Abstract
Background
THA in patients younger than 30 years presents challenges because of uncertainties regarding the long-term survivorship of prostheses. Alumina-on-alumina bearings, which exhibit little long-term wear, may be a reasonable option but the long-term survivorship is unknown.
Questions/Purposes
We determined (1) the survival rate of alumina-on-alumina bearings in patients younger than 30 years after a 10-year followup, (2) the incidence of audible hip clicking and squeaking, (3) radiographic evidence of osteolysis, and (4) the effects on pregnancy, childbirth, and career choice.
Methods
We retrospectively reviewed 62 patients who had 75 THAs with alumina-on-alumina bearings followed more than 10 years (average, 11.5; range, 10–13.5 years). Mean patient age at the time of surgery was 24 years (range, 18–30 years). All operations were performed using the same cementless implant at a single center. We determined survival, presence of osteolysis, and function (Harris hip score, WOMAC).
Results
The 10-year survival rate of alumina-on-alumina bearings in THAs, with revision for any reason as the end point, was 98.9%. Audible hip clicking and squeaking were identified in 10 hips and two hips, respectively. No osteolysis was detected. None of the 11 patients who became pregnant had been affected by their THA during pregnancy or childbirth. Seven of the 14 patients who were unemployed at the time of index surgery stated that their THA affected their job choice.
Conclusions
We found a high 10-year survival of cementless alumina-on-alumina bearings in THAs in patients younger than 30 years. Lifetime events such as job choice, pregnancy, and childbirth should be considered when choosing THA for patients younger than 30 years.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Although the benefit of THA in young patients with debilitating hip disorders has been documented [5, 8], THA in this population historically has been associated with failure rates ranging from 14% to 45% at 10 to 25 years [13, 36, 37], which has caused many surgeons to be cautious when recommending THA in this patient population despite expected short-term relief of pain and improvements in function, quality of life, and overall health. Furthermore, despite improvements in the techniques and implants such as cementless components and the use of alternative bearing surfaces, including ceramic-on-ceramic surfaces, the risk of early failure remains a concern [42].
Alumina-on-alumina bearings, which exhibit little wear, were introduced as an option for young patients [11, 30]. These bearings are characterized by low surface roughness, high hardness for major scratch resistance, and high wettability [16]. The low wear rates of alumina-on-alumina bearings reportedly reduce osteolysis and preserve bone stock, both of which are important considerations in young patients who are expected to require revision surgery at some stage [10, 19]. However, early ceramic-on-ceramic implants were characterized by component fracture and by loosening of monoblock acetabular components with overall failure rates ranging from 4% to 27% at 2 to 11 years [14, 19, 25, 42]. Technologic advances in implant materials and fixation methods reduced the early failure rates to 0% to 9% at 4 to 8 years [10, 21, 30, 38, 42], although it is unclear whether they have increased the long-term survivorship of THAs in young, active patients.
Several reports describe alumina-on-alumina bearings used in THAs in young patients [1, 3, 19, 30], and report survivorship ranging from 91% to 99% at 7 to 11 years [10, 11, 21, 24]. We previously reported 5-year followup results of patients younger than 40 years [38], and 10-year followup results in a series of 100 patients [24]. One of these studies showed that survivorship of patients with mean age of 41 years was 99% at 10 years [24], but the data were not analyzed for patients younger than 30 years and for these patients followup of much longer than 10 years is important. Patients younger than 30 years expect to be in the workforce and lead normal active lives after THA, and female patients expect successful pregnancies and deliveries. In this regard, alumina-on-alumina ceramic bearings seem a reasonable option for young, active patients [11, 30]. Further, they are free of concerns regarding metal ions, which could cross the placental barrier [4, 41].
We therefore determined: (1) the survival rate of THA after 10 years in patients younger than 30 years; (2) the daily activity levels and the incidence of audible hip clicking and squeaking; (3) the proportions of hips showing radiographic evidence of osteolysis; and (4) whether THA affects pregnancy, delivery, and job choice.
