Abstract
Mental health problems are highly prevalent among individuals with HIV and are consistently associated with negative health outcomes. However, mental illness often remains untreated due to significant psychosocial and physical barriers to treatment participation. The Collaborative HIV/AIDS Mental Health Program (CHAMP) assessed the outcomes associated with providing 9 months of in-home mental health counseling for 40 individuals with HIV and a Major Axis I mental disorder. The evidence-based Illness Management and Recovery Model was adapted for use with HIV-positive individuals for the study using a community-based participatory research approach. Study participants were surveyed at baseline, 5 and 9 months to assess for changes in health outcomes. Thirty-five percent of study participants were female, 80% African American, 33% self-identified as MSM and the average participant age was 43. Forty percent of participants were on psychotropic medication at baseline. Participants had an average of 8 counseling visits (median 9). Statistically significant decreases in the global Brief Symptom Inventory (BSI) score and a number of BSI symptoms dimensions including anxiety, depression, obsessive compulsive, phobic anxiety and hostility were detected, indicating a reduction of psychiatric symptoms. Statistically significant improvement was also identified for the SF-12 mental health scale, adaptive coping, overall social support and emotional support. No differences in psychiatric outcomes were identified by gender, race/ethnicity, or sexual preference. Findings from the CHAMP Study suggest that the use of in-home mental health treatment may be beneficial in engaging and treating HIV-positive individuals with comorbid mental health disorders.
Introduction
Ahigh prevalence of mental illness has been consistently identified among HIV-infected individuals.1–5 Results from the HIV/AIDS Costs and Services Utilization Study (HCSUS), a national study of individuals receiving HIV care, found that nearly half (48%) of the study participants had a probable psychiatric disorder.1 Depression and other mood disorders, anxiety disorders, and posttraumatic stress disorder (PTSD) have been identified as the most prevalent diagnoses among HIV-infected individuals. Mental illness among individuals with HIV has been associated with negative outcomes including decreased quality of life,4,6–8 AIDS-related morbidity and mortality,9,10 delayed entry into medical care,5,11,12 poorer medication adherence,4,8,13–15 risky sexual and drug use behaviors12,16 and substantial costs including productivity loss and health care expenditures.10,17,18
Mental health treatment, including mental health counseling and psychopharmacologic treatment, has been associated with improvements in mental health functioning19–26 as well as greater HIV-related medication use and adherence10,19,27–31 and higher CD4 counts.24,32 Although some studies have found psychopharmacologic treatment to have benefit in improving psychiatric symptoms and medication use,27,31,32 one study found no association of psychopharmacologic treatment alone on HIV medication use.29 This study found that mental health counseling alone or in conjunction with psychopharmacologic treatment was associated with greater HIV medication utilization. Despite the benefit of mental health treatment, research data from HCSUS and other studies report that a substantial proportion of HIV-infected individuals with mental illness are not receiving mental health care.2,19,33–38 For example, a study of individuals with HIV initiating mental health counseling found that nearly 30% did not return after 1 session and only 37% completed 6 counseling sessions.37 Significant barriers to mental health treatment have been found for HIV-infected individuals including stigma, fear of discrimination,39–41 travel distance to care,37 and lack of education,34,42 transportation,43 insurance,33,34 service availability,44,45 and motivation.46
Offering mental health treatment in an individual's home or immediate community may reduce barriers that impede treatment entry and retention. Research regarding home-based mental health treatment for individuals with severe mental illness (SMI)47–49 and elderly individuals50 found that these interventions were beneficial in addressing psychiatric needs and improving health outcomes. However, research is lacking regarding the effects of providing in-home mental health services for nonelderly individuals and those with less severe mental health problems who experience barriers to utilizing traditional outpatient mental health services. One related study did find that providing motivational enhancement counseling and cognitive behavioral therapy (CBT) to individuals with substance abuse, some of whom were HIV positive, at a soup kitchen was associated with less substance use and greater participation in formal treatment and self-help groups.51
Innovative methods of treating the mental health needs of individuals with HIV that address the specific needs and barriers to care experienced by HIV-positive individuals are critically needed to improve utilization of mental health care and to reduce the negative health consequences of untreated mental illness in this population. Accordingly, we conducted a demonstration project to examine the feasibility and associated health outcomes of providing mental health treatment for individuals with HIV and mental health disorders in their home or place of their choosing in their community. The objectives of the program were to engage participants in mental health treatment, address immediate mental health needs, and prepare participants for ongoing mental health treatment in existing outpatient services as needed.
Methods
Sample
The Collaborative HIV/AIDS Mental Health Project (CHAMP) study examined the feasibility and outcomes associated with providing 9 months of in-home mental health treatment for individuals with HIV and a mental disorder. CHAMP was a pilot study designed to enroll 40 participants. Study participants were recruited from Infectious Diseases clinics, HIV case management providers, and other social services providers in Charlotte, North Carolina over a 7-month period in 2010.
