity and decreased LBP and disability up to one-year follow-up. The subjects’ positive evaluation of the treatment effect at ten-years follow-up suggests a long-term benefit of training.
Keywords: Randomized clinical trial, Supervised physical training, Back school, Hospital employees, Low back pain
Introduction
Low back pain (LBP) is highly prevalent in the general population and has been investigated in many studies. Results suggest that a variety of factors contribute to the occurrence of LBP, but still the etiology is not understood. Hence intervention and prevention strategies become more and more important and evidence-based recommendations require thorough investigation of the long-term effectiveness of frequently administered therapy concepts.
There exists a variety of different therapy concepts ranging from passive to active therapy. Passive therapy concepts such as medication, massage, and ultrasound have been found to lack documented effectiveness, only manipulation revealed to be of some value for the relief of acute LBP [5]. However, in this context the occurrence of spontaneous remissions of acute LBP should be considered [25]. For the therapy of chronic LBP, active therapies play a major role. Active therapies comprise a broad range of different concepts ranging from back school programs, and aerobic exercise to intensive strengthening exercises with training devices. There is evidence that exercises [38] and comprehensive multidisciplinary programs including active physical and ergonomic training and psychological pain management [2] may be useful for the therapy of chronic LBP.
The ‘Deconditioning Syndrome’ as described by Mayer and Gatchel [32] is one of the underlying hypothesis of intensive training programs that aim to improve muscular stabilization and functional capacity of the patients. There is evidence that the dosage of the training, i.e. the resistance and number of repetitions per session, as well as the total number of sessions, are very important for the outcome of the therapy of chronic LBP patients [26]. Moreover, not only functional but also psychological effects can be expected to contribute to the effectiveness of a training therapy by increasing the level of activity and self-confidence [26], and by modifying the perception of pain and disability [27].
It has been shown that exercise programs are effective in decreasing LBP intensity and disability [13], and in improving functional ability such as back extension strength, mobility, and endurance [31]. However, there is still a lack of knowledge concerning the long-term treatment effects over years. It might be hypothesized that strengthening exercises that are administered frequently over a certain period of time, may modify not only psychological but also neuromuscular patterns thus contributing to a long-term benefit of the therapy. In times of increasing costs in the health care sector this may certainly be of particular interest.
The aim of the current study was to investigate the short and long-term benefit of strengthening exercises using training devices (also referred to as “supervised physical training” later on), combined with a back school program, in comparison to a back school program only. Effectiveness was assessed with regard to subjective and objective outcome variables addressing the following issues: (1) Is there a prolonged increase in functional capacity in the exercise group over a six-months follow-up period? (2) Are there differences between the exercise and the comparison group in terms of self-rated disability, pain intensity and general well being at one-year follow-up? (3) Are there any long-term treatment effects regarding self-rated pain and disability at ten-years follow-up? and finally, (4) Do subjects attribute changes in self-rated LBP intensity and disability to the intervention they attended ten years ago?
Materials and methods
Study population
In 1991 all employees of a large university hospital were requested to complete a modified version of the Nordic Questionnaire on LBP (n=5,100). Out of subjects who returned the questionnaires (n=3,621, response rate=71%), potential candidates were recruited for the current study. Prior to a first contact they were randomly assigned to the exercise or comparison group by means of a computer randomization program. Since the first recruitment did not deliver the required number of subjects, a second recruitment was performed in 1992, finally resulting in a number of 358 participants. Inclusion criteria were: more than 30 days LBP within the preceding 12 months (first recruitment) or 8–30 days LBP together with reported disability in daily tasks within the preceding 12 months (second recruitment); age between 20 and 55 years; ability to read and write German or Italian. Exclusion criteria were: cardiovascular or metabolic diseases (angina pectoris, previous heart surgery, cardiac failure, hypertension, diabetes, hyperthyroidism), progressive radicular neurological defects, inflammatory diseases of the spine, previous spinal surgery, other non rheumatic diseases that may account for LBP (i.e. kidney, gynecological disease). Furthermore, subjects who participated in regular strength training within the last six months, who aspired to change job, or worked less than 50%, as well as pregnant women were excluded. Subjects who fulfilled our criteria were randomly allocated to either the exercise or the comparison group. All participants received an oral and written explanation of the study and were requested to sign an informed consent form. The study was approved by the local Ethics Committee.
Programs for the exercise and the comparison group
The control program comprised a low back school, consisting of three sessions, each lasting 1 h. In the first session information about the functional anatomy of the spine was provided, and subjects were instructed in lifting techniques. The second session dealt with the use of mental stress coping strategies. Further, the necessity of physical activity with respect to LBP was emphasized. In the third session, subjects were advised in sports activities and optimal lifting techniques for everyday life situations.
The exercise program comprised the same low back school as described above and further physical exercises based on concepts of medical training therapy [16], and sequence exercise training on Norsk machines [12]. The whole program lasted three months and included three phases of individual training with a duration of four weeks each. In the first phase (first to fourth week) subjects attended a back school course once a week. Training therapy was performed twice a week. Each session lasted at least 1 h and comprised static and dynamic exercises using mainly pulleys and small weights. According to the individual’s physical tolerance, weight, number of repetitions, speed and range of movement were adjusted and gradually increased during the first phase. In the next phase (fifth to eighth week), the more demanding sequence training was performed three times a week, lasting 1 h each. The training was performed on Norsk machines and aimed to increase whole body strength and endurance performing a minimum of 2×15 repetitions for each exercise. Either loading on the spine or the number of repetitions or both was increased throughout the intervention period and individual records were kept to indicate the subjects’ progress. The third phase (9th to 12th week) comprised sequence training twice a week lasting 1 h each.
Each training session started with a warming up procedure. This procedure comprised low impact aerobics and subsequent stretching. Training was supervised by a physiotherapist to secure the appropriate performance of the exercises. Individual instructions and determination of exercise levels took place at the start of the intervention program and were repeated at a two-weeks interval.
Outcome measurements before and after intervention and at six-months, one-year and ten-years follow-up
Prior to the start of the intervention study all participants were thoroughly examined and completed several functional tests and questionnaires. The examiners were not blinded to group assignment.
Normative values
In a previous study, normative values for the functional tests had been recorded in a group of 121 healthy subjects (Table 1) [35]. Isokinetic strength, isometric muscular endurance, and lifting capacity were recorded. Normative values for aerobic capacity measurements had been already available [36]. All data retrieved from functional tests in the current study have been expressed in % of those normative values.