Patients and Methods
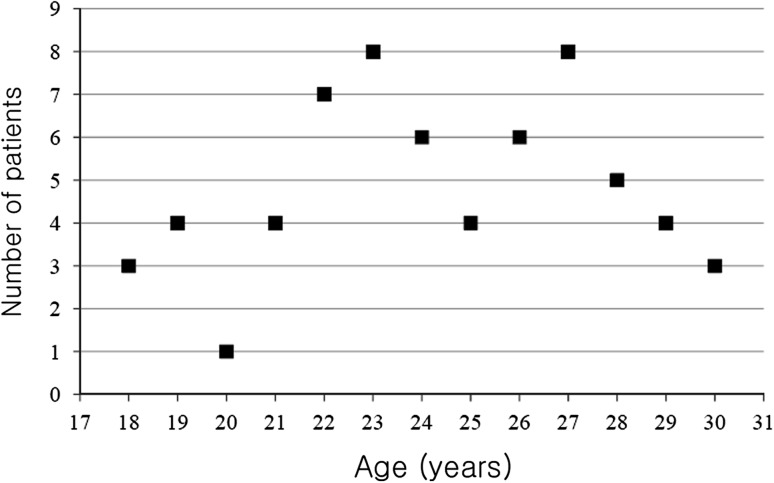
From November 1997 to December 2000, we performed 89 THAs using alumina-on-alumina bearings in 74 patients younger than 30 years. No other bearing combination was used in younger patients during this period. In two previous papers [24, 39], we reported 17 of the 74 patients included in this study. One patient (two hips) with ankylosing spondylitis died from end-stage renal disease during the seventh followup year, and 11 patients (12 hips) were lost to followup. This left 62 patients (75 hips or 84%), 37 men and 25 women, with a minimum followup of 10 years (average, 137 months; range, 120–161 months). Mean patient age at the time of index surgery was 24 years (range, 18–30 years), mean weight was 61 kg (range, 39–89 kg), and mean BMI was 22 kg/m2 (range, 16–32 kg/m2) (Fig. 1). The most common diagnosis was osteonecrosis of the femoral head in 38 hips (51%) (Table 1). Eighteen hips underwent at least one operation before THA (Table 2). Institutional review board approval was obtained for this study.
Fig. 1.
A scattergram shows patient age at the time of the index arthroplasty.
Table 1.
Initial diagnoses
| Initial diagnosis leading to THA | Number of hips (N = 75) |
|---|---|
| Osteonecrosis of the femoral head | 38 |
| Sequelae of hip infection | 17 |
| Primary coxarthrosis or coxarthrosis after hip dysplasia | 7 |
| Ankylosis of the hip | 5 |
| Sequelae of Legg-Calvé-Perthes disease | 4 |
| Miscellaneous conditions | 4 |
Table 2.
Previous operations
| Previous operations | Number of hips (N = 18) |
|---|---|
| Internal fixation for treatment of fracture | 5 |
| Septic hip arthrotomy | 4 |
| Decompression procedure for ONFH | 4 |
| Vascularized fibular bone graft for ONFH | 3 |
| Triple osteotomy | 2 |
ONFH = osteonecrosis of the femoral head.
All index arthroplasties were performed at one institution by one of two high-volume hip arthroplasty surgeons (YMK and HJK). A posterolateral approach was used in 43 hips, a lateral approach with trochanteric osteotomy in 16 hips, a lateral approach without trochanteric osteotomy in 13 hips, and an anterolateral approach in three hips. In all patients, THA involved a hemispheric titanium cup (Plasmacup® SC; Aesculap AG & Co, Tuttlingen, Germany) with an outer pure titanium plasma spray coating with a microporosity of 35% and a thickness of 0.35 mm (Plasmapore; Aesculap AG & Co), a slightly tapered, rectangular, collarless titanium femoral component in three types (Bicontact®; Aesculap AG & Co) with a Plasmapore-coated proximal one-third surface, a 28-mm modular alumina femoral head, and an alumina acetabular insert (BIOLOX® forte; CeramTec AG, Plochingen, Germany). The alumina liner had a 9.4835-degree cone angle and 11.7 to 13.1 mm cone clamp length. The cone diameter of the neck was 12/14 in 69 hips and 8/10 in six hips.