Study criteria included being HIV-positive and having a Major Axis I disorder, which included major depressive disorder, dysthymia, bipolar disorders, PTSD, generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, and psychotic disorders (not actively psychotic). The Mini-International Neuropsychiatric Interview (MINI)52 was used to make probable mental disorder diagnoses and determine study eligibility.
Intervention
CHAMP was a Community Based Participatory Research (CBPR) project, which included a partnership with a local HIV/AIDS organization, Carolinas CARE Partnership, and extensive community involvement and guidance from two community advisory boards and multiple community forums. The community partners were involved in adapting the evidence-based Illness Management and Recovery (IMR) treatment model for use with HIV-positive individuals.53 The IMR model is based on the principles of instilling hope for change, wellness skills building and client collaboration in treatment planning, and is organized into nine modules that are taught using educational, motivational, and cognitive-behavioral strategies. The revised IMR, titled HIV/AIDS Illness Management and Recovery (HAIMR), included revised versions of the IMR modules that were adapted to contain information about how HIV relates to the specific module topic and HIV-specific modules addressing HIV care and risk reduction developed for the CHAMP study (Table 1). Consistent with the tenets of the IMR model, the HAIMR model focuses on providing education, increasing motivation, and building skills for coping and positive change. The study counselors used CBT techniques, which have been consistently associated with positive outcomes for the diagnoses included in this study including PTSD, depression/bipolar disorder, anxiety disorders and schizophrenia.54–58
Table 1.
HIV/AIDS Illness Management and Recovery (HAIMR) Model Modules
| HAIMR module title | Content |
|---|---|
| Goal Setting | Identify treatment goals and plans for reaching goals |
| Stress Vulnerability Module | Presents the stress vulnerability model |
| Coping with Stress | Education and skills building for coping with stressful situations |
| Social Support | Education/skills building on increasing social support |
| Coping with Problems/Symptoms | Education, motivation, skills building on symptoms such as depression and insomnia |
| HIV Medications and Coping | Basic HIV information and information/skills building re HIV medications and adherence |
| HIV Risk Reduction | Information, skills on HIV transmission/prevention |
| Mental Health Diagnoses | Information about Depression, Bipolar, PTSD, Schizophrenia, and Anxiety |
| Medications | Information on psychotropic medications and decisions regarding these medications |
| Relapse Prevention | Information on identifying/coping with relapse symptoms |
| Substance Use | Information on addiction, recovery and risk reduction |
| Getting Needs Met in the Health Care System | Information and skills building on navigating health care systems |
PTSD, posttraumatic stress disorder.
Mental health counseling was provided by licensed professional counselors and psychologists with experience in providing care for individuals with HIV and mental disorders. The counselors met monthly and documented their counseling activities to monitor and enhance consistency between counseling providers. The mental health treatment program began with engagement, goal setting, and planning using the HAIMR goal-setting module. Subsequent treatment sessions covered other treatment modules and included continued work on participant goals. The treatment program and specific modules used were tailored to address each participant's specific mental health needs and diagnoses. However, most participants completed the social support, psychiatric illnesses, goal setting, and HIV specific modules. Treatment participants also met with a study case coordinator at least quarterly for assistance with resources, such as HIV case management and housing, as needed.
Measures
Study participants were surveyed at baseline, 5 months (treatment midpoint), and 9 months (after treatment completion) using computer-assisted interviews.
Psychiatric symptoms were measured by the Brief Symptom Inventory (BSI)59 and the SF-12 mental health index.60 The BSI is designed to reflect psychological distress and symptom patterns and contains 9 subscales measuring items such as depression, anxiety, hostility, and paranoid ideation.61 The Medical Outcome Study (MOS) Social Support Scale62 was used to measure social support. Stigma was measured using the HIV Stigma Scale63 and coping styles were assessed with the Brief COPE.64 Components of the Client Motivation for Therapy Scale were used to examine types of motivation to participate in mental health treatment.65 These scale components measure a continuum of motivation types from more internal motivation to amotivation (lack of motivation) for treatment. The surveys also included questions ascertaining demographic information, traumatic events,66,67 medication adherence,68 substance use,69 and perceptions of the treatment program.
Statistical analysis
Descriptive statistics were used to provide information on participant characteristics, mental health, social support, and coping at baseline, 5, and 9 months. Bivariate and multivariate analyses were used to examine changes in psychiatric symptoms, social support, coping, and motivation for mental health treatment. These analyses used linear mixed models, an analytic method appropriate for use with longitudinal, repeat-observation data to account for the dependency between multiple observations on the same individuals.70 We used multivariable regression models to test whether psychiatric outcomes differed by demographic characteristics, illicit substance use or taking psychotropic medications at baseline.