Table 1.
Normative data (median) obtained from hospital employees (as reported by Oliveri et al. [35])
| Men n=35 | Women n=86 | |
|---|---|---|
| Muscular endurance (s) | ||
| Trunk flexion | 120 | 120 |
| Trunk extension | 39 | 30 |
| Arm holding | 162 | 110 |
| Squatting | 90 | 67 |
| Lifting capacity (kg) | ||
| Lower lifting test | 36.5 | 24.0 |
| Upper lifting test | 21.5 | 14.0 |
| Isokinetic strength (% Nm/body weight) | 278 | 237 |
| Range of motion | 20–32 years: 81° | |
| 33–43 years: 71° | ||
| 44–57 years: 64° | ||
Clinical investigation
An extended clinical investigation was performed. Body height and weight, and blood pressure were measured. If the systolic and diastolic values exceeded 180 and 110, respectively, special attention was paid to these subjects in the functional tests later on. An inspection concerned the curvature of the spine and the pelvis (distortion, different height), and the evaluation of the myotonus of the erector spinae muscle. The straight leg raising test was performed to evaluate the presence of radiating pain. An angle <50° was characterized as “abnormal”. Further, the neurological status was investigated with respect to strength during walking on the toes and the heels or during squatting. Further, reflexes in the patella and the ankle jerks were examined. The iliopsoas and the rectus muscles were evaluated with respect to muscle length.
Lifting capacity
A modified version of the validated PILE test [29] was used to evaluate the subjects’ lifting capacity (for further details see Appendix). For both, the upper and the lower lifting test, the maximum weight lifted was recorded. For further analysis an index (“Lifting”) was created by averaging the results of the upper and the lower lifting test.
Isokinetic trunk strength
Isokinetic trunk strength, expressed as peak torque in Newton-meters (Nm), was recorded at velocities of 60, 120 and 150°/s using the Cybex TEF Modular Component isokinetic dynamometer from Lumex Inc., Ronkonkoma, NY [33] (for further details see Appendix). For subsequent analysis, an index (“Isokinetic Strength”) was formed, which was the mean of all six peak torques (related to body weight) at three different angle velocities measured in flexion and extension.
Range of motion
An inclinometer (EDI, Cybex, Lumex Inc.) was used to measure range of motion in flexion, extension and side bending [21] (for further details see Appendix). The subject’s total mobility was obtained by adding results of flexion and extension.
Isometric muscular endurance
Muscular endurance was recorded in trunk extension (modified version of the Soerensen test [4]) and flexion as well as in squatting position. Moreover, muscular endurance of the upper arm and shoulder girdle muscles was measured. Endurance time was recorded in seconds (for further details see Appendix).
Out of endurance measurements performed in trunk flexion, squatting, and arms holding an index (“Muscular endurance”) was derived from the average of the tests.
Aerobic capacity
Subjects had to step on a box (height 30 cm) according to a metronome at a sequence of 24 times /min. After 3 min the test was stopped and the subject’s heart rate was measured for another minute in sitting position. For subsequent analysis the mean of the heart rate recorded after 30, 60 and 180 s was determined [36].
Questionnaires: The following questionnaires were included to obtain information about:
Frequency and duration of LBP (Nordic questionnaire [22]) and other musculoskeletal disorders [23]
Disability due to LBP (Roland and Morris questionnaire [37], Waddell questionnaire [39] in modified version)
LBP intensity (Numeric Rating Scale [8] for actual pain and greatest and lowest pain within the last seven days, Quantitative Pain Drawing [6], and number of days with intake of pain relieving drugs within the last week)
Pain characteristics (short-form Mc Gill questionnaire [34])
General well being (General well being questionnaire [9] in modified version)
General beliefs (Sense of coherence questionnaire [1]).
Further questions were added concerning sociodemographic and occupational data, workload, and frequency of sports activities, regular fitness or strengthening exercise habits.
At discharge from the program (after three months), subjects of both groups were requested to complete again the same questionnaires. Additionally, the exercise group performed all functional tests. This group was also requested to evaluate the effectiveness of the treatment with respect to whether pain (no pain any more, less pain, slightly less pain, as much as before, more pain) or functional capacity to perform daily tasks had changed (substantially improved, partly improved, no improvement), and whether they were satisfied with the overall benefit of the treatment (very good, rather good, rather bad, very bad). Out of these items an index was built for further analysis (index “self-assessed treatment effectiveness”).
Six months after discharge from the program (six-months follow-up), the entire initial evaluation was repeated in both groups and all subjects were requested to evaluate the treatment they had received.
At one-year follow-up only questionnaires were administered in both groups and again subjects were inquired about the benefit of the treatment they had received.
At ten-years follow-up a shortened version of the original questionnaires was administered comprising the Nordic Questionnaire on LBP, the Roland and Morris questionnaire, and the Numeric Rating Scale on LBP intensity. Questions concerning the long-term treatment effectiveness were added. Since a large proportion of subjects had left the hospital within ten-years follow-up, two reminders were posted and subjects were contacted by phone to obtain as many answers as possible.
Table 2 lists all tests used in the study.
Table 2.
Clinical and functional assessment, questionnaires, and self-assessment of treatment effectiveness within the study period
| Test | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|
| Clinical examination | E/C | ||||
| Functional capacity | E/C | E | E/C | ||
| Lifting capacity | |||||
| Isokinetic strength | |||||
| Muscular endurance | |||||
| Aerobic capacity | |||||
| Range of motion | |||||
| Questionnaires | E/C | E/C | E/C | E/C | E/Ca |
| Self-assessment of treatment effectiveness | E | E/C | E/C | E/Ca |
T1 Pretreatment; T2 Posttreatment; T3 six-months follow-up; T4 one-year follow-up; T5 ten-years follow-up; E Exercise group; C Comparison group
ashortened questionnaire
Statistical analysis
For analysis only subjects having completed the intervention program have been considered. Dropouts, i.e. subjects who did not complete the program, were requested to indicate their intensity of LBP on a numeric rating scale at six-months follow-up. The Wilcoxon matched-pairs signed-ranks test was used to analyze whether significant changes in pain intensity occurred without even having participated in strength exercises thus leading to biased results. At ten-years follow-up again all subjects, including the dropouts, were requested to complete the follow-up questionnaire. Answers of dropouts and non-dropouts were compared for pain intensity and self-assessed treatment effectiveness.