Partial weightbearing was allowed after 6 days, and full weightbearing was allowed after 8 to 10 weeks. No other specific physiotherapy was provided.
Followup was conducted at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and then yearly. Radiographs including AP and translateral views of the hips were performed at each followup. Clinical evaluations included a physical examination, Harris hip score [17], WOMAC score [2], and administration of a questionnaire (Appendix 1) on functional topics related to THA such as job choice, pregnancy, and childbirth. Patient activity levels were rated using a modified version of the UCLA Activity Level Scale [40] and Devane activity level scale [6]. A questionnaire that included items regarding any noise during daily activity (the presence of noise; the nature, time of onset, and frequency of the noise and activities associated with the noise; awareness of the noise by other people; intensity of the noise with time; associated pain; and effect of the noise on the quality of life) was completed.
Radiographs were reviewed at last followup by two independent observers (KSY and KHK) with respect to component stability [9], radiolucent lines [39], calcar resorption [34], osteolysis [20], and loosening [26]. Osteolysis was defined as a periprosthetic cystic or scalloped lesion with a diameter exceeding 2 mm that had not been present on the immediate postoperative radiographs [20].
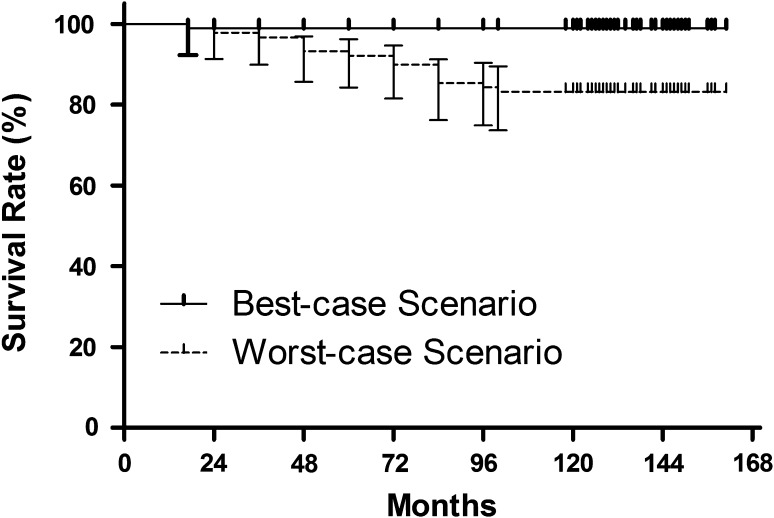
Kaplan-Meier survival analysis was performed to estimate survival in patients including those who were lost to followup. We performed two analyses; a best-case scenario with patients lost to followup as censored cases, and a worst-case scenario with patients lost to followup as having failed cases. Statistical analyses were conducted using SPSS for Windows (version 16.0; SPSS, Chicago, IL, USA).
Results
The 10-year survival rate of alumina-on-alumina bearings in THAs, with revisions of any implant for any reason as the end point, was 98.9% (95% CI, 96.7%–100%) in the best-case scenario and 83.1 % (95% CI, 75.3%–91.0%) in the worst-case scenario (Fig. 2). All THAs, excluding one with a ceramic liner fracture 17 months after surgery, had survival extending more than 10 years. No implant was revised as a result of wear or osteolysis.
Fig. 2.
The Kaplan-Meier survival curve with revision for any reason as the end point is shown.
