Abstract
Background:
Medial proximal tibial angle (MPTA) is the commonly used angle, which is simply measured from the knee radiographs. It can determine the correction angle in medial opening wedge high tibial osteotomy (MOWHTO). The hypothesis of our study is that post-osteotomy MPTA can predict the change in correction angle, and we aimed to determine the optimal MPTA with which to prevent recurrent varus deformity after MOWHTO.
Materials and Methods:
Between January 2002 and April 2010, radiographs of 59 patients, who underwent 71 MOWHTOs using the locking-compression osteotomy plates without bone grafts, were evaluated for the change of the MPTA. The MPTA was measured preoperatively and one and twelve months postoperatively. The changes of MPTA between one and twelve months were classified into valgus, stable, and varus change. The predicting factors were analyzed using analysis of variance (ANOVA) and Bonferroni multiple comparisons. The receiver operating characteristic (ROC) curve was used to find out the cut off point for preventing the recurrent varus deformity.
Results:
The overall preoperative, and one and twelve month postoperative MPTA values were 84.4 ± 2.4°, 97.2 ± 4.1°, and 96.3 ± 3.6°, respectively. Between one and twelve months, 39 knees displayed reduced varus change (–2.8 ± 2.1°), 18 knees displayed no change, and 14 knees displayed a greater valgus change (+2.9 ± 2.1°). The best factor for predicting these changes was the one month MPTA value (P = 0.006). By using the ROC curve, a one month MPTA of 95° was analyzed as the cut off point for preventing the recurrent varus deformity. With MPTA ≥95°, 92.3% of the osteotomies exhibited stable or varus change and 7.7% exhibited valgus change. However, with MPTA <95°, 47.4% exhibited stable or varus change and 52.6% exhibited valgus change (P < 0.001, odds ratio = 13.3).
Conclusion:
The postoperative MPTA can be used to predict the change in correction angle and an MPTA of at least 95° is the crucial angle with which to prevent recurrent varus deformity.
Keywords: High tibial osteotomy, loss of correction, medial proximal tibial angle, recurrent varus
INTRODUCTION
Medial opening wedge high tibial osteotomy (MOWHTO) is an effective treatment for medial compartmental osteoarthritic knee.1–3 The principle of this procedure is to shift the weight bearing load from the arthritic portion to the viable articular cartilage portion. Thus, the mechanical axis should be corrected and passed through the lateral compartment. The pain improvement and the long term outcome of this operation depend on the accuracy of correction and correction angle after the osteotomy has united.3,4 Several methods for determining the proper overcorrection have been proposed.5–8
The causes of failure after high tibial valgus osteotomy include inadequate preoperative planning, inaccurate correction during surgery, and a loss of correction.5,7,9,10 Undercorrection is one of the common complications after osteotomy and can lead to recurrent varus deformity, the progression of medial joint arthritis, and patient dissatisfaction.3,11,12
In the context of deformity correction, medial proximal tibial angle (MPTA) is the frequently referenced angle. It is measured using simple methods from the knee radiographs, with the normal value of 87° (range 85°–90°).8 This angle can represent the correction angle for use in the osteotomy and is usually seen during the operation under fluoroscopic control. Importantly, the MPTA can be used to detect the correction angle change and recurrent varus deformity during the followup period. Thus, the hypothesis of our study is that postoperative MPTA can be used to predict the change in correction angle. We aimed to determine the optimal MPTA to prevent recurrent varus deformity after MOWHTO.
MATERIALS AND METHODS
Between January 2002 and April 2010, 81 knees (68 patients) with primary medial osteoarthritis were treated with MOWHTOs at our institute. The preoperative exclusion criteria were symptomatic osteoarthritis in the lateral or patellofemoral compartments assessed by clinical examination with correlated radiographic findings, osteoporosis defined as T-score of bone mineral density <–2.5, varus deformity >15°, flexion contracture >10°, range of motion <90°, and the presence of severe osteoarthritis (defined as a grade of 4 on the Kellgren–Lawrence radiographic grading scale).13 Furthermore, the patients who had previous complex knee surgery, nonunited osteotomy, and no radiographs following our criteria were also excluded from this study. Finally, two nonunited osteotomies (2 patients) assessed by using Apley and Solomon's criteria14 and eight osteotomies (7 patients) that did not meet our radiographic criteria were excluded. Therefore, 71 knees from 59 patients were available for evaluation in our study. This study was approved by the Ethics Committee of Siriraj Hospital.