Since functional outcome variables and the questionnaire scales were approximately normally distributed, parametric statistics were used.
Comparability of groups (exercise and comparison group) for data obtained at baseline was assessed using the Mann-Whitney U test for ordinal data, the Chi square test for nominal data, and the two sample t test for continuous data. Similarly categorical variables recorded at ten-years follow-up were analyzed. Analysis of variance with repeated measures (group × time) was used to identify changes of the functional outcome variables between pretreatment and six-months follow-up. Similarly, changes of the outcome variables self-rated pain, disability, and general well being were analyzed for the one-year follow-up period and changes in self-rated pain intensity and disability for the ten-years follow-up period. Only subjects attending all evaluations in the respective time intervals were included in the analysis. If there was one missing observation for variables that were recorded at all follow-ups (pain on a numeric Rating Scale, Roland and Morris Index), the missing one was calculated out of the mean of the data obtained at the other follow-ups. If only the ten-years follow-up or more than one observation was missing, this person was excluded from analysis.
Global changes within the respective time interval were assessed by noting the significance of the time effect from the repeated ANOVA.
To determine the internal consistency of each of the indices “Isokinetic Strength”, “Lifting”, “Muscular Endurance”, and “Self- Assessed Treatment Effectiveness”, Cronbach’s alpha coefficients were computed [7]. Further, the reliability of the outcome measures between pre- and posttreatment measurements was analyzed and expressed as Pearson correlation coefficient.
All analyses were performed with the SAS (statistical analysis system, Cary, NC, USA) software package (Release 6.12). Significance was defined as p<0.05.
Results
Study sample
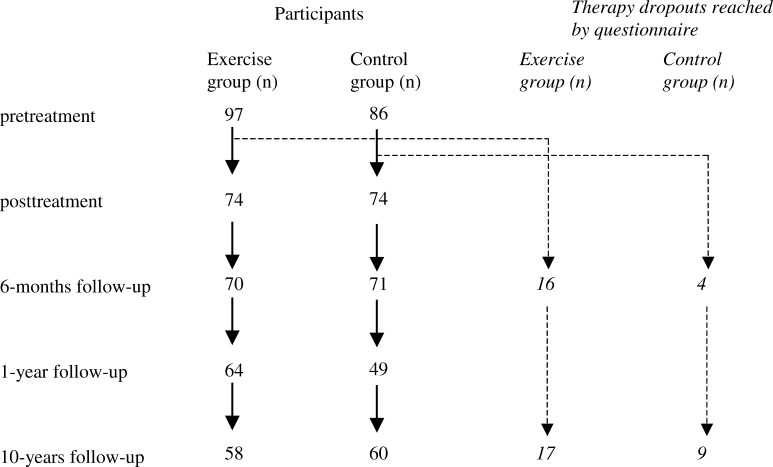
From all subjects who returned the questionnaire in 1991, 358 met the criteria to be included in the current study. Prior to its start, 175 subjects retreated from participation, half of them (50%) due to lack of time. The second most frequent reason was end of employment at the time when the treatment should start (27%), followed by other reasons such as diseases, accidents, and participation in regular strength training thus failing the inclusion criteria. The total number of subjects who finally participated in the study was 183, of whom 97 subjects were in the exercise group and 86 in the comparison group. A total of 74 subjects of either group completed the program. From those, 70 participants of the exercise group and 71 of the comparison group attended the six-months follow-up, the others either refused to participate or could not be reached because of a change of address. At one-year follow-up, the number of completed questionnaires was 64 and 49, at the ten-years follow-up it was 58 and 60 in the exercise and the comparison group, respectively. Therapy dropouts were also requested to complete the six-months and the ten-years follow-up questionnaire. At 6-months follow-up, 16 exercise group dropouts and 4 comparison group dropouts returned the questionnaire. At 10-years follow-up 17 dropouts from the exercise group, and 9 from the comparison group completed the questionnaire. Figure 1 displays a flowchart of the study including number of participants and dropouts at each follow-up. The number of subjects finally included in statistical analysis in Tables 4 and 5 differs from the number of subjects displayed in the flowchart since subjects were excluded from statistical analysis if more than one observation of the respective variables was missing (see previous section “Statitical analysis”).
Fig. 1.
Flow diagram showing the number of participants and investigated therapy dropouts throughout the ten years follow up
Table 4.
Changes in functional outcome variables from pretreatment to six-months follow-up
| Global (n=104) | p (time effect) | Exercise group (n=59a) | Comparison group (n=45a) | p (interaction time × group) | |
|---|---|---|---|---|---|
| Index muscular endurance | 0.0001 | 0.002 | |||
| Pretreatment | 95±36 | 97±36 | 93±37 | ||
| Posttreatment | 120±41 | ||||
| 6-months follow-up | 111±39 | 120±35 | 99±42 | ||
| Index isokinetic strength | 0.006 | 0.01 | |||
| Pretreatment | 94±20 | 95±20 | 93±20 | ||
| Posttreatment | 100±20 | ||||
| 6-months follow-up | 97±19 | 99±18 | 93±18 | ||
| Aerobic capacity | 0.47 | 0.20 | |||
| Pretreatment | 100±14 | 101±13 | 97±14 | ||
| Posttreatment | 106±13 | ||||
| 6-months follow-up | 100±14 | 102±13 | 97±15 | ||
| Index lifting | 0.0001 | 0.31 | |||
| Pretreatment | 92±19 | 94±18 | 91±20 | ||
| Posttreatment | 104±21 | ||||
| 6-months follow-up | 100±22 | 102±24 | 97±18 | ||
| Range of motion | 0.01 | 0.33 | |||
| Pretreatment | 102±22 | 102±21 | 102±23 | ||
| Posttreatment | 104±22 | ||||
| 6-months follow-up | 106±21 | 107±21 | 105±22 |
Note: Values given are mean ± SD in % of values obtained from a healthy reference group
aExclusion from statistical analysis due to more than one missing observation accounts for the differing number of subjects compared to Fig. 1
Table 5.