The mean preoperative Harris hip score was 59 points (range, 40–83 points) and this improved to 97 points (range, 93–100 points) at last followup. Mean WOMAC score at last followup was 13 points (range, 0–28 points). Sixty patients (97%) were able to participate regularly in moderate activities such as housework, shopping, and daily routines. Thirty patients (48%) regularly participated in active sports such as cycling and swimming, and four patients (6%) sometimes participated in impact sports such as soccer. According to the activity level scale of Devane et al. [6], four patients were graded as being in Level 5, 43 were graded as being in Level 4, 13 were graded as being in Level 3, and two were graded as being in Level 2 in our series. The incidence of audible hip clicking and of squeaking at last followup were 13% (10 hips) and 3% (two hips), respectively. Hip noise was not associated with pain or any modification of daily activities in any patient. Furthermore, no patient could reproduce the squeaking, which was not of clinical importance in any patient.
All of the 75 hips showed radiographic evidence of osseointegration at last followup. No acetabular component or femoral stem showed radiographic signs of loosening. No periprosthetic osteolysis was detected around any cup or stem. Rounding off of the sharp medial edge of the resected femoral neck was a frequent finding, but no calcar resorption was observed in any hip (Fig. 3). Of the 25 female patients, 11 had a successful pregnancy without problems after THA. Sixteen infants were born, nine vaginally and seven by cesarean section. The reasons for cesarean delivery were obstetric in nature and not related to the THA. One patient changed his job from construction to an office job as a result of concerns of a hip problem. Seven of the 14 patients who were unemployed at the time of the index surgery said that their THA did affect their job choice; four chose office or secretarial work and three ran their own businesses.
Fig. 3A–C.
A 29-year-old man underwent cementless THA using an alumina-on-alumina bearing surface. (A) A preoperative AP radiograph shows femoral head osteonecrosis of both hips. (B) An AP radiograph was obtained immediate postoperatively. (C) The AP radiograph obtained 10.9 years postoperatively shows no radiolucent line or osteolysis around the acetabular or femoral components.
Ceramic fracture, which was associated with recurrent subluxation, occurred in one female patient. Preoperatively, she had an unstable hip as a result of inadequate hip muscle tone after spinal cord injury and also experienced constant instability of the hip after arthroplasty.
Discussion
The risk of early failure of THA in young patients remains a concern because of uncertainties regarding the long-term survivorship of prostheses. Alumina-on-alumina bearings, which exhibit little long-term wear, may be a favorable option for young patients. We therefore determined: (1) the survival rate of THA after 10 years in patients younger than 30 years; (2) the daily activity levels and the incidence of audible hip clicking and squeaking; (3) the proportions of hips showing radiographic evidence of osteolysis; and (4) whether THA affects pregnancy, delivery, and job choice.
There are a few limitations to our study. First, 11 patients (12 hips) were lost to followup, and the number of lost patients can influence the survival rate. However, we also provided a worst-case scenario with lost patients as failure cases. Second, we evaluated osteolysis on radiographs. CT scans would be more sensitive to identify the presence, location, and extent of osteolysis than standard radiographs [22, 32]. However, CT is costly and associated with a risk of radiation exposure. Third, the maximum BMI of the cohort was less than 32 kg/m2, limiting our ability to extend our conclusions to obese patients. Fourth, we had a small cohort. However, the indications for THA in very young patients are limited and any single-institution study will necessarily have a limited number of these patients. Fifth, this study was not a comparative one, therefore, we can draw no conclusions regarding the results of this implant compared with another implant in a similar group of patients.
We found the survivorship of implants with alumina-on-alumina bearings was 98.9% in the best-case scenario and 83.1 % in the worst-case scenario, at 10 years, which are similar to the survival rates reported for older patients [23, 28, 31]. Numerous reports have been published on alumina-on-alumina bearings in THAs in young patients (Table 3). The findings of our study suggest alumina-on-alumina bearings are associated with high implant survivorship after 10 years in young patients.
Table 3.