Results
Of the 40 individuals initially recruited for the study, 2 were deemed ineligible due to active psychosis and were referred to more intensive treatment and 3 signed consent forms but were lost to follow-up before the baseline interview. Five additional subjects were recruited for a total of 40 individuals who completed the baseline interview. Just over one third of the CHAMP study participants were female and 80% were African American. One third of participants identified as MSM (Table 2). Forty percent of study participants were covered by Medicaid but the majority of participants (55%) had no commercial or governmental health insurance. The case coordinator worked with individuals to secure Medicaid if eligible. However, in the study location eligibility is tied to social security disability or having a dependent child in the home, making some participants ineligible for Medicaid.
Table 2.
Baseline Characteristics of CHAMP Participants (n=40)
| Demographic characteristics | |
| Female | 35% |
| African American | 80% |
| Caucasian | 20% |
| Age | |
| Under 30 | 10% |
| 30–39 | 28% |
| 40–49 | 40% |
| 50–60 | 22% |
| Less than high school education | 28% |
| Identify as MSM | 33% |
| Illicit substance use in the last 4 months | 35% |
| Alcohol intoxication in last 30 days | 15% |
| Disabled | 28% |
| Unstable housing sometime in last 4 monthsa | 35% |
| Insurance | |
| Medicaid primary | 22% |
| Medicare | 23% |
| No insurance | 55% |
| Probable mental disorders | |
| Bipolar | 30% |
| Depression | 55% |
| Anxiety | 33% |
| PTSD | 38% |
| Trauma | |
| Ever seen someone seriously injured/killed | 60% |
| Had spouse/partner or child die | 50% |
| Sexual abuse | 45% |
| Physical abuse (with or without weapon) | 68% |
| On HIV medications | 85% |
| On psychotropic medications | 40% |
| Social support | |
| Someone to listen when you need to talkb | 43% |
| Someone to help you if you were confined to bedb | 59% |
| Stigma | |
| “Feel I'm not as good a person as others because I have HIV”c | 35% |
| “People I know believe that someone with HIV is dirty”c | 64% |
Defined as having been in a shelter, temporarily doubled up in someone else's home, on the street, or in emergency/transitional housing for at least one night in the last 4 months.
Response category was “most or all the time.”
Response category was “Agree” or “Strongly Agree.”
CHAMP, Collaborative HIV/AIDS Mental Health Program; MSM, men who have sex with men; PTSD, posttraumatic stress disorder.
Lack of emotional support was common among study participants, as 58% reported not consistently having “someone to listen when I need to talk.” Perceptions of stigma were also high, as 35% reported that they “Feel I'm not as good a person as others because I have HIV” and over half reported that “People I know believe that someone with HIV is dirty.” Study participants also reported a high level of previous traumatic experiences. For example, 50% reported having experienced the death of a significant other or child and 45% had experienced sexual abuse at some point in their lives.
Findings from the MINI indicated that 55% of participants had a probable depressive disorder, 30% a bipolar disorder, and 38% had PTSD. Forty percent of participants were on psychotropic medications at baseline. Only 17.5% had seen a psychiatrist in the last 4 months for medications or treatment.
Treatment participants received an average of 8 visits from the mental health counselor (median 9; range, 0–12) during the 9 months of treatment. Most participants (77%) received at least 6 counseling visits. The vast majority of treatment visits were conducted in the participants' home; however, for the 15% of clients (n=6) with unstable housing or concerns about privacy in their home, the counselor met them at a place of their choosing in their immediate community such as a library or park. Study participants who were homeless were seen at a local homeless shelter. The six participants who routinely received counseling outside the home were similar to the other participants in terms of race, gender, and psychiatric symptom severity; however, the majority were homeless or unstably housed. Two participants were concerned about privacy in the home so preferred to meet in a park or library. Although the number of individuals receiving mental health counseling in their immediate community rather than their home was too small to analyze for differences in outcomes, no substantial outcome differences were noted by study staff.
Feedback from participant surveys was uniformly positive regarding in-home counseling as a treatment modality and most of the participants indicated that they would not have participated in counseling in an outpatient setting due to lack of comfort with mental health care, stigma concerns, and other treatment barriers.
Changes from baseline to 9-month follow-up and entry into existing mental health treatment
Ninety percent of CHAMP participants completed the survey at 5 months and 85% completed the survey conducted at treatment completion. Data from interviews conducted after completion of the 9-month treatment duration (n=34; 85% of CHAMP participants) showed statistically significant decreases in a number of BSI symptom dimensions including anxiety, depression, obsessive compulsive, phobic anxiety, and hostility as well as a decrease in the global BSI score (Table 3). BSI scale effect sizes included Cohen's d=0.52 for depression and 0.64 for the global symptom index, which are considered moderate to strong effects.71 Although the decreases in BSI scores were statistically significant, it is also important to examine the clinical significance of the declines in psychiatric symptoms. Two criteria have been established for categorizing an individual as positive for diagnosable psychopathology based on BSI adult, nonpatient norms: (1) a global BSI score of 63 or greater or (2) scores of 63 or greater on two or more subscales.72,73 At the 9-month follow-up survey, the proportion of participants meeting the BSI case definition of a probable mental disorder based on these two criteria decreased from 85% to 54% indicating a substantial decline in the number of individuals meeting a probable diagnostic threshold (p=0.018). The sample means for anxiety, hostility, and phobia dropped below the threshold score of 63 indicating that, on average, participants experienced substantive declines in these symptom areas. No differences in changes in psychiatric symptoms were detected by race, gender, sexual preference, illicit substance, use or being on psychotropic medications at baseline.