Changes in self-rated pain, disability, and general well being from pretreatment to one-year follow-up
| Variable | Global (n=77) | P (time effect) | Exercise group (n=44a) | Comparison group (n=33a) | P (interaction time × group) |
|---|---|---|---|---|---|
| Pain drawingb | 0.001 | 0.02 | |||
| Pretreatment | 6±6 | 6±7 | 5±6 | ||
| Posttreatment | 4±5 | 3±3 | 5±6 | ||
| 6-months follow-up | 4±5 | 4±5 | 5±5 | ||
| 1-year follow-up | 3±5 | 3±3 | 5±6 | ||
| Current pain (NRS)c | 0.0001 | 0.50 | |||
| Pretreatment | 3±2 | 3±2 | 3±2 | ||
| Posttreatment | 2±2 | 1±2 | 2±2 | ||
| 6-months follow-up | 2±2 | 1±2 | 2±2 | ||
| 1-year follow-up | 1±2 | 1±1 | 1±2 | ||
| Pain (Mc Gill)d | 0.0001 | 0.92 | |||
| Pretreatment | 22±6 | 21±5 | 22±7 | ||
| Posttreatment | 18±4 | 17±3 | 20±4 | ||
| 6-months follow-up | 18±5 | 18±4 | 19±5 | ||
| 1-year follow-up | 18±4 | 17±3 | 18±4 | ||
| Disability (Waddell)e | 0.002 | 0.05 | |||
| Pretreatment | 38±9 | 39±10 | 36±7 | ||
| Posttreatment | 35±8 | 33±6 | 37±9 | ||
| 6-months follow-up | 33±6 | 32±6 | 34±5 | ||
| 1-year follow-up | 34±6 | 33±6 | 35±6 | ||
| Disability (Roland Morris)f | 0.005 | 0.07 | |||
| Pretreatment | 4±3 | 4±4 | 3±3 | ||
| Posttreatment | 2±2 | 2±2 | 3±3 | ||
| 6-months follow-up | 2±3 | 2±3 | 2±3 | ||
| 1-year follow-up | 3±3 | 2±3 | 3±3 | ||
| General well beingg | 0.53 | 0.61 | |||
| Pretreatment | 32±7 | 32±6 | 31±7 | ||
| Posttreatment | 33±5 | 34±5 | 33±6 | ||
| 6-months follow-up | 33±6 | 34±6 | 32±7 | ||
| 1-year follow-up | 32±6 | 33±5 | 31±6 |
aExclusion from statistical analysis due to more than one missing observation accounts for the differing number of subjects compared to Fig. 1
bScore 0–112
cScore 1–10 (no pain at all–strongest pain)
dScore 0–45
eScore 29–87
fScore 0–24
gScore 0–35
Note: Values given are mean ± SD
Comparison of groups for baseline characteristics
When the exercise group was compared with the comparison group for baseline characteristics, a slight but significant difference concerning the qualification was found (Table 3). The proportion of nurses was higher in the exercise than in the comparison group. Comparison between nurses and non-nurses for each group revealed that nurses of both groups were younger when compared to the non-nurses. In the comparison group nurses had a higher range of motion, whereas nurses of the exercise group indicated a higher pain score according the pain drawing. All other variables did not significantly differ in between the two groups. Comparison between the dropouts (n=35) and subjects who completed the entire program (n=148), revealed no difference among the groups, with exception of duration of LBP. The dropouts indicated shorter duration of LBP than the non-dropouts (mean, 8 and 12 years, respectively [p=0.004]). When the dropouts were analyzed with respect to changes in pain intensity (Numeric Rating Scale) within follow-up, we found no significant differences neither between baseline and six-months follow-up (mean, 2.7 and 2.8, respectively [p=0.62]) nor between baseline and ten-years follow-up (mean, 2.7 and 2.5, respectively [p=0.93]). Thus, without treatment there were no major changes in pain intensity.
Table 3.
Sociodemographic and physical characteristics at baseline (pretreatment) of the participants who completed the entire intervention program
| Exercise group n=74 | Comparison group n=74 | p | |
|---|---|---|---|
| Civil status | 0.21 | ||
| Single (%) | 60 | 52 | |
| Married (%) | 23 | 37 | |
| Divorced (%) | 16 | 11 | |
| Widowed (%) | 1 | ||
| Work status | 0.34 | ||
| Full time (%) | 54% | 64 | |
| >75% | 35% | 22 | |
| 50–75% | 10% | 14 | |
| <50% | 1% | ||
| Occupation | 0.03 | ||
| Nurses (%) | 76 | 60 | |
| Technical service (%) | 23 | 26 | |
| Administrative personnel (%) | 1 | 11 | |
| Physicians (%) | 3 | ||
| Age (years) | 38±8 | 39±10 | 0.84 |
| Weight (kg) | 66±11 | 69±13 | 0.15 |
| Height (cm) | 169±9 | 168±9 | 0.85 |
| LBP duration (years) | 11±7 | 13±10 | 0.11 |
| LBP within preceding 12 months | 0.44 | ||
| 8–30 days (%) | 19 | 25 | |
| >30 days (%) | 81 | 75 |
Note: Values are mean ± SD. The Mann Whitney test was used for ordinal data, Chi square test for nominal data, and the two sample t test for continuous data
Internal consistency of the indices
Cronbach’s alpha coefficients of the indices “Lifting”, “Isokinetic Strength”, and “Self-Assessed Treatment Effectiveness” ranged from 0.75 to 0.95 thus confirming the internal consistency. Since the index “Muscular Endurance” showed lower internal consistency (α=0.56), not only the index but also the single underlying items trunk flexion, arms holding, and squatting were included in subsequent analysis.
Reliability of outcome measures
Reliability of the functional outcome measures ranged from 0.62 to 0.84 (p<0.001, each) when considering pre- and posttreatment measurements. For the questionnaires, similar results were found with coefficients ranging from 0.59 to 0.83 (p<0.001) [35].
Treatment effects on functional capacity at six-months follow-up
Muscular endurance
The strongest treatment effect was found for isometric muscular endurance measurements (Table 4). All participants, irrespective of the group they were assigned to, showed an increase in muscular endurance from pretreatment to the six-months follow-up. However, the increase was significantly larger in the exercise than in the comparison group. Table 4 also contains the posttreatment outcome of the exercise group to provide evidence that an immediate training effect was present. It should be noted that there was only a slight decrease in endurance between posttreatment and six-months follow-up measurements, although subjects had been discharged from the training program.
Concerning the outcome of the single items trunk flexion, arms holding and squatting, the following results were obtained: Endurance time recorded in trunk flexion and squatting increased to a significantly larger extent in the exercise group than in the comparison group within follow-up (p=0.04, p=0.003, respectively). With respect to endurance time recorded during arms holding, we found a significant increase within follow-up for both groups as a whole (p=0.001), however there was no significant difference among groups in the extent of this increase.