Results of reports of THAs with ceramic bearings
| Study | Age of patients in years (mean) | Number of hips (patients) | Mean followup (years) | Moderate activities possible (%) | Audible hip noise (%) | Osteolysis (%) | Survival rate |
|---|---|---|---|---|---|---|---|
| Hyder et al. [19] | < 30 (24) | 26 (22) | 6.5 | 96 | NR | NR | NR |
| Bizot et al. [3] | < 40 (32.3) | 88 (74) | 2 to 22* | NR | NR | 0 | 83.9% at 10 years |
| Yoo et al. [38] | < 40 (30) | 72 (61) | 5.8 | 97 | NR | 0 | NR |
| Murphy et al. [28] | < 76 (49.9) | 194 (173) | 4.3 | NR | NR | 0 | 96% at 9 years |
| Nizard et al. [30] | < 30 (23.4) | 132 (101) | 6.9 | NR | NR | 0.7 | 82.1% at 10 years |
| Kim et al. [21] | < 45 (38.2) | 93 (64) | 11.1 | 95 | 2 | 0 | 99% at 11.1 years |
| Park et al. [31] | < 66 (39) | 102 (90) | 9.6 | NR | 0 | 0 | 95.3% at 10 years |
| Kress et al. [23] | < 77 (58) | 75 (71) | 10.5 | NR | NR | 1 | 97% at 10 years |
| Finkbone et al. [10] | < 20 (16.4) | 24 (20) | 4.3 | NR | 0 | 0 | NR |
| Current study | < 30 (24) | 75 (62) | 11.5 | 97 | 16 | 0 | 98.9% at 10 years |
NR = not reported; * range of followup in years.
In one report, 20 of 21 patients could perform outdoor activities of daily living after THA using alumina-on-alumina bearings [19]. In another report, 97% of patients were able to participate regularly in moderate activities such as housework, shopping, and light occupational work [38] (Table 3). Similarly, in our study, most patients (97%) were able to participate regularly in moderate activities and nearly half of the patients (48%) can regularly participate in active sports. These findings support that use of alumina-on-alumina bearings in THAs can be an attractive option for young patients.
Noises such as squeaking and clicking are reported as annoying complications related to alumina-on-alumina bearings [21, 33]. The cause or causes of this phenomenon have not been determined and the incidence of squeaking has ranged from 0% to 18% among investigators [10, 21, 31, 33] (Table 3). We identified 12 hips (16%) with noises. Most (10 of 12 hips) had a clicking noise and none was associated with pain. Moreover, this noise was not reproducible during outpatient evaluations and had little effect on postoperative function. However, our findings suggest that patients should be informed of this problem when a THA with alumina-on-alumina bearings is considered.
Previous studies report an incidence of osteolytic lesions ranging from 0% to 46% at 10 to 22 years after THAs using alumina-on-alumina bearings [3, 18, 24, 29]. According to a 10-year followup study by Kim et al. [21], no osteolysis was observed in 93 hips of patients operated on when the patients were younger than 45 years, and this result was supported by CT scans. Similar results were reported by Baek and Kim [1]. In our study, no appreciable osteolysis was observed by plain radiography (Table 3).
THA and job choice appear related, and one patient changed his job because of concerns regarding hip problems. Furthermore, seven of 14 patients who were not employed at the time of index surgery stated they considered THA when choosing a job; four chose office jobs and three chose to run their own businesses.
Few authors have addressed the relation between THA and pregnancy [27, 35], although this issue is important when counseling young female patients. Sierra et al. [35] reported 60% of pregnant patients (28 of 47) experienced more hip pain during pregnancy and 21% (10 of 47) experienced persistent pain after pregnancy. In addition, five of seven patients who reported pain in the groin after childbirth underwent revision THA. However, in our series, no patients experienced persistent pain after childbirth and no revision was required as a result of pain. Although case numbers were small as compared with the study by Sierra et al. [35], none of our 11 patients reported that their THA had adversely affected pregnancy or childbirth.
The resistance to wear and osteolysis characteristics of THA with metal-on-metal implants also are compatible with the requirements of young, active patients [12]. However, concerns exist regarding elevated blood chrome and cobalt levels [41] because of the potential risks of mutagenicity and hypersensitivity [7] and possible teratogenic and chromosomal changes in developing fetuses [12]. These concerns are alleviated by THAs using ceramic implants, which is why they are considered suitable for young women of childbearing age.