All osteotomies were performed by the principal investigator (KC). Preoperative planning and postoperative analysis were based on the digitalized standing hip-to-ankle radiographs. The weightbearing line was planned and calculated to pass Fujisawa's point.6 The oblique incision was started just distal to the medial joint line and ended at the tibial tubercle level. The superficial medial collateral ligament was subperiosteally released from proximal tibia, and the complete release was confirmed by valgus stress test under fluoroscopic examination. A Kirschner wire was inserted in the oblique direction from the metaphysio-diaphyseal junction of the medial proximal tibial cortex, which corresponded to just above the upper border of pes anserinus and was directed toward the lateral proximal tibial cortex at the level of the tip of the fibular head. The osteotomy was performed beneath the wire using an osteotome and oscillating saw. An ascending cut was made behind the tibial tuberosity in the anterior fourth of the tibial tuberosity, leaving the patellar ligament attached to the distal tibial fragment. The osteotomy ended 5 mm medial to the lateral cortex. The osteotomy was opened gradually using two flat chisels, and the gap was maintained with a spreader. The intraoperative mechanical axis was controlled using the cable method.15 Internal fixation was performed using fixed angle plates (Tomofix or Locking Compression Plate, Synthes, Switzerland) without bone grafts or bone substitutes. A number 10 gauge drain was placed over the plate. After wound closure, a compressive Robert Jones bandage was applied.
The isometric quadriceps exercise, active ankle pumping, and straight leg raising were started on the first postoperative day. The drain and compressive dressing were removed on the second day after surgery. The patient was allowed to move the knee as tolerated and walk using toe touch weight bearing for 2 weeks followed by partial weight bearing for the next 2 weeks. Full weight bearing was permitted at 4 weeks after the operation. All patients were followed up at 1, 2, 3, 6, 9, and 12 months.
The femorotibial angle (FTA) and MPTA were measured preoperatively and 1 and 12 months postoperatively using the picture archiving and communication system (PACS). FTA was the angle formed by the mechanical axis of the femur (from the center of the femoral head to the top of the femoral notch) and tibia (from the center of the ankle to the center of the tibial spines) [Figure 1]. MPTA was the medial angle between two lines: one line of the tibial anatomical axis and a second line extending from the medial to the lateral most area of the tibial plateau, while excluding the osteophyte at the tibial plateau surface [Figure 1]. Recurrent varus deformity was defined as less than 90° MPTA at the 1 year followup.
Figure 1.
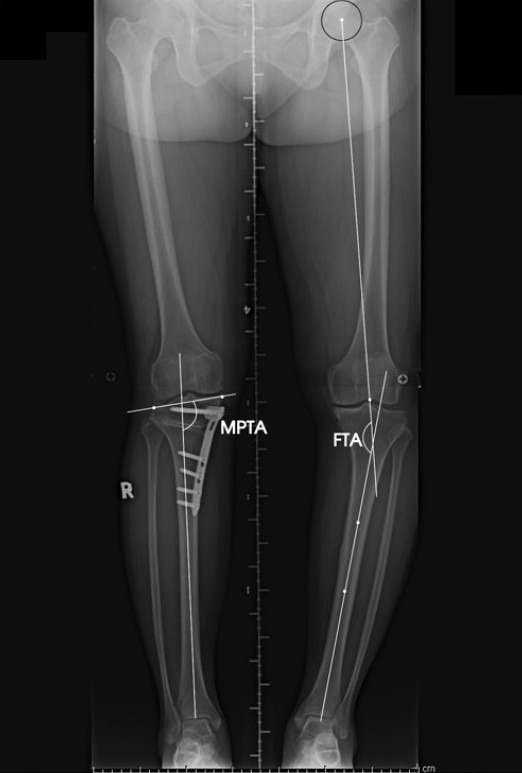
The radiograph demonstrates the measurement of medial proximal tibial angle and femorotibial angle