Isokinetic strength
Treatment effects on isokinetic strength measurements were found between pretreatment and six-months follow-up when considering both groups as a whole, but also between groups (Table 4). Increase in strength was significantly larger in the exercise than in the comparison group.
Concerning all other functional measurements, such as the lifting capacity, aerobic capacity, and range of motion measurements, there was no significant difference between the outcome of the exercise and the comparison group. We just found a significant increase in lifting capacity and range of motion when analyzing changes within follow-up for both groups together.
Treatment effects on self-rated pain, disability, and general well being at one-year follow-up
Self-rated pain
Considering both groups together, a significant pain reduction was observed at one-year follow-up concerning pain intensity (NRS), pain quality (McGill) and quantitative pain drawing (Table 5). However, a significant difference in the extent of pain reduction between groups was only found for the quantitative pain drawing. Changes in pain intensity and pain quality were not significantly different between the groups.
Self-rated disability
Self-rated disability according to the Roland and Morris and the Waddell questionnaire showed a significant decrease from pretreatment to one-year follow-up for both groups as a whole. For the Waddell questionnaire it was further found, that the decline was significantly larger in the exercise than in the comparison group. Results from the Roland and Morris questionnaire showed the same tendency but differences were not significant between groups (Table 5).
General well being
Concerning the general well being score we found no significant changes within follow-up, neither for both groups as whole nor between groups (Table 5).
Treatment effects on self-rated pain and disability at ten-years follow-up
Self-rated pain intensity (NRS) and disability (Roland and Morris scale) first decreased between pretreatment and six-months follow-up and then again increased over the following ten-years. However changes were not found to be significant.
Self-assessed treatment effectiveness at ten-years follow-up
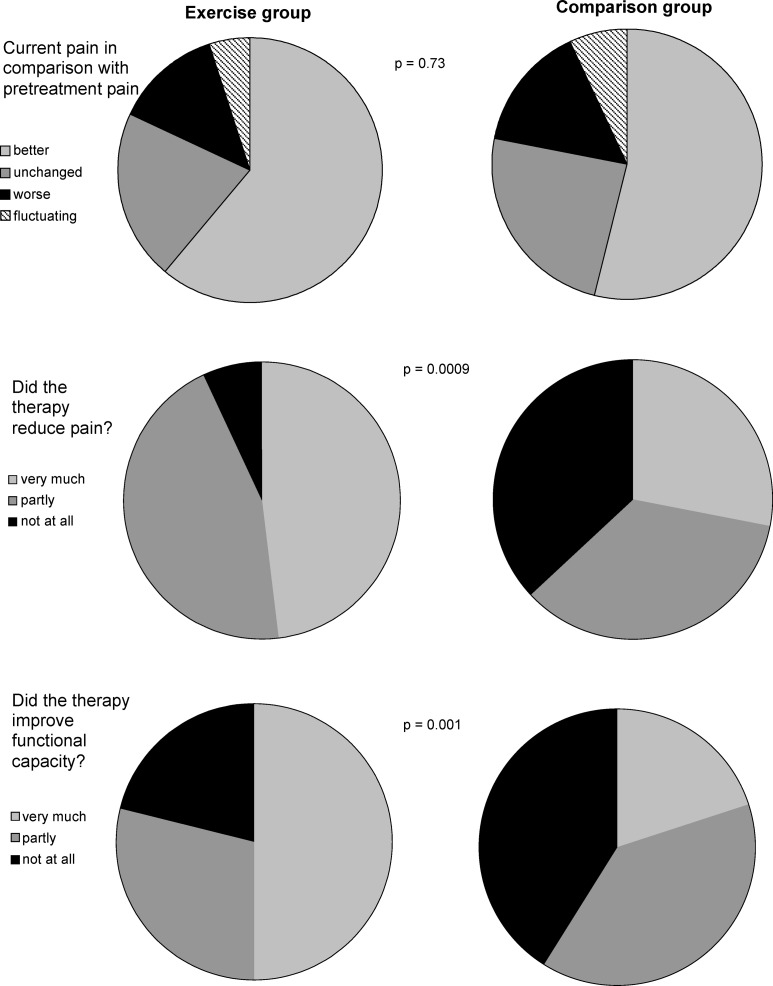
Figure 2 shows the evaluation of the treatment effectiveness at the ten-years follow-up. The majority of hospital employees (61 and 54% in the exercise and comparison group, respectively) indicated that they had less pain than they had before treatment, with no significant difference between groups. Concerning treatment effectiveness with respect to reduction of pain and improvement of functional capacity, the ratings of the exercise group were significantly higher than those of the comparison group. A total of 48% of the exercise group declared that the treatment had reduced their pain very much and 50% reported that their functional capacity had improved very much, whereas it were only 28 and 20% in the comparison group.
Fig. 2.
Self-assessed effectiveness of the treatment at ten-years follow-up. p values indicate the significance of the difference between the exercise group (n=58) and the comparison group (n=60)
Discussion
The current study shows that supervised physical training effectively improved functional capacity in terms of muscular endurance and isokinetic strength during a six-months follow-up. Furthermore, self-rated LBP and disability significantly decreased during a one-year follow-up [35]. Although during the ten-years follow-up self-rated LBP and disability nearly reached pretreatment level, the individual’s ratings concerning the effectiveness of treatment revealed that supervised physical training was more successful in reducing pain intensity and improving functional capacity than a back school intervention. Another study covering a five-year follow-up period also suggests a possible long-term benefit of a functional restoration program in terms of significantly fewer contacts with the health care system and fewer days of sick leave over the five-years follow-up period compared to a non-treated control group [3].
The main reason for offering a back school program within the scope of the current study was to provide at least some medical care for the comparison group. In order to maintain the subjects’ motivation to attend the subsequent follow-ups, the comparison group was only requested to complete the questionnaires at discharge from the program. Otherwise it was expected that the physical strenuousness of the functional tests would have possibly kept participants from attending further follow-ups. In fact, participation rates at six-months follow-up were high in both, the exercise and the comparison group (95 and 96%, respectively). Considering all follow-ups, participation ranged from 66 to 96% among those having completed the program. Among the dropouts, i.e. subjects who did not complete the program, a considerable proportion returned the six-months (57) and the ten-years follow-up questionnaires (74). When the self-rated pain intensities (Numeric Rating Scale) recorded at six-months and ten-years follow-up were compared to those recorded at baseline, no significant changes were found, neither between baseline and six-months follow-up, nor between baseline and ten-years follow-up. Thus, it may be assumed that changes in pain intensity, as they have been observed among non–dropouts, can be attributed to the intervention and not to artifacts. Although selection effects cannot be completely excluded, the results suggest that at least the dropouts do not cause biased results.