Table 3.
Collaborative HIV/AIDS Mental Health Project (CHAMP) Findings
| n=34, 85% retention at 9 months | Baseline | 9 Months |
|---|---|---|
| Mental health and coping | ||
| Brief Symptom Inventory (BSI) case definition (Global score of >62) | 85.0% | 55.0%a |
| BSI Scores—higher score indicates higher symptom levels | ||
| BSI Global Score | 71.5 | 65.7b |
| BSI Depression | 68.5 | 62.6b |
| BSI Anxiety | 65.8 | 57.6b |
| BSI Hostility | 64.5 | 57.5b |
| BSI Phobic Anxiety | 63.1 | 57.9b |
| BSI Obsessive Compulsive | 69.9 | 65.4b |
| BSI Paranoid Ideation | 68.6 | 65.4 |
| BSI Somatization | 65.2 | 62.1 |
| BSI Psychoticism | 69.4 | 64.9a |
| SF-12 Mental Health Scale (lower score indicates worse mental health) | 37.6 | 46.5b |
| Adaptive Coping | 2.9 | 3.2b |
| Social support | ||
| Overall social support index | 57.6 | 70.9b |
| Social/emotional support scale | 50.2 | 70.7b |
| Medications (self-report) | ||
| Missed HIV medication in last week | 29.0% | 24.0% |
| Missed HIV medication in last 24 h | 17.4% | 4.8% |
Methods include logistic and linear mixed models.
Indicates statistical significance at ap<0.05, bp<0.01.
Statistically significant improvement was also found for the SF-12 mental health scale, adaptive coping, overall social support and the emotional support subscale on the MOS social support scale. However, no statistically significant changes were found in tangible social support, which measures support of a more physical nature, such as providing meals if needed. Changes in motivation for treatment were also detected as scores for having external motivation and amotivation for mental health treatment significantly declined from baseline to 9-month follow-up survey. Although the proportion of individuals missing medication doses in the last week decreased from baseline to 9-month follow-up, this change was not statistically significant.
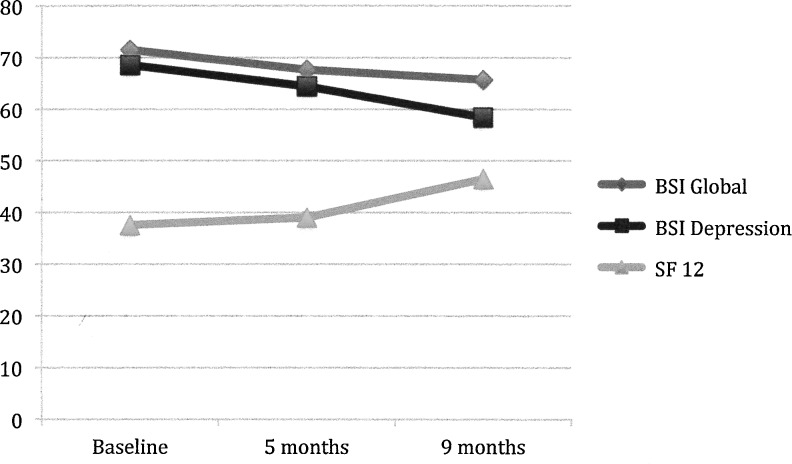
Although data from the participant interviews at 5 months showed statistically significant changes for the global BSI score, most BSI dimensions and the emotional social support score (results not shown), the magnitude of the improvements increased between 5 and 9 months (Fig. 1).
FIG. 1.
Mental health measure scores.
Participant data and information from referral sources indicated that 35% of participants transitioned to outpatient mental health counseling (n=14), which was defined as having at least one counseling visit after CHAMP completion. One participant entered a day psychosocial rehabilitation program. Of the remaining participants, 5 were lost to follow-up, 1 was deceased and the other 20 (50%) selected not to continue counseling after program completion but had a plan for counseling with a local provider if they chose to pursue treatment in the future.
Discussion
Findings from the evaluation of this demonstration project of in-home mental health counseling for individuals with HIV indicated that the study participants experienced statistically significant declines in psychiatric symptoms. In addition, the percentage of study participants who met the BSI diagnosis case definition declined from 85% to 54%. Study participants also experienced statistically significant improvement in adaptive coping and perceptions of social support, particularly emotional support.