From our previous study, 10 radiographs after MOWHTOs obtained in neutral, 15° external rotation and 15° internal rotation views of the knees were assessed. In the internal rotation view, the patellar center moved to the medial two-fifths of the distal femur and MPTA increased 4.7 ± 1.2°. However, MPTA decreased 6.5 ± 1.0°, and the patella was positioned at the lateral two fifths when the legs were externally rotated. Therefore, the rotation of lower limb had a major effect on the MPTA measurement. We selected the anteroposterior views of the standing long films, which had the patellae (middle one-fifth) centered over the femoral condyles as our radiographic criteria. However, at the 12 month followup, 14 osteotomies yielded only standing short films. The short films could not be used to measure the FTA or identify the precise tibial anatomical axis for MPTA measurement. To avoid less sample size, we studied 20 standing hip to ankle radiographs after MOWHTOs. Each film was cropped and used to create 30 cm (standard length of short knee radiographs) short films of the knees with two different proximal tibia lengths: 10 and 15 cm [Figure 2]. MPTA was measured by two blinded orthopedists. The deviation of MPTA was 0.5° (range 0°–1°) and 2.0° (range 0°–3°) in 15 and 10 cm proximal tibial length films, respectively, when compared to the gold standard long film. Therefore, the additional criterion for short knee radiograph selection was a proximal tibial length of at least 15 cm, as revealed by the film. Based on these two criteria, four long films with rotational error and four short films with inadequate proximal tibial length were excluded from our study as mentioned above.
Figure 2.
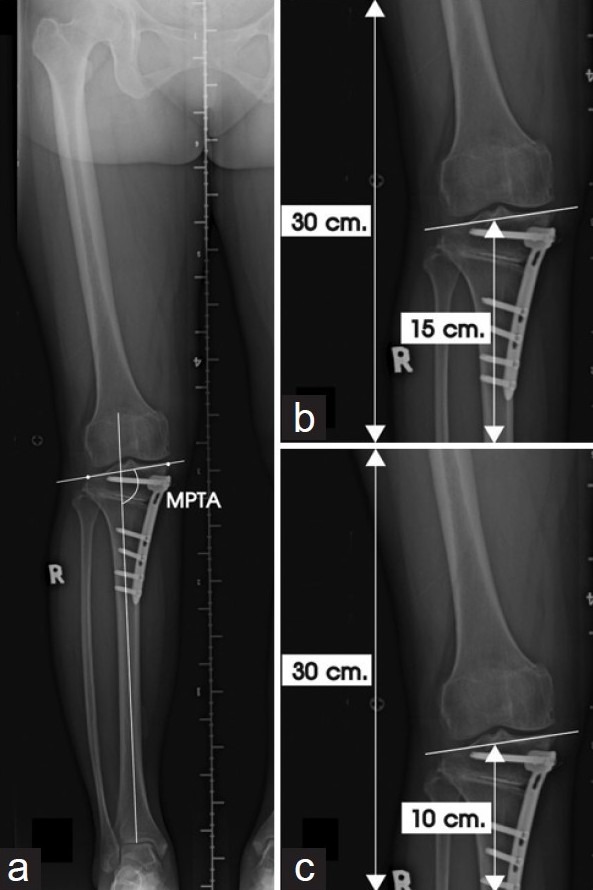
Anteroposterior view of standing hip-to-ankle radiograph with medial proximal tibial angle (MPTA) measurement (a) and cropped 30-cm length radiographs with two different proximal tibia lengths: 15 cm (b) and 10 cm (c)
The data were analyzed using the commercially available SPSS statistics software, version 13.0. Quantitative data were presented as the mean. The MPTA changes between 1 and 12 months were classified into three groups. The varus group consisted of the knees with evidence of decreased MPTA on subsequent X-rays, whereas stable group had unchanged MPTA and valgus group had increased MPTA. Differences in one month MPTA values among the three groups were analyzed using analysis of variance (ANOVA) and the Bonferroni multiple comparison. The receiver operating characteristic (ROC) curve was used to determine the cut off postoperative MPTA value that was best able to prevent recurrent varus deformity. P values less than 0.05 were regarded as statistically significant. The intra and interobserver reproducibility of MPTA measurement was assessed and expressed as the intraclass correlation coefficients (ICCs), which varied from zero (no agreement at all) to 1 (total agreement).