Comparability of groups was only limited by differences in the subjects’ occupation. The proportion of nurses was higher in the exercise group. When the nurses were compared to the non-nurses for baseline data of each group, we only found a significant difference in age, range of motion, and pain extension according to the quantitative pain drawing. However, since differences between groups concerned only few variables, subsequent analysis considered nurses and non-nurses as a whole in each group.
Changes in aerobic capacity, range of motion, and lifting capacity revealed not to be associated with treatment. One reason for the lack of improvement in the lifting tests probably is that lifting was not included in the exercise concept. From subsequent experience with Work Hardening we know that lifting capacity improves when lifting is exercised within the scope of the program. This was also described by Mayer et al. [30]. In conclusion, it seems to be important that lifting or other functional and work oriented exercises are included in a training program in order to meet physical demands of work [17, 28, 32].
Concerning the evaluation of the treatment effects, it should be noted that some participants complained about the isokinetic strength measurements. This could be due to the unfamiliar situation of the testing procedure, which forced the subjects to move at a given velocity, thus inhibiting the performance of self-determined movements. Conversely, the treatment itself, supervised physical training and the back school, did not cause any adverse effects.
In the current study a strong treatment effect was found for isometric muscular endurance measurements, which can be mainly attributed to the focus of the exercise program. Between pre- and posttreatment there was a high increase of muscular endurance. The related effect size was found to be 0.63 for the exercise group, whereas it was only 0.16 for the comparison group. The benefit of intensive exercises has been described earlier [19]. We found that even 6 months after discharge from the program, muscular endurance was still significantly increased. This finding deserves particular attention. It is hypothesized that once the muscle system has been trained and has improved its strength and neuromuscular patterns, improvement can last due to the continuation of physical demands during work and leisure time. Due to financial restrictions functional tests could not be repeated at ten-years follow-up. Thus, the long-term treatment effect was just analyzed by means of a shortened questionnaire. Though it has been reported that after active low back training, improved muscular endurance tended to diminish at the one-year follow-up [18], our results indicate that some long-term effect might be present. At the ten-years follow-up a large proportion of subjects ascribed reduction in pain intensity and increase in functional capacity to the treatment they had received ten years ago. Furthermore, the subjects’ ratings concerning pain reduction and functional capacity improvement were significantly higher in the exercise group than in the comparison group thus documenting a long-term effect of strengthening exercises. This might be at least partially due to a better muscular support and stability of the low back. In addition, the adaptation of cognitive pain coping strategies [40] and alterations in the subjects’ perception of disability [27] might play an important role, especially when considering the discrepancy between the subject’s self-rated pain intensity and disability, which was similar in both groups, and the self-assessed treatment effectiveness, which was much better in the intervention group. Finally, the development of some kind of safety concern regarding strenuous physical demands, such as lifting of heavy weights, might have contributed to the long-term effect observed in the current study. The effectiveness of an integrated approach promoting self control and behavior change through educational measures has been shown ealier [20].
Concerning changes in self-rated disability and pain intensity we found a significant improvement from pretreatment to the one-year follow-up with subsequent diminution over the following ten years in both groups. Changes were not significantly associated with treatment and subjects of both groups ended up at a similar pain level. However, in the exercise group, the Roland and Morris disability score at ten-years follow-up was still beyond that of the beginning. Moreover, the subjects’ self-assessed treatment effectiveness in terms of disability and pain reduction indicate that subjects still had less pain and felt less disabled, or had better strategies to cope with the pain even ten years after treatment. Another study found that a reduction in the subjects’ self-rated disability was the most important predictor of success in the treatment of chronic LBP, when considering pain intensity, back-to-work, and subjective rating of success [14]. The modification of beliefs appeared to be more important for the rehabilitation of LBP patients than actual changes in the objective physical status. However, it should be pointed out that the latter study only included patients incapacitated for work. Though our data indicate similar results, comparison might be limited. It may be assumed that patients incapacitated for work show different beliefs concerning physical capacity and pain intensity than subjects capable for work. In this context psychological parameters may play a more important role for the effectiveness of treatment than they probably do for subjects capable for work. Moreover, we found that the general well being index did not significantly change over the study period thus indicating a stable condition of the subjects under investigation.
Concerning the effectiveness of a back school program, it has been found that it can be successful in improving functional capacity, self-rated disability [15], and reducing the recurrence and severity of new LBP episodes among chronic LBP patients within short [24] and long-term follow-up [11]. Although in the current study, the back school group also experienced improvement of complaints to some extent, the effects diminished shortly after treatment. Furthermore, in comparison with the exercise group, it clearly appeared that an exercise program using strengthening devices was superior to a back school program in terms of functional outcome, self-rated pain intensity, and disability among subjects with chronic LBP. A comprehensive review [38] revealed similar results, stating that in chronic LBP patients (>12 weeks LBP) exercise therapy was superior to usual care offered by a general practitioner and giving some evidence that exercise therapy may be also superior to a back school program. This is supported by another study, which found that the exercise group improved significantly more in terms of functional (Oswestry questionnaire) and pain status (Visual Analog Scale) than the back school group did [10]. After six months and after two years, differences concerning the functional status still were significant. The authors suggested that patients might have become more active due to the intervention thus contributing to a long-term effect. This might be also true for the current study. In fact, at six-months follow-up, the proportion of subjects indicating regular strengthening exercises was slightly, but not significantly, higher in the exercise group than in the comparison group. Moreover, six-months follow-up data of the comparison group show that the proportion of subjects indicating no physical activity in leisure time had decreased when compared to pretreatment. It may be assumed that subjects of the exercise group reported about the benefit of exercises thus encouraging the comparison group to become more physically active. In phone interviews at ten-years follow-up, it became evident that subjects of both groups appreciated to have training facilities within the occupational setting.
The current study has some limitations since functional capacity has not been assessed at one-year and ten-years follow-up. Hence, no objective data are available to describe the long-term benefit of supervised physical training. Since recall bias was expected to be present at ten-years follow-up, only shortened questionnaires were used. Consequently, the current study can only provide some evidence about a probable long-term effect of supervised physical training using strengthening devices.