Although the percentage of individuals reporting not taking their HIV medications decreased over time, this change was not statistically significant. Other studies examining the outcomes associated with mental health treatment have noted an improvement in medication adherence; however, these studies utilized more rigorous methods of measuring adherence and larger sample sizes than were possible for this feasibility study.28,32 A more comprehensive examination of HIV medication adherence would be needed to evaluate the effects of receiving in-home counseling on medication adherence. An examination of the effects of in-home mental health counseling on adherence would also need to be longer term as an influence of in-home mental health counseling on adherence may be subsequent, at least in part, to improvements in mental health functioning. In addition, the treatment intervention was relatively low-intensity with participants' receiving an average of 8 visits from the mental health counselor (median, 9) during the treatment period. Additional research would be beneficial to determine whether a more intensive intervention with a specific focus on adherence would be associated with greater increases in medication adherence.
The participants' perceptions of treatment provided in the home or immediate community were strongly positive and many participants indicated that they would likely not have entered mental health treatment outside of their home or immediate community. After participating in the study, the participants generally indicated a greater willingness to engage in outpatient counseling and a more complete understanding of mental health treatment options. A substantial minority of participants (35%) did continue counseling as an outpatient after completing the CHAMP program. A longer study that included follow-up several months after treatment completion would be beneficial in examining whether participants maintained the improvements noted after treatment completion and whether individuals not initially seeking outpatient counseling after treatment completion entered treatment at a later date if psychiatric symptoms worsened.
Although the outcomes of this demonstration study indicate that participants experienced positive changes after treatment participation, the study is limited by a number of methodological factors including a small sample size and lack of a control group. The relatively small sample size results in greater difficulty identifying meaningful changes in health outcomes after treatment participation. Not having a control group leaves the study open to threats to validity such as regression to the mean and social desirability bias.74,75 More rigorous study using a randomized control design is needed to further examine the utility of in-home mental health care in improving health outcomes for individuals with HIV. In addition, the lack of comprehensive measures of HIV-related outcomes in this pilot study including adherence, which only included two self-reported questions, and no objective measure of adherence, viral load or CD4 count results in difficulty measuring the impact of the intervention on these outcomes. However, psychiatric symptoms are strongly associated with the key HIV outcomes of medication adherence and HIV-related morbidity,4,8,10,14 thus improvements in psychiatric symptoms may result in downstream improvements in these outcomes.
The CHAMP pilot study has a number of strengths that contribute to its usefulness to the literature and future research, including use of a theoretically grounded adaptation of an evidence-based mental health treatment model, IMR, that was informed by a thorough and inclusive CBPR process. In addition, the study used existing and tested measures for critical outcomes of interest and had high retention rates in a population with multiple needs that is often challenging to maintain contact with.
Despite its limitations, the CHAMP pilot data provide support for the potential clinical benefit of an in-home mental health treatment approach. This approach can address many of the common barriers to outpatient mental health treatment for individuals with HIV including HIV and mental health-related stigma, transportation concerns and lack of motivation, and avoids the additional costs necessary to transport low-income individuals without consistent transportation to mental health treatment. Identification, testing, and implementation of innovative mental health treatment strategies, such as the CHAMP pilot, are critically needed to avoid the negative individual and community repercussions of mental illness among individuals with HIV.
Acknowledgments
The project described was supported by Award Number R21MH082686 from the National Institute Of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Mental Health or the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Galvan F. Burnam M. Bing E. Co-occurring psychiatric symptoms and drug dependence or heavy drinking among HIV-positive people. J Psychoactive Drugs. 2003;35(Supp 1):153–160. doi: 10.1080/02791072.2003.10400510. [DOI] [PubMed] [Google Scholar]