During the last three decades, technical improvements in the alumina manufacturing process and improvements in conical fixation have substantially reduced ceramic fracture rates [15]. However, the possibility of ceramic fracture still poses a challenge [16]. In the current study, one ceramic fracture occurred as a result of inadequate hip muscle tone after spinal cord injury, and after experience of this failure, we no longer use alumina-on-alumina articulation in patients at risk of repetitive subluxation and relocation. Therefore, we suggest THAs using alumina-on-alumina implants only be performed after careful preoperative evaluation.
We found a survival rate of 98.9% at 10 years after surgery in active patients younger than 30 years. Our observations support the continued use of ceramic bearing surfaces in young adults. Nonetheless, our findings also suggest surgeons should be aware of the potential risks of impingement, ceramic fracture, and noise associated with the use of alumina-on-alumina articulation. In addition, our observations show lifetime events including job choice, pregnancy, and childbirth should be considered when choosing THA for patients younger than 30 years. Continued followup during the next decade will add to our knowledge of the value of alumina-on-alumina implants in THAs in young adult patients.
Acknowledgments
We thank Young-Min Kim MD for performing the index arthroplasties in some of the subjects included in this study.
Appendix 1. Patient Followup Questionnaire
Regarding occupation
-
What was your occupation before THA?
Student ( )
Housewife ( )
Sales, marketing, or service worker ( )
Factory worker ( )
Farmer, fisherman, or construction worker ( )
Other ( )
Did you change your job after THA? (YES/NO)
-
If you changed your job, what occupation did you choose after THA.
Student ( )
Housewife ( )
Sales, marketing, or service worker ( )
Factory worker ( )
Farmer, fisherman, or construction worker ( )
Other ( )
-
When did you change your occupation?
( ) month(s) or ( ) year(s) after THA
What was the main reason for the change of occupation? Was it because of the THA you underwent?
Regarding delivery
The questions below are required only for female patients.
Did you have a baby or babies after your THA? (YES/NO)
How many babies did you have? ( )
What kind of method was used for delivery? (vaginal delivery/cesarean section)
If you chose cesarean section, did you choose it because of possible difficulties that could be incurred by the THA? (YES/NO)
Did your pain reoccur around hip area after delivery? (YES/NO)
Footnotes
The institution one or more of the authors (JJY and HJK) received funding from the Ministry of Knowledge Economy of Korea (Grant no. 10030019-2010-21) and the Seoul National University Hospital Research Fund (Grant no. 06-03-063).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at Seoul National University College of Medicine, Seoul, South Korea.
References
- 1.Baek SH, Kim SY. Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Joint Surg Am. 2008;90:1314–1320. doi: 10.2106/JBJS.G.00755. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 3.Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-alumina total hip prostheses in patients 40 years of age or younger. Clin Orthop Relat Res. 2000;379:68–76. doi: 10.1097/00003086-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Brodner W, Grohs JG, Bancher-Todesca D, Dorotka R, Meisinger V, Gottsauner-Wolf F, Kotz R. Does the placenta inhibit the passage of chromium and cobalt after metal-on-metal total hip arthroplasty? J Arthroplasty. 2004;19(8 suppl 3):102–106. doi: 10.1016/j.arth.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old: a five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426–1434. [PubMed] [Google Scholar]