Conclusions
The current study revealed that supervised physical training applying strengthening exercises effectively improved objective functional outcome parameters and subjective self-rated disability and pain scores during short-term follow-up. The subjects’ positive evaluation of the treatment effect after ten years, further suggests a long-term benefit of the treatment. Therefore it is recommended that these programs should be promoted within occupational settings. Future studies should address the long-term effect of strengthening exercises with respect to effects on functional capacity.
Appendix: Detailed description of tests performed
Lifting capacity
Subjects were instructed to perform a lower and a upper lifting test (modified version of the validated PILE test [29]). The lower lifting test meant to lift the initial weight in a box (height 28 cm, width and depth each 33 cm) from floor to waist (75 cm) and back to floor at a sequence of four lifting cycles within 20 s. Afterwards weight was increased until the subject was not able any more to complete four lifting cycles within 20 s. The upper lifting test was done similarly applying lifting cycles from waist to shoulder (135 cm) to waist. The test was terminated when one of the following end-points was achieved: fatigue or voluntary test termination, maximum heart rate higher than 190 minus age, and if the weight lifted exceeded 50% of the subject’s body weight. For women the initial weight was 4 kg (crate 1.5 kg, first increment 2.5 kg), increasing at 2.5 kg intervals, for men it was 6.5 kg, increasing at 5 kg intervals.
Isokinetic trunk strength
Subjects were standing in the device (Cybex TEF Modular Component isokinetic dynamometer from Lumex Inc., Ronkonkoma, NY. [33]), fixed at the sacrum and the thoracolumbar junction. They had to perform flexion and extension movements against resistance at three different angle velocities (60°, 120° and 150° per s) after standardized instructions. In order to get used to the test, a first trial with submaximal effort was performed. Data were recorded only during the following test session.
Range of motion
Anatomical reference points at L5/S1 and Th12/L1 were defined by palpation in upright position, and were marked for further measurements. After a warming up of three flexion/extension and side bending movements, the position of the reference points was recorded with the subject standing in neutral position. Then flexion and extension movements were performed after standard instructions and the inclinometer (EDI, Cybex, Lumex Inc.). was put on the reference points to register the position. Differences between reference points in neutral and in maximally flexed respectively extended position were added up to obtain the subject’s flexion and extension range of motion.
Isometric muscular endurance
Muscular endurance in trunk extension using the modified version of the Soerensen test [4]: The subject lay prone on a 8 cm thick pad with the lower legs fixed to the pad, and arms abducted, fingers positioned behind the ears. The trunk had to be lifted and an unsupported horizontal position to be maintained up to a maximum time of 120 s. Endurance time (s) was recorded until the subject could no longer maintain the horizontal position. More than half of all subjects (53%) reached > 100% of the set time limit (120 s) thus artificially reducing the outcome of the test. Consequently results of this test have been disregarded.
Muscular endurance in trunk flexion: The subject was in supine position, the pelvis and the lumbar spine 10 cm beyond the iliac crest positioned on a hard, 8 cm thick foam cushion, and the lower legs placed on a box thus forming a 90° angle with the thighs. Arms were folded in front of the chest. Subjects had to curl up just a few centimeters and maintain this position with unsupported upper back until a maximum of 120 s was reached. Endurance time was recorded in seconds.
Muscular endurance of the upper arm and shoulder girdle muscles The maximum time subjects were able to hold weights of six pounds in each hand with the upper arms horizontal and the forearms angled at 90°, was recorded. The test was stopped when 180 s were reached.
Muscular endurance measurements were also performed in squatting position in 90° flexion of the hips and knees. Endurance time was recorded until the limit of 120 s was reached.
During all measurements subjects were encouraged to maintain the position as long as possible.
Acknowledgements
The authors acknowledge that the first part of the study (six-months follow-up period) was mainly developed and guided by M. Oliveri, and has been documented in a comprehensive report for the Swiss National Science Foundation and in an article for Eular [35]. The study was approved by the local Ethics Committee.
Footnotes
Supported in part by a grant of the Swiss National Science Foundation (Project NFP 26, No. 4026-27064) and by the BBW (Project “SOS-LBD”, No. 97.0046).
References
- 1.Antonovsky A. Unraveling the mystery of health. How people manage stress and stay well. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 2.Bendix AE, Bendix T, Ostenfeld S, Busch E, Andersen A. Active treatment programs for patients with chronic low back pain: a prospective, randomized, observer-blinded study. Eur Spine J. 1995;4:148–152. doi: 10.1007/BF00298239. [DOI] [PubMed] [Google Scholar]
- 3.Bendix AE, Bendix T, Heatrup C, Busch E. A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients. Eur Spine J. 1998;7:111–119. doi: 10.1007/s005860050040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biering-Soerensen F. Physical measurement as risk indicators for low-back trouble over a one-year period. Spine. 1984;9:106–119. doi: 10.1097/00007632-198403000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Bigos S, Bowyer O, Braen G, et al. Acute low back problems in adults. Clinical practice guideline No. 14. AHCPR Publication No. 95-0642. Rockville: Public Health Service; 1995. [Google Scholar]
- 6.Capra P, Mayer T, Gatchel R. Adding psychological scales to your back pain assessment. J Musculoskel Med. 1985;2:41–52. [Google Scholar]
- 7.Cronbach LJ. Essentials of psychological testing. New York: Harper and Row; 1970. [Google Scholar]
- 8.Downie WW, Leatham PA, Rhind VM, et al. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–381. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DuPuy HJ, Ulin PR, Bullinger M, et al. PGWB psychological general well-being index. In: Westhoff G, et al., editors. Handbuch psychosozialer Messinstrumente. Göttingen: Hogrefe; 1993. pp. 642–646. [Google Scholar]