- 2.Bottonari K. Stepleman L. Improving access to mental health services via a clinic-wide mental health intervenion in a Southeastern US infectious disease clinic. AIDS Care. 2010;22:133–136. doi: 10.1080/09540120903038358. [DOI] [PubMed] [Google Scholar]
- 3.Grossman C. Gordon C. Mental health considerations in secondary HIV prevention. AIDS Behav. 2010;14:263–271. doi: 10.1007/s10461-008-9496-8. [DOI] [PubMed] [Google Scholar]
- 4.Pence B. Reif S. Whetten K, et al. Minorities, the poor, and survivors of abuse: HIV-infected patients in the US Deep South. South Med J. 2007;100:1114–1122. doi: 10.1097/01.smj.0000286756.54607.9f. [DOI] [PubMed] [Google Scholar]
- 5.Walkup J. Blank M. Gonzales J, et al. The impact of mental health and substance abuse factors on HIV prevention and treatment. J Acquir Immune Defic Syndr. 2008;47:S15–S19. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- 6.Sherbourne C. Hays R. Fleishman J. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry. 2000;57:248–254. doi: 10.1176/appi.ajp.157.2.248. [DOI] [PubMed] [Google Scholar]
- 7.Mosack K. Weinhardt L. Kelly J, et al. Influence of Coping, social support, and depression on subjective health statusamong HIV-positive adults with different sexual identities. Behav Med. 2009;34:133–144. doi: 10.3200/BMED.34.4.133-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohl M. Landon B. Cleary P. LeMaster J. Medical Clinic characteristics and access to behavioral health services for persons with HIV. Psychiatr Serv. 2008;59:400–407. doi: 10.1176/ps.2008.59.4.400. [DOI] [PubMed] [Google Scholar]
- 9.Ickovics J. Hamburger M. Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 10.Mkanta W. Mejia M. Duncan R. Race, Outpatient mental health service use and survival after an AIDS diagnosis in the highly active antiretroviral therapy era. AIDS Patient Care STDs. 2010;24:31–37. doi: 10.1089/apc.2009.0177. [DOI] [PubMed] [Google Scholar]
- 11.Andersen M. Tinsley J. Milfort D, et al. HIV health care access issues for women living with HIV, mental illness and substance abuse. AIDS Patient Care STDs. 2005;19:449–459. doi: 10.1089/apc.2005.19.449. [DOI] [PubMed] [Google Scholar]
- 12.Fairfield K. Libman J. Davis R. Eisenberg D. Phillips RS. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999;14:395–401. doi: 10.1046/j.1525-1497.1999.08198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartlett J. Addressing the challenges of adherence. J Acquir Immune Defic Syndr. 2002;29(Supp1):S2–10. doi: 10.1097/00126334-200202011-00002. [DOI] [PubMed] [Google Scholar]
- 14.Spire B. Duran S. Souville M, et al. Adherence to Highly Active Antiretroviral Therapies (HAART) in HIV-infected patients: From a predictive to a dynamic approach. Soc Sci Med. 2002;54:1481–1496. doi: 10.1016/s0277-9536(01)00125-3. [DOI] [PubMed] [Google Scholar]
- 15.Catz S. Kelly J. Bogart LM. Benotsch E. McAuliffe T. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19:124–133. [PubMed] [Google Scholar]
- 16.Avants S. Warburton L. Hawkins K. Margolin A. Continuation of high-risk behavior by HIV-positive drug users: treatment implications. J Subst Abuse Treat. 2000;19:15–22. doi: 10.1016/s0740-5472(99)00092-6. [DOI] [PubMed] [Google Scholar]
- 17.Dupont R. Rice D. Miller L. Shiraki S. Rowland C. Harwood H. Economic costs of anxiety disorders. Anxiety. 1996;2:167–172. doi: 10.1002/(SICI)1522-7154(1996)2:4<167::AID-ANXI2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.Rice D. Miller L. Health economics and cost implications of anxiety and other mental disorders in the United States. Br J Psychiatry. 1998;(Suppl 34):4–9. [PubMed] [Google Scholar]
- 19.Whetten K. Reif S. Ostermann J, et al. Improving health outcomes among individuals with HIV, mental illness, and substance use disorders in the Southeast. AIDS Care. 2006;18(Supp 1):18–26. doi: 10.1080/09540120600839330. [DOI] [PubMed] [Google Scholar]
- 20.Markowitz J. Kocsis J. Fishman B. Treatment of depressive symptoms in individual with human immunodeficiency virus. Arch Gen Psychiatry. 1998;55:452–457. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- 21.Brown JL. Vanable PA. Cognitive-behavioral stress management interventions for persons living with HIV: A review and critique of the literature. Ann Behav Med. 2008;35:26–40. doi: 10.1007/s12160-007-9010-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrando A. Wapenyi K. Psychopharmacological treatment of patients with HIV and AIDS. Psychiatr Q. 2002;73:33–49. doi: 10.1023/a:1012840717735. [DOI] [PubMed] [Google Scholar]
- 23.Scott-Sheldon LA. Kalichman SC. Carey MP. Fielder RL. Stress management interventions for HIV-positive adults: A meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychol. 2008;27:129–139. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crepaz N. Passin WF. Herbst JH. Rama SM. Malow RM. Purcell DW. Meta-analysis of cognitive behavioral interventions on HIV-positive persons' mental health and immune functioning. Health Psychol. 2008;27:4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- 25.Himelhoch S. Medoff D. Oyeniyi G. Efficacy of group psychotherapy to reduce depressive symptoms among HIV-infected individuals: A systematic review and meta-analysis. AIDS Patient Care STDs. 2007;21:732–739. doi: 10.1089/apc.2007.0012. [DOI] [PubMed] [Google Scholar]