RESULTS
Seventy one MOWHTOs were carried out on a total of 59 patients. There were 55 females and 4 males, with a mean age of 54.4±4.9 years (range 40–67 years) and a mean body mass index of 28.6±4.0 kg/m2. The mean preoperative range of motion was 118.9±16.5°. Thirty one (43.7%) and 40 (56.3%) knees, respectively, were classified as grade II and III by the Kellgren-Lawrence radiographic grading scale. The overall mean FTA was 169.5±3.0° preoperatively; at 1-month postoperatively, this value was 183.3±4.0°. The mean correction angle in our series was 13.9±4.6°. The overall preoperative, and one and twelve month postoperative MPTA values were 83.4±3.0°, 97.2±4.1°, and 96.3±3.6°, respectively. The overall loss of correction angle was 1.0±2.9°. One patient (1.4%) had displayed recurrent varus deformity at the one year followup. However, no patients required conversion to total knee arthroplasty at the last followup time. In subgroup analysis, the MPTA changes between 1 and 12 months were classified into three groups: 18 knees (25.4%) were in the stable group, 39 knees (54.9%) were in varus group (a decreasing MPTA angle of –2.8±2.1°) and 14 knees (19.7%) were in valgus group (an increasing MPTA angle of +2.9±2.1°) [Table 1]. The comparison of the changes in MPTA among three groups is shown in Figure 3.
Table 1.
Subgroup analysis of radiographic outcomes
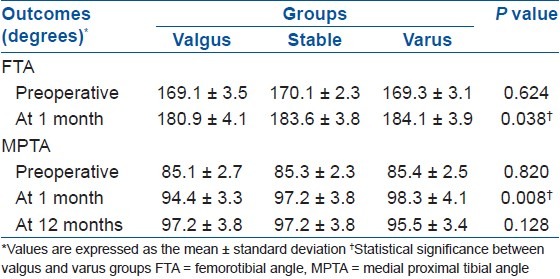
Figure 3.
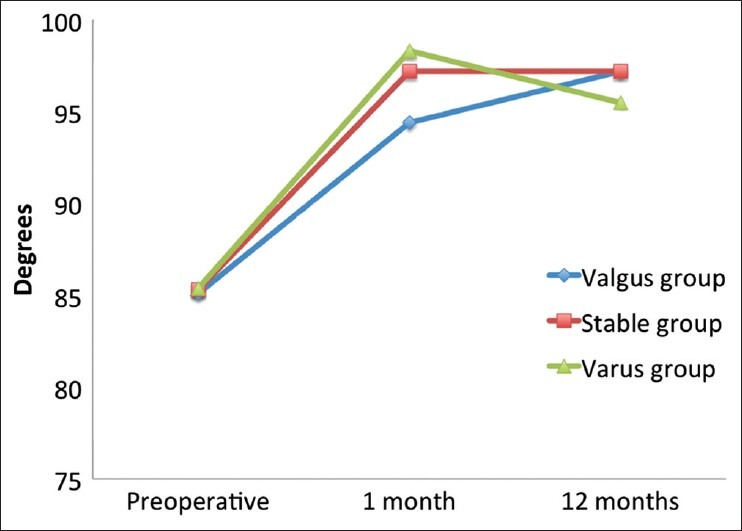
The diagram displays the comparison of the changes in medial proximal tibial angle among three groups
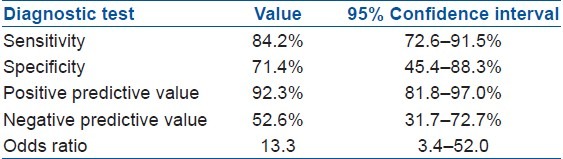
ANOVA revealed no significant difference in terms of patients’ characteristic data among the three groups. Nevertheless, the postoperative one month FTA and MPTA values were the two radiographic parameters that varied significantly among these subgroups [Table 1]. In further analysis with Bonferroni multiple comparisons, this significant difference was shown only between the varus and valgus groups (P = 0.034 and P = 0.006 for postoperative one month FTA and MPTA, respectively). With a more significant P-value, the one month postoperative MPTA was the best predictor of the MPTA change at 12 months after the operation. The cut off point for one month postoperative MPTA was analyzed using an ROC curve. The 95° of MPTA was indicated to predict the MPTA change as follows: with one month MPTA ≥95°, 48 knees (92.3%) had stable or varus collapse and 4 knees (7.7%) had valgus collapse at 1 year. In contrast, with 1-month MTPA <95°, 9 knees (47.4%) displayed stable or varus collapse and 10 knees (52.6%) displayed valgus collapse (P < 0.001, odds ratio = 13.3). The diagnostic test from the MTPA >95° is summarized in Table 2. Furthermore, because the maximal degree of varus collapse in this study was 4°, no patient had recurrent varus deformity when we corrected the MPTA to at least 95°.