- 6.Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis: factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–266. doi: 10.1016/S0883-5403(97)90021-8. [DOI] [PubMed] [Google Scholar]
- 7.Domingo JL. Metal-induced developmental toxicity in mammals: a review. J Toxicol Environ Health. 1994;42:123–141. doi: 10.1080/15287399409531868. [DOI] [PubMed] [Google Scholar]
- 8.Dudkiewicz I, Salai M, Ganel A, Blankstein A, Chechik A. Total hip arthroplasty in patients younger than 30 years of age following developmental dysplasia of hip (DDH) in infancy. Arch Orthop Trauma Surg. 2002;122:139–142. doi: 10.1007/s004020100307. [DOI] [PubMed] [Google Scholar]
- 9.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 10.Finkbone PR, Severson EP, Cabanela ME, Trousdale RT. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty. 2012;27:213–219. doi: 10.1016/j.arth.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Rey E, Cruz-Pardos A, Garcia-Cimbrelo E. Alumina-on-alumina total hip arthroplasty in young patients: diagnosis is more important than age. Clin Orthop Relat Res. 2009;467:2281–2289. doi: 10.1007/s11999-009-0904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Girard J, Bocquet D, Autissier G, Fouilleron N, Fron D, Migaud H. Metal-on-metal hip arthroplasty in patients thirty years of age or younger. J Bone Joint Surg Am. 2010;92:2419–2426. doi: 10.2106/JBJS.I.01644. [DOI] [PubMed] [Google Scholar]
- 13.Halley DK, Wroblewski BM. Long-term results of low-friction arthroplasty in patients 30 years of age or younger. Clin Orthop Relat Res. 1986;211:43–50. [PubMed] [Google Scholar]
- 14.Hamadouche M, Boutin P, Daussange J, Bolander ME, Sedel L. Alumina-on-alumina total hip arthroplasty: a minimum 18.5-year follow-up study. J Bone Joint Surg Am. 2002;84:69–77. [PubMed] [Google Scholar]
- 15.Hannouche D, Nich C, Bizot P, Meunier A, Nizard R, Sedel L. Fractures of ceramic bearings: history and present status. Clin Orthop Relat Res. 2003;417:19–26. doi: 10.1097/01.blo.0000096806.78689.50. [DOI] [PubMed] [Google Scholar]
- 16.Hannouche D, Zaoui A, Zadegan F, Sedel L, Nizard R. Thirty years of experience with alumina-on-alumina bearings in total hip arthroplasty. Int Orthop. 2011;35:207–213. doi: 10.1007/s00264-010-1187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 18.Hernigou P, Zilber S, Filippini P, Poignard A. Ceramic-ceramic bearing decreases osteolysis: a 20-year study versus ceramic-polyethylene on the contralateral hip. Clin Orthop Relat Res. 2009;467:2274–2280. doi: 10.1007/s11999-009-0773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hyder N, Nevelos AB, Barabas TG. Cementless ceramic hip arthroplasties in patients less than 30 years old. J Arthroplasty. 1996;11:679–686. doi: 10.1016/S0883-5403(96)80006-4. [DOI] [PubMed] [Google Scholar]
- 20.Joshi RP, Eftekhar NS, McMahon DJ, Nercessian OA. Osteolysis after Charnley primary low-friction arthroplasty: a comparison of two matched paired groups. J Bone Joint Surg Br. 1998;80:585–590. doi: 10.1302/0301-620X.80B4.7361. [DOI] [PubMed] [Google Scholar]
- 21.Kim YH, Choi Y, Kim JS. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head osteonecrosis. Int Orthop. 2010;34:1123–1127. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kitamura N, Leung SB, Engh CA., Sr Characteristics of pelvic osteolysis on computed tomography after total hip arthroplasty. Clin Orthop Relat Res. 2005;441:291–297. doi: 10.1097/01.blo.0000192359.12573.15. [DOI] [PubMed] [Google Scholar]
- 23.Kress AM, Schmidt R, Holzwarth U, Forst R, Mueller LA. Excellent results with cementless total hip arthroplasty and alumina-on-alumina pairing: minimum ten-year follow-up. Int Orthop. 2011;35:195–200. doi: 10.1007/s00264-010-1150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010;92:1715–1719. doi: 10.2106/JBJS.I.01019. [DOI] [PubMed] [Google Scholar]