- 26.Himelhoch S. Medoff D. Efficacy of antidepressant medication among HIV-positive individuals with depression: A systematic review and meta-analysis. AIDS Patient Care STDs. 2005;19:813–822. doi: 10.1089/apc.2005.19.813. [DOI] [PubMed] [Google Scholar]
- 27.Angelino A. Treisman G. Management of psychiatric disorders in patients infected with human immunodeficiency virus. Clin Infect Dis. 2001;33:847–856. doi: 10.1086/322679. [DOI] [PubMed] [Google Scholar]
- 28.Weber R. Christen L. Christen S, et al. Effect of individual cognitive behaviour intervention on adherence to antiretroviral therapy: Prospective randomized trial. Antivir Ther. 2004;9:85–95. [PubMed] [Google Scholar]
- 29.Cook J. Grey D. Burke-Miller J, et al. Effects of treated and untreated depressive symptoms on highly active antiretroviral therapy use in a US multi-site cohort of HIV-positive women. AIDS Care. 2006;18:93–100. doi: 10.1080/09540120500159284. [DOI] [PubMed] [Google Scholar]
- 30.Hartzell J. Igor E. Weintrob A. Impact of depression on HIV outcomes in the HAART eraa. J Antimicrob Chemother. 2008;62:246–255. doi: 10.1093/jac/dkn193. [DOI] [PubMed] [Google Scholar]
- 31.Walkup J. Wei W. Sambamoorthi U. Crystal S. Antidepressant treatment and adherence to combination antiretroviral therapy among patients with AIDS and diagnosed depression. Psychiatr Q. 2008;79:43–53. doi: 10.1007/s11126-007-9055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horberg M. Silverberg M. Hurley L, et al. Effects of depression and selective serotonic reuptake inhibitor use on adherence to highly active antiretorviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47:384–390. doi: 10.1097/QAI.0b013e318160d53e. [DOI] [PubMed] [Google Scholar]
- 33.Katz M. Douglas J. Bolan G, et al. Depression and use of mental health services among HIV-infected men. AIDS Care. 1996;8:433–442. doi: 10.1080/09540129650125623. [DOI] [PubMed] [Google Scholar]
- 34.Schuman P. Ohmit S. Moore J, et al. Perceived need for and use of mental health services by women living with or at risk of human immunodeficiency virus infection. J Am Med Womens Assoc. 2001;56:4–8. [PubMed] [Google Scholar]
- 35.Taylor S. Burnam M. Sherbourne C. Andersen R. Cunningham W. The relationship between type of mental health provider and met and unmet mental health needs in a nationally representative sample of HIV-positive patients. J Behav Health Serv Res. 2004;31:149–163. doi: 10.1007/BF02287378. [DOI] [PubMed] [Google Scholar]
- 36.Treissman G. Angelino A. Interrelation between psychiatric disorders and the prevention and treatment of HIV infection. Clin Infect Dis. 2007;45:S313–317. doi: 10.1086/522556. [DOI] [PubMed] [Google Scholar]
- 37.Bottonari K. Stepleman LM. Factors associated with psychotherapy longevity among HIV-positive patients. AIDS Patient Care STDs. 2009;23:109–118. doi: 10.1089/apc.2008.0081. [DOI] [PubMed] [Google Scholar]
- 38.Weaver M. Conover C. Proescholdbell R. Arno P. Ang A. Ettner S. Utilization of mental health and substance abuse care for people living with HIV/AIDS, chronic mental illness and substance abuse disorders. J Acquir Immune Defic Syndr. 2008;47:449–458. doi: 10.1097/QAI.0b013e3181642244. [DOI] [PubMed] [Google Scholar]
- 39.Reece M. HIV-related mental health care: Factors influencing dropout among low-income, HIV-positive individuals. AIDS Care. 2003;15:707–716. doi: 10.1080/09540120310001595195. [DOI] [PubMed] [Google Scholar]
- 40.Logie C. Gadalia T. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21:742–753. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 41.Sayles J. Wong M. Kinsler J. Martins D. Cunningham W. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24:1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burnam M. Bing E. Morton S, et al. Use of mental health and substance abuse treatment services among adults with HIV in the United States. Arch Gen Psychiatry. 2001;58:729–736. doi: 10.1001/archpsyc.58.8.729. [DOI] [PubMed] [Google Scholar]
- 43.Whetten R. Whetten K. Pence B. Reif S. Does distance affect utilization of substance abuse and mental health services in the presence of transportation services. AIDS Care. 2006;18:27–34. doi: 10.1080/09540120600839397. [DOI] [PubMed] [Google Scholar]
- 44.Scott KA. Nguyen TQ. Whetten K. If there's a will, is there a way?: Integrating HIV and mental health services in rural areas. AIDS Public Policy J. 2004;17:130–137. [Google Scholar]
- 45.Weissman G. Melchior L. Huba G, et al. Women living with substance abuse and HIV disease: Medical care access issues. J Am Med Womens Assoc. 1995;50:115–120. [PubMed] [Google Scholar]