Table 2.
The diagnostic test from the medial proximal tibial angle (MPTA) >95°
The excellent inter observer reliability was demonstrated for MPTA measurement in standing long films (ICC = 0.95), 15 cm (ICC = 0.95) and 10cm proximal tibial length film (ICC = 0.92), and 0.98 of ICC was expressed in all length films for the intra observer reproducibility.
DISCUSSION
Accurate correction in high tibial osteotomy and maintenance of corrected limb alignment until osteotomy healing are very important. The precision of correction can be achieved by sufficient preoperative planning and meticulous surgical technique. However, a loss of correction may still occur peri or postoperatively.9,10,16 In this study, the MPTA that directly referenced the correction angle after MOWHTO was used to determine the future collapse of the osteotomies. With postoperative MPTA ≥95°, most osteotomies (92.3%) could maintain or collapse into a more varus position with a maximal degree of 4°. The tethering effect of medial soft tissue structures might explain this phenomenon. However, with MPTA <95°, the results with respect to MPTA change at 1year followup were unpredictable (47.4% had stable or varus change and 52.6% had valgus change). Although the number of cases seemed to be small, only 62 knees were required to predict 80±10% of MTPA change with 95% confidence interval (2-sided). Thus, 71 knees of this study were sufficient for analysis. Additionally, the change in MPTA was not correlated with age, gender, and body mass index.
The definition of recurrent varus deformity in our series was set as less than 90° MPTA at the 1 year followup because theses angles would make the weight bearing load fall on the medial compartment, which led to the failure of high tibial osteotomy.3,11,12 From our results, the recurrent varus deformity was revealed in one patient who had 92° of 1-month MPTA and 86° of 12-month MPTA; nevertheless, no patient required conversion to total knee arthroplasty at the minimum 1-year followup. In addition, the most important thing was that if postoperative MPTA of at least 95° was made, no recurrent varus deformity was detected. We therefore suggest that MPTA of at least 95° can prevent the recurrent varus deformity after MOWHTO.
In clinical applications, the assessment of MPTA is a simple method and its value of at least 95° provides the minimum point of correction to prevent recurrent varus deformity in MOWHTO. Nevertheless, the actual correction angle should be calculated following the recommendations that were reported in previous studies.5,6,17 Theoretically, all recommendations of overcorrection point in high tibial osteotomy require long radiographs, which are not technically possible in the operating room. Several techniques, including the cable method or grids with lead impregnated reference lines, were established to solve this problem.15,18 But the axis deviation could still arise from the movement of landmark points or image intensifier motion.7,19,20 In this study, we proved that the accuracy of MPTA measurement obtained from 15 cm proximal tibial length films was found to be comparable to that obtained from standard long films. This result could be applied to use during HTO. With the image intensifier continuously centered on the knee joint, at least 15 cm of proximal length and exact rotational control were achieved; this approach provided intraoperative realtime control of the osteotomy correction and the minimum of overcorrection point was the MPTA of 95°. Additionally, the MPTA could be used to detect the change in correction angle in a followup period.
There are several limitations in this study. First, we only focused on the amount of correction angle, but other factors (such as bone quality, type and technique of fixation) may relate to the degree and direction of osteotomy collapse. MOWHTO with fixed-angle plates is our recommended technique. It provides adequate stability and a satisfactory union rate without augmentation with bone grafts or bone substitutes.2,21–23 Second, due to the retrospective design, incomplete data and lack of ideal radiographs with exact rotational control were inevitable. Finally, theoretically, the adequacy of proximal tibial length in short films should be compared to the total tibial lengths or heights of the patients. We used the fixed 15 cm and 10 cm proximal tibial length film because our standard cassette for knee radiograph was 30 cm length. Thus, the 15 cm of proximal tibial length film might not be appropriate for every patient. However, in our experience, individual proper length could be seen from the parallelism between medial and lateral inner cortices of proximal tibia in fluoroscopic image.