- 10.Frost H, Lamb SE, Klaber Moffett JA, et al. A fitness programme for patients with chronic low back pain: 2-year follow-up of a randomised controlled trial. Pain. 1998;75:273–279. doi: 10.1016/S0304-3959(98)00005-0. [DOI] [PubMed] [Google Scholar]
- 11.Glomsrod B, Lonn JH, Soukup MG, et al. “Active back school”, prophylactic management for low back pain: three-year follow-up of a randomized, controlled trial. J Rehabil Med. 2001;33:26–30. doi: 10.1080/165019701300006506. [DOI] [PubMed] [Google Scholar]
- 12.Gunnari H, Evjenth O, Brady MM. Sequence exercise. The sensible approach to all-round fitness. Oslo: Dreyers; 1984. [Google Scholar]
- 13.Hansen FR, Bendix T, Skov P, et al. Intensive, dynamic back muscle exercises, conventional physiotherapy, or placebo-control treatment of low-back pain. A randomized, observer-blind trial. Spine. 1993;18:98–108. doi: 10.1097/00007632-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Hildebrandt J, Pfingsten M, Saur P, et al. Prediction of success from a multidisciplinary treatment program for chronic low back pain. Spine. 1997;22:990–1001. doi: 10.1097/00007632-199705010-00011. [DOI] [PubMed] [Google Scholar]
- 15.Hodselmans AP, Jaegers SM, Goeken LN. Short-term outcomes of a back school program for chronic low back pain. Arch Phys Med Rehabil. 2001;82:1099–1105. doi: 10.1053/apmr.2001.23899. [DOI] [PubMed] [Google Scholar]
- 16.Holten O. Medical exercise therapy- the basic principles. Fysioterapeuten. 1991;58:27–32. [Google Scholar]
- 17.Isernhagen SJ. Functional capacity evaluation and work hardening perspectives. In: Mayer TG, Mooney V, Gatchel RJ, editors. Contemporary conservative care for painful spinal disorders. Philadelphia: Lea & Febiger; 1991. pp. 328–345. [Google Scholar]
- 18.Kankaanpää M, Taimela S, Airaksinen O, et al. The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability. Spine. 1999;24:1034–1042. doi: 10.1097/00007632-199905150-00019. [DOI] [PubMed] [Google Scholar]
- 19.Kannus P, Jozsa L, Renström P, et al. The effects of training, immobilization, and remobilization on musculoskeletal tissue. Scand J Rehab Med. 1992;2:100–118. [Google Scholar]
- 20.Keel PJ, Wittig R, Deutschmann R, et al. Effectiveness of in-patient rehabilitation for sub-chronic and chronic low back pain by an integrative group treatment program (Swiss Multicentre Study) Scand J Rehab Med. 1998;30:211–219. doi: 10.1080/003655098443959. [DOI] [PubMed] [Google Scholar]
- 21.Keeley J, Mayer TG, Cox R, et al. Quantification of lumbar function Part 5: reliability of range-of-motion measures in the sagittal plane and an in vivo torso rotation measurement technique. Spine. 1986;11:31–35. [PubMed] [Google Scholar]
- 22.Kuorinka I, Jonsson B, Kilbom A, et al. Standardised nordic questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 23.Läubli T, Thomas C, Hinnen U, et al. Erfassung muskuloskeletaler Beschwerden mittels Fragebogen. Sozial- und Präventivmedizin. 1991;36:25–33. doi: 10.1007/BF01322297. [DOI] [PubMed] [Google Scholar]
- 24.Lonn JH, Glomsrod B, Soukup MG, et al. Active back school: prophylactic management for low back pain. A randomized, controlled, 1-year follow-up study. Spine. 1999;1:865–871. doi: 10.1097/00007632-199905010-00006. [DOI] [PubMed] [Google Scholar]
- 25.Malmivaara A, Hakkinen U, Aro T, et al. The treatment of acute low back pain–bed rest, exercises, or ordinary activity? N Engl J Med. 1995;332:351–355. doi: 10.1056/NEJM199502093320602. [DOI] [PubMed] [Google Scholar]
- 26.Manniche C. Clinical benefit of intensive dynamic exercises for low back pain. Scand J Med Sci Sports. 1996;6:82–87. doi: 10.1111/j.1600-0838.1996.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 27.Mannion AF, Müntener M, Taimela S, et al. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24:2435–2448. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- 28.Matheson LN. Work hardening for patients with back pain. J Musculoskel Med. 1993;10:53–63. [Google Scholar]
- 29.Mayer TG, Barnes D, Nichols G, et al. Progressive isoinertial lifting evaluation I. A standardized protocol and normative database. Spine. 1988;13:993–997. doi: 10.1097/00007632-198809000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Mayer TG, Gatchel RJ, Kishino H, et al. Objective assessment of spine function following industrial injury. A prospective study with comparison group and one-year follow-up. Spine. 1985;10:482–493. doi: 10.1097/00007632-198507000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Mayer TG, Gatchel RJ, Mayer H, et al. A prospective two-year study of functional restoration in industrial low back injury. An objective assessment procedure. JMA. 1987;258:1763–1767. doi: 10.1001/jama.258.13.1763. [DOI] [PubMed] [Google Scholar]
- 32.Mayer TG, Gatchel RJ. Functional restoration for spinal disorders: the sports medicine approach. Philadelphia: Lea & Felbiger; 1988. [Google Scholar]
- 33.Mayer TG, Smith SS, Keeley J, et al. Quantification of lumbar function. Part 2: Sagittal plane trunk strength in chronic low-back pain patients. Spine. 1985;10:765–772. [PubMed] [Google Scholar]
- 34.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 35.Oliveri M, Kopp HG, Läubli T, et al. Die Bedeutung von körperlicher Aktivität und physischer Leistungsfähigkeit für die Prävention und Behandlung chronischer Rückenbeschwerden. In: Keel P, Perini Ch, Schütz-Petitjean D, et al., editors. Chronifizierung von Rückenschmerzen: Hintergründe, Auswege. Basel: Eular; 1996. pp. 52–69. [Google Scholar]
- 36.Pollock ML, Wilmore JH, Fox SM. Exercise in health and disease. Evaluation and prescription for prevention and rehabilitation. Philadelphia: Saunders; 1984. [Google Scholar]
- 37.Roland M, Morris R. A study of the natural history of back pain. Part I. Development of a reliable and sensitive measure of disability in low back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Tulder M, Malmivaara A, Esmail R, et al. Exercise therapy for low back pain. A systematic review within the framework of the Cochrane collaboration back review group. Spine. 2000;25:2784–2796. doi: 10.1097/00007632-200011010-00011. [DOI] [PubMed] [Google Scholar]
- 39.Waddell G. Clinical assessment of lumbar impairment. Clin Orthop. 1987;221:110–120. [PubMed] [Google Scholar]
- 40.Waddell G. A new clinical model for the treatment of low back pain. Spine. 1987;12:632–644. doi: 10.1097/00007632-198709000-00002. [DOI] [PubMed] [Google Scholar]