- 46.Bouis S. Reif S. Whetten K. Scovil J. Murray A. Swartz M. An integrated, multidimensional treatment model for individuals living with HIV, mental illness and substance abuse. Health Soc Work. 2007;32:268–278. doi: 10.1093/hsw/32.4.268. [DOI] [PubMed] [Google Scholar]
- 47.Catty J. Burns T. Knapp M, et al. Home treatment for mental health problems: A systematic review. Psychol Med. 2002;32:383–401. doi: 10.1017/s0033291702005299. [DOI] [PubMed] [Google Scholar]
- 48.Morrissey J. Meyer P. Cuddeback G. Extending assertive community treatment to criminal justice settings: Origins, current evidence, and future directions. Community Ment Health J. 2007;43:527–544. doi: 10.1007/s10597-007-9092-9. [DOI] [PubMed] [Google Scholar]
- 49.The Lewin Group. Assertive Community Treatment Literature Review. 2000. www.wvmhpc.org/docs/13.ACT_Tips_PMHA_Pt2.pdf. [Jul;2012 ]. www.wvmhpc.org/docs/13.ACT_Tips_PMHA_Pt2.pdf
- 50.Bruce M. Van Citters A. Bartels S. Evidence-Based Mental Health Services for Home and Community. Psychiatr Clin North Am. 2005;28:1039–1060. doi: 10.1016/j.psc.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 51.DeLeon G. Sacks S. Staines G. McKendrick K. Modified therapeutic community for homeless mentally ill chemical abusers: Treatment outcomes. Am J Drug Alcohol Use. 2000;26:461–480. doi: 10.1081/ada-100100256. [DOI] [PubMed] [Google Scholar]
- 52.Sheehan D. Lecrubier Y. Sheehan K, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl):22–33. [PubMed] [Google Scholar]
- 53.SAMHSA. Evidence-Based Practices: Shaping Mental Health Services Toward Recovery. Illness Management and Recovery Workbook. 2007. http://mentalhealth.samhsa.gov/cmhs/communitysupport/toolkits/illness/workbook/default.asp. [Apr;2007 ]. http://mentalhealth.samhsa.gov/cmhs/communitysupport/toolkits/illness/workbook/default.asp
- 54.Foa E. Cognitive behavioral therapy of obsessive-compulsive disorder. Dialogues Clin Neurosci. 2010;12:199–207. doi: 10.31887/DCNS.2010.12.2/efoa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abramowitz J. Bartholomew D. Roche K. Cognitive-behavioral therapy for obsessive-compulsive disorder: A review of the treatment literature. Res Soc Work Pract. 2011;11:357–372. [Google Scholar]
- 56.Ham P. Waters D. Oliver M. Treatment of panic disorder. Am Fam Physician. 2005;71:733–739. [PubMed] [Google Scholar]
- 57.Solomon SD. Gerrity ET. Muff AM. Efficacy of treatments for posttraumatic stress disorder: An empirical review. JAMA. 1992;268:633–638. [PubMed] [Google Scholar]
- 58.Gabbard G. Gabbard's Treatments of Psychiatric Disorders. Fourth Edition. Washington, D.C.: American Psychiatric Press; 2007. [DOI] [PubMed] [Google Scholar]
- 59.Derogatis LR. Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 60.Hurst N. Ruta D. Kind P. Comparison of the MOS short form-12 (SF12) health status questionnaire with the SF36 in patients with rheumatoid arthritis. Rheumatology. 1998;37:862–869. doi: 10.1093/rheumatology/37.8.862. [DOI] [PubMed] [Google Scholar]
- 61.Derogatis L. BSI Brief Symptom Inventory. Bloomington MN: Pearson; 1993. [Google Scholar]
- 62.Sherbourne C. Stewart A. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 63.Bunn J. Solomon S. Miller C. Forehand R. Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19:198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- 64.Carver C. You want to measure coping but your protocol's too long: Consider the Brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 65.Pelletier L. Tuson K. Haddad N. Client Motivation for Therapy Scale: A measure of intrinsic motivation, extrinsic motivation, and motivation for therapy. J Subst Abuse. 1997;68:414–435. doi: 10.1207/s15327752jpa6802_11. [DOI] [PubMed] [Google Scholar]
- 66.Leserman J. Stressful life events and adherence in HIV. AIDS Patient Care STDs. 2008;22:403–411. doi: 10.1089/apc.2007.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sarason I. Johnson J. Siegel J. Assessing the impact of life changes: Development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- 68.Chesney M. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 69.McLellan A. Kushner H. Metzger D, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 70.Fitzmaurice GM. Laird NM. Ware JH. Wiley Series in Probability and Statistics. Hoboken, N.J.: John Wiley and Sons; 2004. Applied Longitudinal Analysis. [Google Scholar]
- 71.Ferguson C. An effect size primer: a guide for clinicians and researchers. Prof Psychol. 2009;40:532–538. [Google Scholar]
- 72.Derogatis L. Brief Symptoms Inventory (BSI): Administration, Scoring, and Procedures Manual. Minneapolis, MN: NCS Pearson Inc.; 1993. [Google Scholar]
- 73.Johnson M. Brems C. Mills M. Fisher D. Psychiatric Symptomatology among individuals receiving detoxification treatment. Addict Behav. 2007;32:1745–1752. doi: 10.1016/j.addbeh.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nederhof A. Methods of coping with social desiirability bias: A review. Eur J Soc Psychol. 1985;15:263–280. [Google Scholar]
- 75.Barnett A. van der Pols J. Dobson A. Regression to the mean: What it is and how to deal with it. Int J Epidemiol. 2004;34:215–220. doi: 10.1093/ije/dyh299. [DOI] [PubMed] [Google Scholar]