In conclusion, MPTA, which is simple to measure, can be used to determine the overcorrection point intraoperatively and to detect a loss of correction after surgery. For MOWHTO with fixed angle plate, this study demonstrates that postoperative MPTA can be used to predict the change in correction angle and that MPTA of at least 95° is necessary to prevent recurrent varus deformity, and thus the use of this angle is recommended.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop. 2010;34:155–60. doi: 10.1007/s00264-009-0889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008;90:1548–7. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]
- 3.Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–54. [PubMed] [Google Scholar]
- 4.Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;4:366–72. doi: 10.1016/j.arthro.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248–64. [PubMed] [Google Scholar]
- 6.Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 7.Kim SJ, Koh YG, Chun YM, Kim YC, Park YS, Sung CH. Medial opening wedge high-tibial osteotomy using a kinematic navigation system versus a conventional method: a 1-year retrospective, comparative study. Knee Surg Sports Traumatol Arthrosc. 2009;17:128–34. doi: 10.1007/s00167-008-0630-y. [DOI] [PubMed] [Google Scholar]
- 8.Paley D. Principles of deformity correction. Vol. 1. Berlin Heidelberg New York: Springer-Verlag; 2002. Realignment for mono-compartment osteoarthritis of the Knee; pp. 479–85. [Google Scholar]
- 9.Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. Clin Orthop Relat Res. 1989;246:250–9. [PubMed] [Google Scholar]
- 10.Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am. 2003;85A:469–74. [PubMed] [Google Scholar]
- 11.Dowd GS, Somayaji HS, Uthukuri M. High tibial osteotomy for medial compartment osteoarthritis. Knee. 2006;13:87–92. doi: 10.1016/j.knee.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am. 1984;66:1040–8. [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Apley AG, Solomon L. Apleys system of orthopaedics and fractures. 7th ed. Oxford: Butterworth and Heinemann; 1993. [Google Scholar]
- 15.Krettek C, Miclau T, Grun O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures. Technical note. Injury. 1998;29:29–39. doi: 10.1016/s0020-1383(98)95006-9. [DOI] [PubMed] [Google Scholar]
- 16.Pape D, Adam F, Rupp S, Seil R, Kohn D. Stability, bone healing and loss of correction after valgus realignment of the tibial head. A roentgen stereometry analysis. Orthopade. 2004;33:208–17. doi: 10.1007/s00132-003-0591-2. [DOI] [PubMed] [Google Scholar]
- 17.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–65. [PubMed] [Google Scholar]
- 18.Saleh M, Harriman P, Edwaeds DJ. A radiological method for producing precise limb alignment. J Bone Joint Surg Br. 1991;73:515–6. doi: 10.1302/0301-620X.73B3.1670463. [DOI] [PubMed] [Google Scholar]
- 19.Hankemeier S, Hufner T, Wang G, Kendoff D, Zheng G, Richter M, et al. Navigated intraoperative analysis of lower limb alignment. Arch Orthop Trauma Surg. 2005;125:531–5. doi: 10.1007/s00402-005-0038-9. [DOI] [PubMed] [Google Scholar]
- 20.Hankemeier S, Mommsen P, Krettek C, Jagodzinski M, Brand J, Meyer C, et al. Accuracy of high tibial osteotomy: comparison between open- and closed-wedge technique. Knee Surg Sports Traumatol Arthrosc. 2009;18:1328–33. doi: 10.1007/s00167-009-1020-9. [DOI] [PubMed] [Google Scholar]
- 21.Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia-early results in 92 cases. Injury. 2003;34:B55–62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 22.Lobenhoffer P, De Simoni C, Staubli AE. Open-wedge high-tibial osteotomy with rigid plate fixation. Tech Knee Surg. 2002;1:93–105. [Google Scholar]
- 23.Stoffel K, Stachowiak G, Kuster M. Open wedge high tibial osteotomy: biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin Biomech (Bristol, Avon) 2004;19:944–50. doi: 10.1016/j.clinbiomech.2004.06.007. [DOI] [PubMed] [Google Scholar]