- 25.Mahoney OM, Dimon JH., 3rd Unsatisfactory results with a ceramic total hip prosthesis. J Bone Joint Surg Am. 1990;72:663–671. [PubMed] [Google Scholar]
- 26.Martell JM, Pierson RH, 3rd, Jacobs JJ, Rosenberg AG, Maley M, Galante JO. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg Am. 1993;75:554–571. doi: 10.2106/00004623-199304000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Meldrum R, Feinberg JR, Capello WN, Detterline AJ. Clinical outcome and incidence of pregnancy after bipolar and total hip arthroplasty in young women. J Arthroplasty. 2003;18:879–885. doi: 10.1016/S0883-5403(03)00270-5. [DOI] [PubMed] [Google Scholar]
- 28.Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102. doi: 10.1097/01.blo.0000246532.59876.73. [DOI] [PubMed] [Google Scholar]
- 29.Nam KW, Yoo JJ, Lae Kim Y, Kim YM, Lee MH, Kim KJ. Alumina-debris-induced osteolysis in contemporary alumina-on-alumina total hip arthroplasty: a case report. J Bone Joint Surg Am. 2007;89:2499–2503. doi: 10.2106/JBJS.G.00130. [DOI] [PubMed] [Google Scholar]
- 30.Nizard R, Pourreyron D, Raould A, Hannouche D, Sedel L. Alumina-on-alumina hip arthroplasty in patients younger than 30 years old. Clin Orthop Relat Res. 2008;466:317–323. doi: 10.1007/s11999-007-0068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park YS, Park SJ, Lim SJ. Ten-year results after cementless THA with a sandwich-type alumina ceramic bearing. Orthopedics. 2010;33:796. doi: 10.3928/01477447-20100924-11. [DOI] [PubMed] [Google Scholar]
- 32.Puri L, Wixson RL, Stern SH, Kohli J, Hendrix RW, Stulberg SD. Use of helical computed tomography for the assessment of acetabular osteolysis after total hip arthroplasty. J Bone Joint Surg Am. 2002;84:609–614. doi: 10.2106/00004623-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Restrepo C, Post ZD, Kai B, Hozack WJ. The effect of stem design on the prevalence of squeaking following ceramic-on-ceramic bearing total hip arthroplasty. J Bone Joint Surg Am. 2010;92:550–557. doi: 10.2106/JBJS.H.01326. [DOI] [PubMed] [Google Scholar]
- 34.Sarmiento A, Gruen TA. Radiographic analysis of a low-modulus titanium-alloy femoral total hip component: two to six-year follow-up. J Bone Joint Surg Am. 1985;67:48–56. [PubMed] [Google Scholar]
- 35.Sierra RJ, Trousdale RT, Cabanela ME. Pregnancy and childbirth after total hip arthroplasty. J Bone Joint Surg Br. 2005;87:21–24. doi: 10.1302/0301-620x.87b12.16914. [DOI] [PubMed] [Google Scholar]
- 36.Sochart DH, Porter ML. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty. 1998;13:123–131. doi: 10.1016/S0883-5403(98)90089-4. [DOI] [PubMed] [Google Scholar]
- 37.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old: long-term results. J Bone Joint Surg Am. 1996;78:995–1003. doi: 10.1302/0301-620X78B6.7170. [DOI] [PubMed] [Google Scholar]
- 38.Yoo JJ, Kim YM, Yoon KS, Koo KH, Kim JW, Nam KW, Kim HJ. Contemporary alumina-on-alumina total hip arthroplasty performed in patients younger than forty years: a 5-year minimum follow-up study. J Biomed Mater Res B Appl Biomater. 2006;78:70–75. doi: 10.1002/jbm.b.30457. [DOI] [PubMed] [Google Scholar]
- 39.Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87:530–535. doi: 10.2106/JBJS.D.01753. [DOI] [PubMed] [Google Scholar]
- 40.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 41.Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007;89:301–305. doi: 10.1302/0301-620X.89B3.18520. [DOI] [PubMed] [Google Scholar]
- 42.Zywiel MG, Sayeed SA, Johnson AJ, Schmalzried TP, Mont MA. Survival of hard-on-hard bearings in total hip arthroplasty: a systematic review. Clin Orthop Relat Res. 2011;469:1536–1546. doi: 10.1007/s11999-010-1658-0. [DOI] [PMC free article] [PubMed] [Google Scholar]